Key updates in valvular heart disease management: insights from the 2025 ESC/EACTS Guidelines
Reported from ESC Congress 2025
Alex Sticchi provides his take on the new ESC Valvular Guidelines presented at the ESC Congress 2025 in Madrid.
General overview
The 2025 ESC/EACTS Guidelines on Valvular Heart Disease represent a decisive step forward compared to the 2021 edition. They incorporate a wealth of randomized evidence and real-world data accumulated over the past years, and they reshape clinical practice by moving interventions earlier in the disease trajectory, expanding the role of transcatheter therapies, refining imaging and coronary work-up, and simplifying antithrombotic regimens. The result is a more proactive and patient-centered approach, anchored in multidisciplinary Heart Teams and Heart Valve Networks.
Aortic valve disease
In aortic stenosis, the new guidelines endorse earlier intervention, extending the indication even to asymptomatic patients with severe high-gradient AS and preserved LVEF, provided procedural risk is low. This is a clear departure from the “watchful waiting” approach and reflects evidence showing prognostic benefit of timely treatment. The choice of intervention is also redefined: TAVI is now recommended in patients aged ≥70 years, while SAVR remains standard in those under 70 at low surgical risk. Non-transfemoral TAVI is upgraded for those unsuitable for surgery and transfemoral access. For aortic regurgitation, a remarkable innovation is the possibility of TAVI in symptomatic inoperable patients with suitable anatomy—something unthinkable just a few years ago. Criteria for surgical intervention in asymptomatic AR have also been refined, with stricter LV dimension and function thresholds, and aortic valve repair is now more strongly encouraged at expert centres.
In aortic stenosis, the guidelines now endorse earlier intervention. Asymptomatic patients with severe high-gradient AS and preserved LVEF may undergo intervention if procedural risk is low, a departure from the previous 'watchful waiting' approach. Age thresholds have been refined: TAVI is recommended in patients ≥70 years, while SAVR remains standard in those <70 with low surgical risk. Non-transfemoral TAVI is upgraded as a valid option in patients unsuitable for both surgery and transfemoral access.
For aortic regurgitation, TAVI may now be considered in symptomatic inoperable patients with suitable anatomy, expanding transcatheter solutions beyond stenosis. Surgery remains the standard, but thresholds for intervention in asymptomatic patients have been clarified: LVESDi >22 mm/m², LVESVi >45 mL/m², or LVEF ≤55% may trigger surgery at low operative risk. Furthermore, aortic valve repair should be considered at expert centres when durable results are expected.
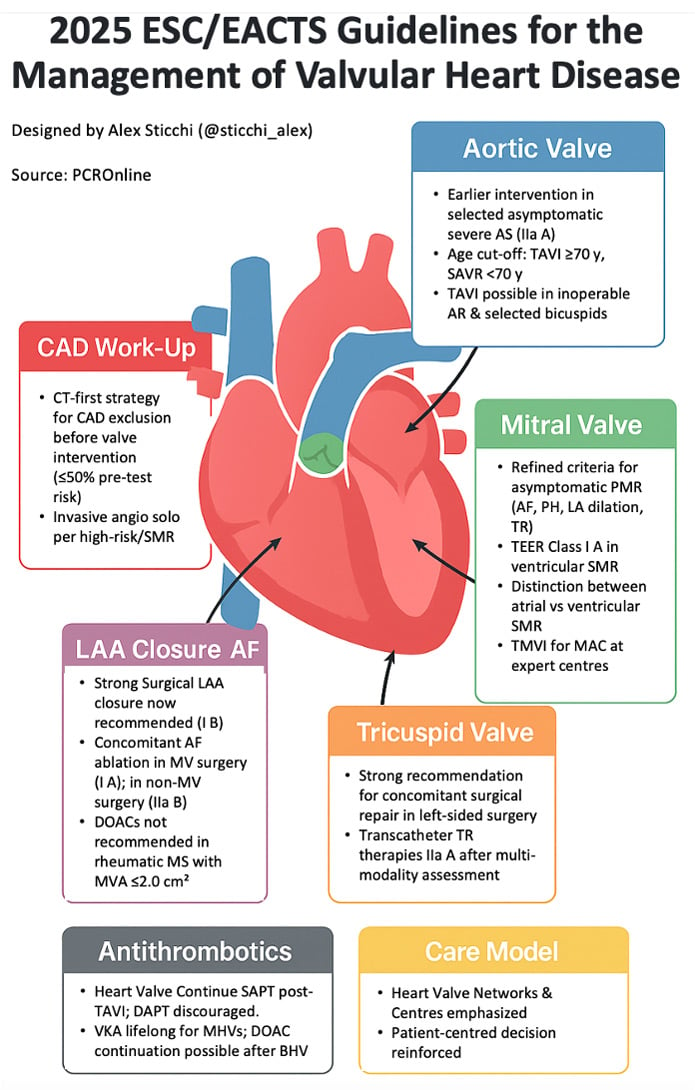
Courtesy of Alex Sticchi. Source: PCRonline.com
Mitral valve disease
For primary mitral regurgitation, surgical repair is recommended earlier in low-risk asymptomatic patients without LV dysfunction, provided at least three additional risk factors are present: atrial fibrillation, pulmonary hypertension, significant LA dilatation, or concomitant TR. Minimally invasive mitral surgery is acknowledged as a valuable approach in expert centres to shorten recovery. TEER has been upgraded to 'should be considered' in symptomatic high-surgical-risk patients with suitable anatomy.
For secondary MR, the guidelines introduce a clearer distinction between atrial and ventricular phenotypes. In atrial SMR, surgery with AF ablation and LAA occlusion is supported, while TEER may be considered in non-surgical candidates after optimization of medical and rhythm therapy. In ventricular SMR, the key change is the elevation of TEER to a Class I A recommendation for haemodynamically stable symptomatic patients with LVEF <50% and persistent severe regurgitation despite GDMT and CRT, fulfilling strict criteria. Surgery remains an option for selected patients unsuitable for TEER. For mitral stenosis, TMVI emerges as an alternative in patients with severe MAC and high surgical risk, provided procedures are performed in experienced Heart Valve Centres.
Tricuspid Valve Disease
Tricuspid valve disease receives unprecedented attention. A mandatory comprehensive Heart-Team evaluation is recommended before intervention. Concomitant tricuspid repair is strongly advised during left-sided surgery in cases of severe TR, and should be considered for moderate TR with annular dilatation ≥40 mm. Importantly, transcatheter therapies for TR are now formally endorsed: they should be considered in high-risk symptomatic patients without severe RV dysfunction or pre-capillary pulmonary hypertension, with evidence of symptomatic improvement and RV reverse remodelling.
Multivalvular and Mixed Disease
The guidelines clarify thresholds for intervention in patients with mixed lesions. In particular, patients with mixed moderate AS and AR should undergo intervention if symptomatic with mean gradient ≥40 mmHg or Vmax ≥4.0 m/s. In asymptomatic patients, intervention is recommended if Vmax ≥4.0 m/s with LVEF <50%. These criteria address a previously grey area in decision-making.
Prosthetic Valves and Antithrombotic Therapy
Mechanical valves remain the prosthesis of choice in patients with long life expectancy and no contraindications to lifelong anticoagulation. Lifelong VKA therapy is reaffirmed, with explicit INR targets individualized by valve type, position, and comorbidities. Patient education and INR self-monitoring/self-management are now strongly recommended. The addition of low-dose aspirin to VKA should be considered in selected patients with symptomatic atherosclerosis.
For transcatheter valves, antithrombotic management is simplified. After TAVI, single antiplatelet therapy (aspirin) is preferred; DAPT is not recommended unless otherwise indicated. DOACs remain contraindicated in mechanical valves and rheumatic MS, but may be continued in selected patients with bioprosthetic valves who already require them. TOE or 4D-CT is recommended in suspected prosthetic valve thrombosis, ensuring more accurate diagnosis and targeted therapy. Valve-in-valve procedures are endorsed for failed surgical or transcatheter valves in patients at intermediate or high surgical risk, across aortic, mitral, and tricuspid positions.
Imaging and Coronary Work-up
Imaging is central across all disease stages. A major novelty is the adoption of a CT-first approach in pre-intervention CAD assessment: CCTA is now recommended in patients with ≤50% pre-test likelihood of obstructive CAD, limiting invasive angiography to those with higher risk or specific conditions such as severe ventricular SMR. This strategy reflects improved accuracy of modern CT and reduces unnecessary invasive procedures. Multimodality imaging with TTE, TOE, CMR, and CCT is also recommended for comprehensive evaluation, procedural planning, and follow-up.
Models of Care and Patient-Centered Approach
The 2025 guidelines reinforce the role of Heart Valve Networks and Heart Valve Centres, highlighting the correlation between procedural volume and outcomes. High-volume centres are expected to manage complex interventions and support regional care pathways. The Heart Team remains central to decision-making, with emphasis on standardized protocols, PROMs, PREMs, and shared decision-making. This ensures that therapeutic strategies not only follow evidence but also align with patient expectations and preferences.
Clinical Impact Summary
Topic | Practice-Changing Update |
Aortic stenosis | Earlier intervention in asymptomatic severe AS; TAVI recommended ≥70 years (was ≥75). |
Aortic regurgitation | TAVI now possible in inoperable severe AR; stricter surgical thresholds; AV repair encouraged. |
Primary MR | Earlier repair in asymptomatic patients with risk factors; minimally invasive surgery recognized. |
Secondary MR | TEER Class I A in ventricular SMR; atrial SMR pathways formalized with surgery/TEER. |
Mitral stenosis (MAC) | TMVI introduced for high-risk severe MAC at expert centres. |
Tricuspid disease | Concomitant repair strengthened; transcatheter TR therapies formally endorsed (IIa A). |
Mixed lesions | Explicit thresholds for mixed moderate AS+AR (symptomatic and asymptomatic). |
CAD work-up | CCTA recommended in low-risk; invasive angiography reserved for high-risk or SMR cases. |
Prostheses / OAC | VKA lifelong for MHVs (I A); INR self-management recommended; ASA add-on clarified. |
TAVI antithrombotics | Single antiplatelet therapy standard; DAPT discouraged; DOAC rules clarified. |
Care model | Structured Heart Valve Networks; Heart-Team mandated; patient-centered decision-making. |




No comments yet!