26 Jun 2025
Simultaneous high-risk PCI and TAVI with hemodynamic support: a stepwise approach using Impella CP SmartAssist
Supported by the EuroIntervention Journal
What’s the safest approach when surgical options are off the table? This real-life case shows how complex coronary revascularsation and TAVI were performed in a single session, supported by Impella.
Explore the rationale behind the sequence, the device choices, and the outcome in a high-risk patient with severe AS, distal left main disease, and PAD.
Authors
Michele Galasso1,2, Emanuela Tavasci2, Silvia Massaro2, Isidoro Pera2, Gianluca Tiberti2
- School of Medicine and Surgery, Milano-Bicocca University, Milan, Italy.
- Cardio-Thoraco-Vascular Department, Division of Cardiology, ASST Manzoni, Lecco, Italy.
Introduction
Managing patients with severe aortic stenosis (AS) and complex coronary artery disease (CAD) presents a clinical challenge, particularly in those deemed inoperable due to high surgical risk.
The optimal strategy for treating these patients remains debated1,2, especially in cases requiring both percutaneous coronary intervention (PCI) and transcatheter aortic valve implantation (TAVI).
Case Report
A 68-year-old male with a significant cardiovascular history, including hypertension, dyslipidemia, and active smoking, presented with worsening dyspnea and signs of acute decompensated heart failure (NYHA III). He had a previous history of acute coronary syndrome, though prior coronary angiography records were unavailable. His comorbidities included severe chronic obstructive pulmonary disease (COPD) and PAD. Upon admission, transthoracic echocardiography revealed severe AS with a mean transvalvular gradient of 43 mmHg and an LVEF of 40 %.
Coronary angiography was performed, revealing severe distal left main disease with critical involvement of the left anterior descending artery (LAD) and a chronic total occlusion of the dominant RCA (Supplementary Figure 1).
Given the complexity of the case, a multidisciplinary heart team discussion concluded that the patient was not a suitable candidate for surgical revascularisation or surgical aortic valve replacement due to his severe respiratory insufficiency and high procedural risk (EUROSCORE 4 %, STS score 3.4 %). Consequently, a percutaneous strategy was planned, integrating staged PCI and TAVI with hemodynamic support.
The procedure began with balloon aortic valvuloplasty using a TrueDilatation 18 × 45 mm balloon to improve transvalvular flow (Supplementary Figure 2).
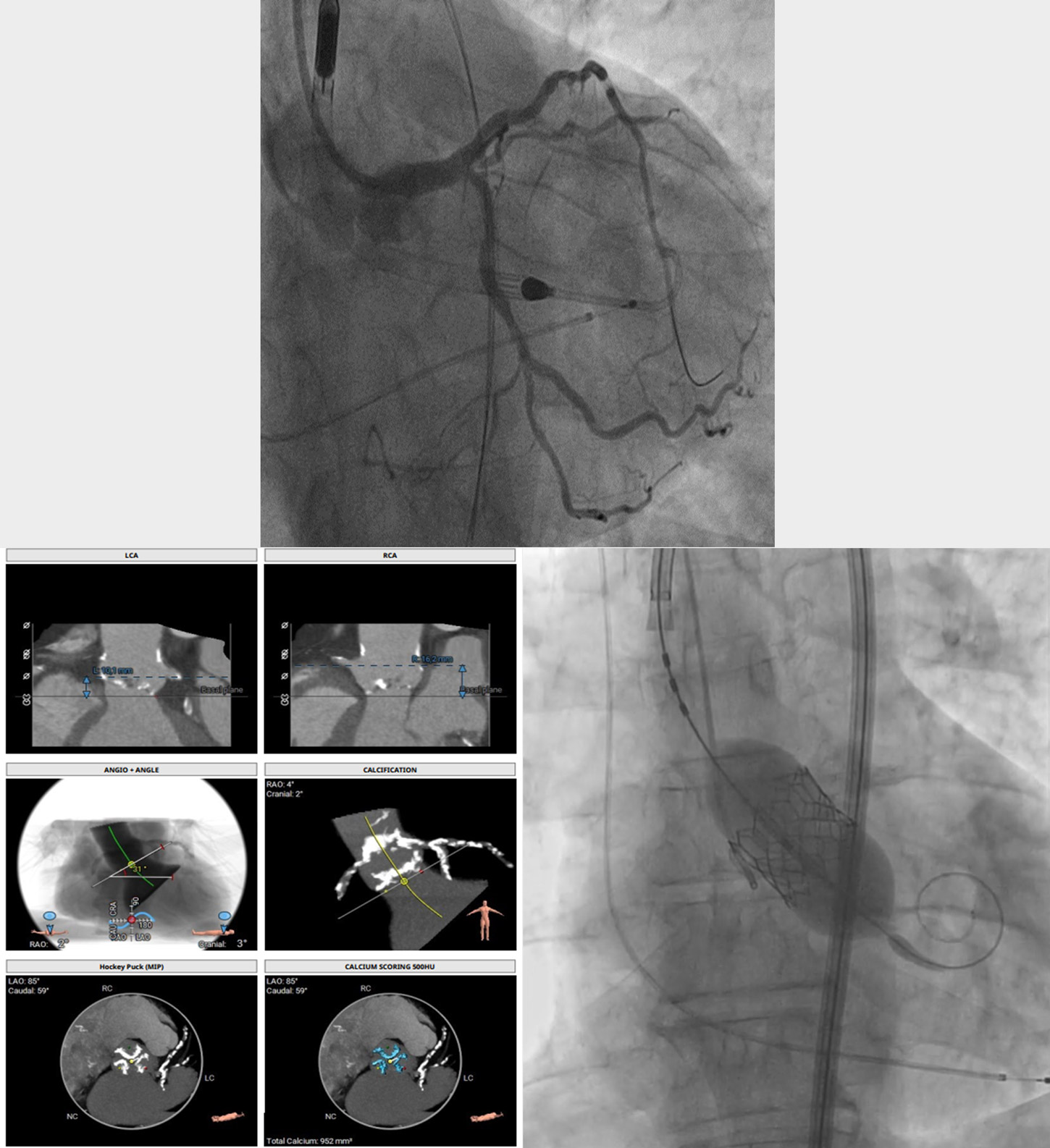
Following this, PCI of the left main and LAD was performed under Impella CP SmartAssist support via transfemoral access. Due to the severe calcification of the lesion, IVL with a Shockwave 4.0 × 12 mm balloon was used before deploying a drug-eluting stent (Synergy Megatron 4.0 × 24 mm) (Figure 1, Supplementary Video 1, 2).
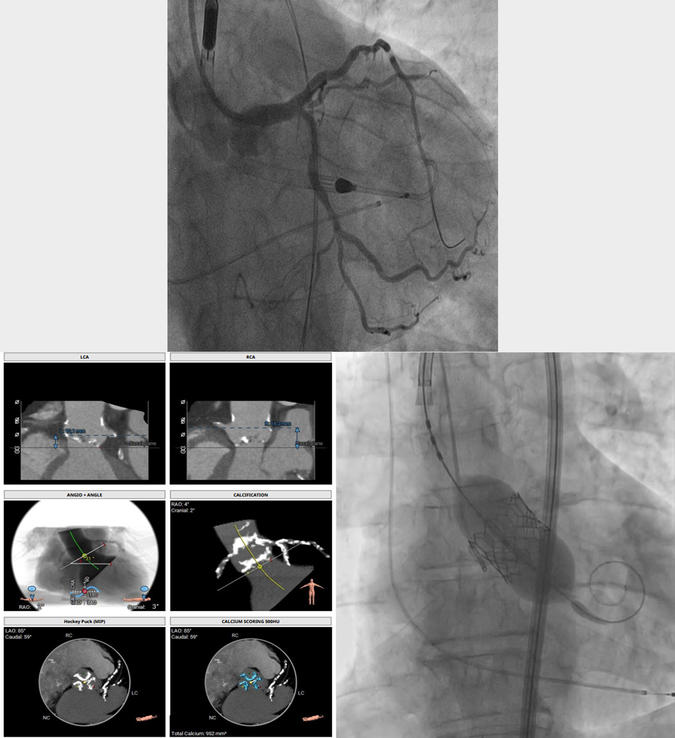
Main Figure 1: Comprehensive procedural summary illustrating the key phases of the intervention. The left panel shows the final angiographic result after complex PCI of the left main and LAD performed under Impella CP SmartAssist support. Successful deployment of a Synergy Megatron 4.0 × 24 mm drug-eluting stent is demonstrated, with optimal stent expansion confirmed by intravascular ultrasound (IVUS). The central panel displays the pre-TAVI computed tomography (CT) analysis, highlighting a suitable aortic annulus and favorable coronary ostia height, allowing for safe valve deployment while preserving future coronary access. The right panel shows the final angiographic result following successful transcatheter aortic valve implantation (TAVI) using a balloon-expandable Sapien 3 Ultra 26 mm valve. The valve is correctly positioned, with no significant paravalvular leak and unobstructed coronary ostia, ensuring excellent hemodynamic performance and future coronary reaccessibility.
After confirming optimal stent expansion with IVUS, the Impella device was removed, and attention shifted to the TAVI procedure.
Given the patient’s CAD burden, particularly the need for future coronary interventions, a balloon-expandable valve (Sapien 3 Ultra 26 mm) was chosen over a self-expanding prosthesis to ensure adequate coronary access post-implantation.
The TAVI was performed via femoral access under rapid pacing with a transjugular pacing wire at 180 bpm (Figure 1, Supplementary Video 3). Deployment was successful, with no significant paravalvular leak or hemodynamic instability.
Vascular closure was achieved with a Manta 18Fr closure device.
The patient remained hemodynamically stable throughout the procedure and was discharged in stable condition three days later. Follow-up echocardiography confirmed proper valve function with an LVEF of 42 %.
However, the day after the procedure, the patient was found smoking on the hospital balcony, against medical advice, emphasizing the challenges of long-term risk factor modification.
Discussion
Patients with concomitant severe CAD and AS represent a challenging subgroup requiring complex decision-making2,3. Traditionally, the approach to these patients has been debated: should PCI precede, follow, or be performed simultaneously with TAVI? In light of recent evidence, the decision to proceed with Impella-supported high-risk PCI prior to TAVI, rather than performing TAVI first, was based on both anatomical and clinical considerations. Immediate revascularisation of the critical left main disease was prioritised to reduce the risk of periprocedural hemodynamic collapse during TAVI. Additionally, pre-TAVI PCI allowed us to optimise myocardial perfusion and left ventricular function, thereby improving the patient’s hemodynamic reserve before valve replacement.
Current consensus2 and registries1 suggest that, in cases of complex coronary anatomy, particularly with left main involvement, addressing critical coronary lesions before TAVI can improve procedural safety and outcomes. Furthermore, the use of mechanical circulatory support with Impella provided hemodynamic stability during PCI, minimising the risk of ischemia-induced complications and enabling safe completion of the staged approach in a single session. This case exemplifies a strategy in which both interventions were performed in the same session under Impella-assisted hemodynamic support, reducing the cumulative procedural risk.
The decision to proceed with simultaneous PCI and TAVI was guided by several considerations3. First, the patient’s PAD made repeated large-bore femoral access potentially risky. Second, severe left main disease required immediate revascularisation, particularly given the possibility of hemodynamic collapse during TAVI if left untreated. Finally, mechanical circulatory support with the Impella CP SmartAssist provided stability throughout the procedure, allowing for complex intervention in a high-risk setting.
The selection of a balloon-expandable valve was driven by the need to maintain coronary access, particularly given the patient’s residual CAD burden. Balloon-expandable valves have been associated with easier coronary reaccess compared to self-expanding platforms, which may be critical for future interventions.
Conclusion
This case highlights the feasibility of performing high-risk PCI and TAVI in a single session under mechanical circulatory support. Careful procedural planning, device selection, and a multidisciplinary approach are crucial to achieving optimal outcomes in this high-risk population. Future studies should further explore the safety and efficacy of this combined approach in patients with severe CAD and AS.
Take-Home Messages
- Simultaneous high-risk PCI and TAVI with Impella support can be safely performed in selected patients.
- Device selection and procedural planning are critical in patients with severe CAD, AS, and PAD to optimise long-term outcomes.
Supplementary data
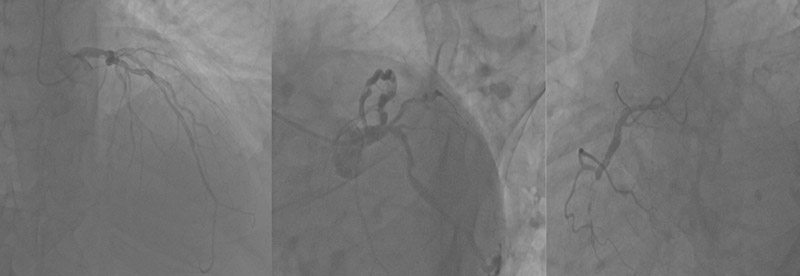
Supplementary Figure 1: Pre-procedural coronary angiography showing severe distal left main disease with critical involvement of the left anterior descending artery (LAD) and chronic total occlusion (CTO) of the dominant right coronary artery (RCA).
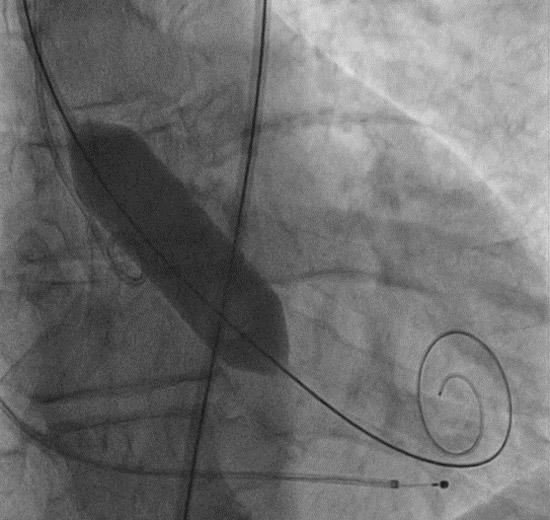
Supplementary Figure 2: Balloon aortic valvuloplasty performed with a TrueDilatation 18 × 45 mm balloon, prior to PCI and TAVI, to improve transvalvular flow and reduce procedural hemodynamic risk.
Bibliography
- Soriano F, Montalto C, Calderone D, Nava S, Esposito G, Saia F, Oreglia JA, Søndergaard L. Transcatheter treatment of severe aortic stenosis in patients with complex coronary artery disease: case series and proposed therapeutic algorithm. Eur Heart J Case Rep. 2022 Sep 26;6(10):ytac399. doi: 10.1093/ehjcr/ytac399. PMID: 36225807; PMCID: PMC9549596.
- Tarantini G, Tang G, Nai Fovino L, Blackman D, Van Mieghem NM, Kim WK, Karam N, Carrilho-Ferreira P, Fournier S, Pręgowski J, Fraccaro C, Vincent F, Campante Teles R, Mylotte D, Wong I, Bieliauskas G, Czerny M, Bonaros N, Parolari A, Dudek D, Tchetche D, Eltchaninoff H, de Backer O, Stefanini G, Sondergaard L. Management of coronary artery disease in patients undergoing transcatheter aortic valve implantation. A clinical consensus statement from the European Association of Percutaneous Cardiovascular Interventions in collaboration with the ESC Working Group on Cardiovascular Surgery. EuroIntervention. 2023 May 15;19(1):37-52. doi: 10.4244/EIJ-D-22-00958. PMID: 36811935; PMCID: PMC10174192.
- López Otero D, Ávila-Carrillo A, González Ferreiro R, Cid Menéndez A, Iglesias Álvarez D, Álvarez Rodríguez L, Antúnez Muiños P, Álvarez BC, Sanmartín Pena XC, Gómez Pérez F, Diéguez AR, Cruz-González I, Trillo Nouche R, González-Juanatey JR. Impact of Coronary Revascularization in Patients Who Underwent Transcatheter Aortic Valve Implantation. Am J Cardiol. 2019 Mar 15;123(6):948-955. doi: 10.1016/j.amjcard.2018.12.007. Epub 2018 Dec 19. PMID: 30598242.
Conflicts of interest
The authors do not have any disclosures or conflicts of interest.






1 comment
Great case and excellent execution with Impella support. In our recent case series (Eur Heart J Case Rep, 2025), we described an alternative approach — Simultaneous Cardioflow Optimisation (SCO) — integrating simultaneous left main PCI and BAV/TAVI without mechanical support. This stepwise strategy facilitates post-pacing hemodynamic recovery in selected high-risk patients with LM disease and severe AS. Both methods highlight valuable treatment options tailored to institutional capabilities and patient risk profiles. https://doi.org/10.1093/ehjcr/ytaf089