Use of advanced coronary techniques in bailout of aortic valvuloplasty balloon entrapment
Supported by the EuroIntervention Journal
Authors
Siu-Fung Wong1, James Cockburn1, Christopher Broyd1, Joao Martins1, David Hildick-Smith1
Case summary
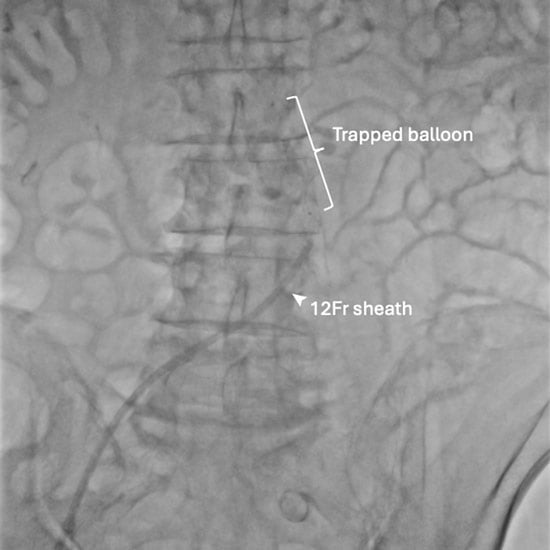
An 81-year-old male patient with symptomatic severe aortic stenosis was admitted for transcatheter aortic valve intervention via right radial and femoral accesses. The native aortic valve was predilated with a 24-mm TrueTM balloon (BD, Franklin Lakes, NJ, USA), delivered via a 12F sheath. The deflated balloon could not be retrieved. Further withdrawal resulted in concertina of the sheath (Figure 1A).
Figure 1. Bailout for aortic valvuloplasty balloon entrapment with schematic illustration of the procedure.
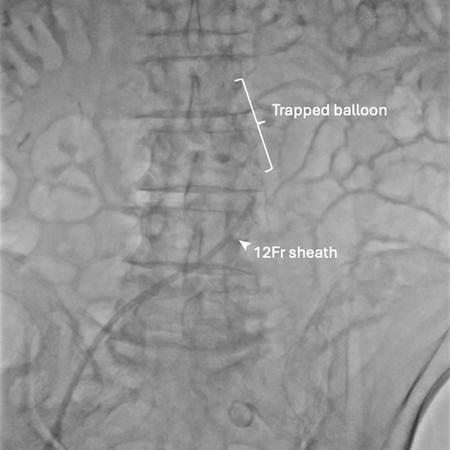
Figure 1A: Failed balloon retrieval.
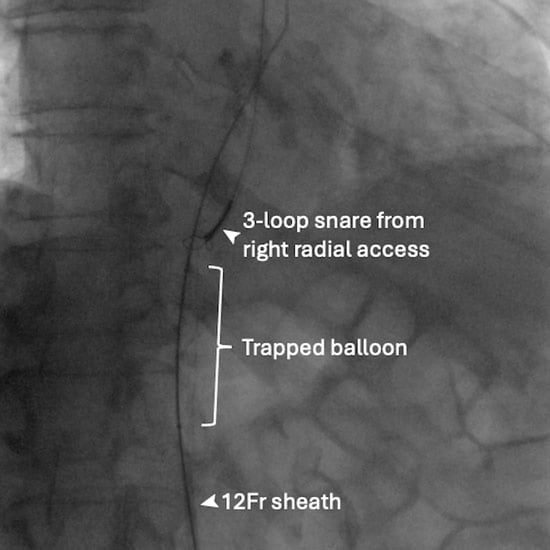
Physical withdrawal of the unsheathed deflated balloon was considered and briefly attempted but was resisted, and severe damage to the calcified iliac and femoral systems was feared. Snaring of the balloon tip from the right radial access for straightening the system did not help with retrieval (Figure 1B).
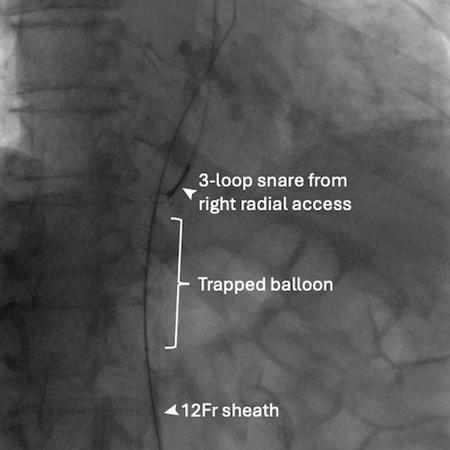
Figure 1B: Snaring from right radial access.
Access from the left femoral was considered, but the angulation of the iliac bifurcation was very acute. We therefore cut the balloon and Amplatzer Super StiffTM wire (Boston Scientific, Marlborough, MA, USA) 40 cm from the skin entry point, snared the very tip of the balloon catheter from the right radial artery and internalised the transected balloon system, holding the wire with forceps outside the body for maintaining access, aiming to introduce a larger sheath to help with retrieval (Figure 1C, Moving Image 1).
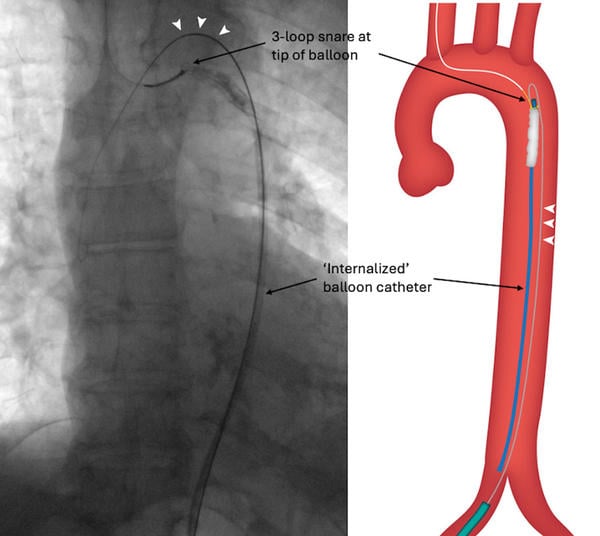
Figure 1C: ‘Internalisation’ of balloon with a 0.035’ wire running parallel to it (arrowheads).
With a new 0.035’ wire running parallel to the internalised balloon, a 20F sheath was introduced. However, the angle for balloon retrieval remained very unfavorable due to femoral calcification and tortuosity. To straighten the system, A Gaia Next® 2 wire (Asahi Intecc, Aichi, Japan) was used to rewire the central lumen of the transected balloon shaft in a ‘tip-in’ fashion (Figure 1D, Moving image 2).
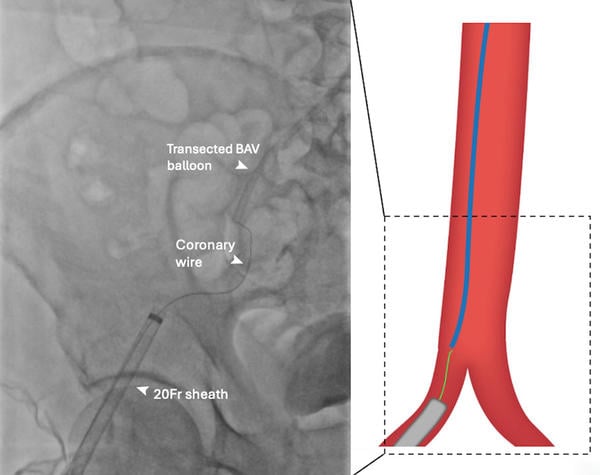
Figure 1D: ‘Tip-in’ rewiring of central lumen of transected valvuloplasty balloon.
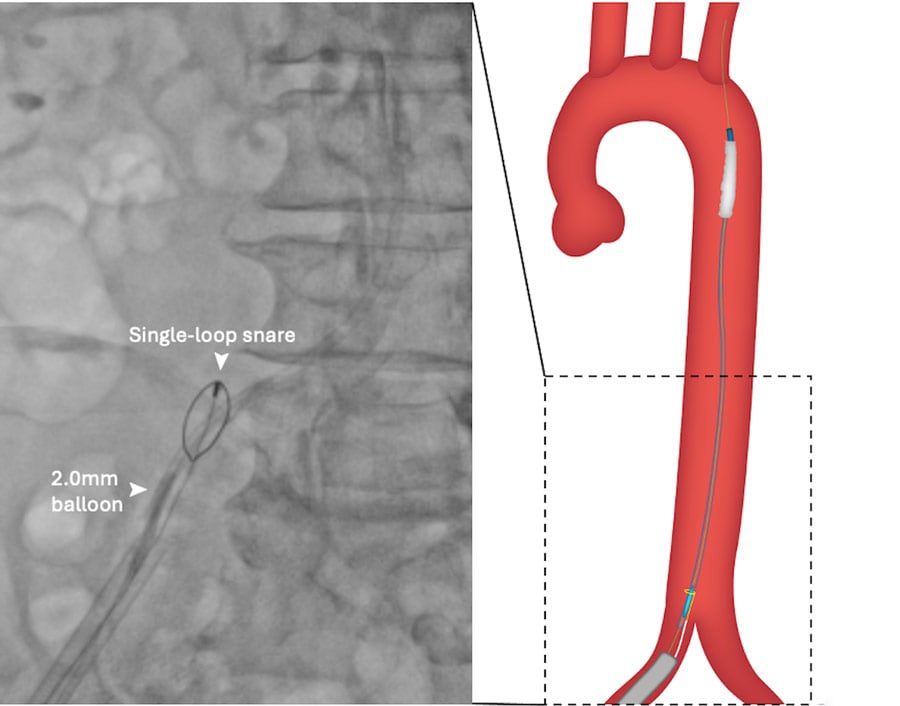
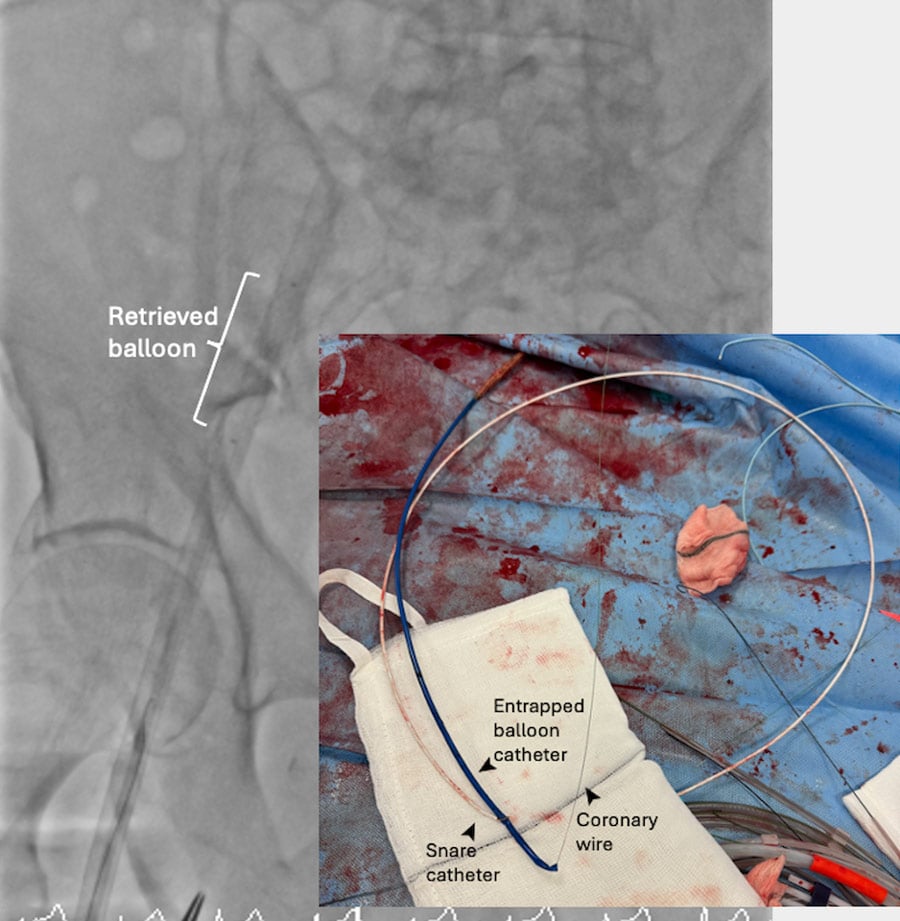
Once this was achieved, internal anchoring with a 2-mm balloon inflated within the wire lumen of the transected valvuloplasty balloon and ipsilateral snaring with a 5-mm Amplatz Goose SnareTM (Medtronic) straightened the system and allowed successful retrieval of the balloon (Figure 1E, Figure 1F, Moving image 3).
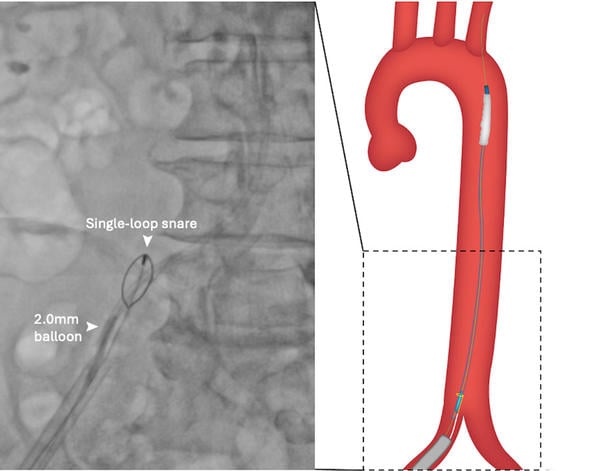
Figure 1E: Ipsilateral snaring and 2-mm balloon anchoring in central lumen of transected balloon.
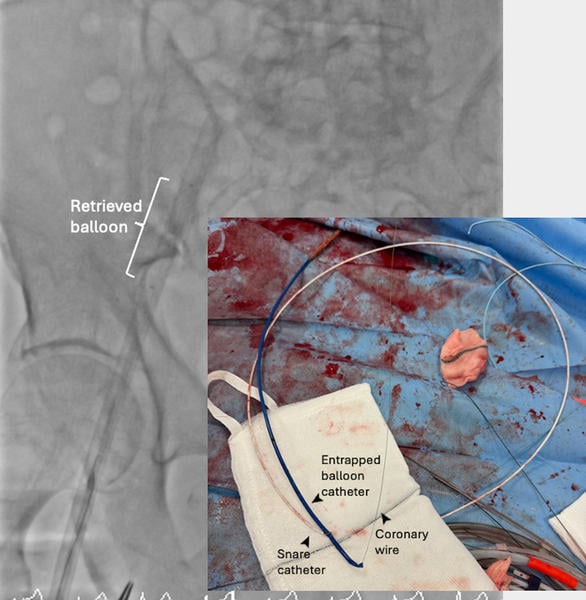
Figure 1F: Successful retrieval of entrapped balloon.
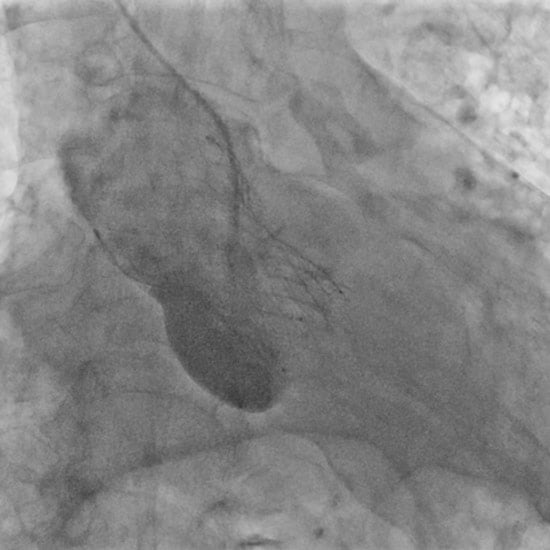
A 34-mm Evolut transcatheter aortic valve (TAV) (Medtronic) was deployed with a good result (Figure 1G). Closure of the femoral access site was uneventful (Figure 1H).
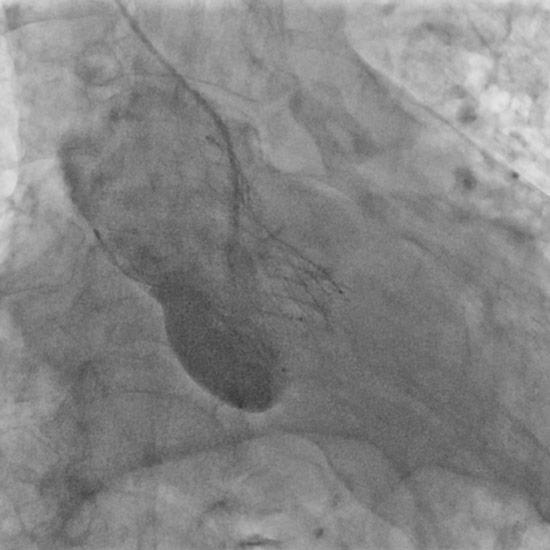
Figure 1G: Implantation of self-expanding transcatheter aortic valve.

Figure 1H: Femoral angiogram demonstrated successful percutaneous closure.
Balloon entrapment in valvuloplasty is an uncommon but potentially fatal complication that can occur especially after the balloon ruptures or inadvertent passage through a cell of a newly implanted TAV1,2.
While balloon aortic valvuloplasty can be done with smaller-sized sheath, this limits the bailout options when entrapment occurs. Here, we reported a novel technique of balloon ‘internalisation’, allowing for sheath upsizing with the balloon fixed in-vivo by a safety snare.
Re-access to the balloon was achieved with coronary chronic total occlusion wires. Simultaneous small balloon anchoring and ipsilateral snaring ensured optimal alignment with femoral sheath, leading to successful retrieval.
References
- Haberman D, Lupu L, Rogers T, Satler LF, Waksman R, Ben-Dor I. Extraction Of Irretrievable Ruptured Balloon During Balloon Aortic Valvuloplasty Using A Bailout Technique. Cardiovasc Revasc Med. 2024; 2: 100017
- Cubero-Gallego H, Millan X, Asmarats L, Li CH, Vaquerizo B, Arzamendi D. Transcatheter Aortic Valve Prosthesis Displacement After Postdilation Balloon Entrapment: A Scary Challenge Solved. JACC Cardiovasc Interv. 2022; 15(15): e175-e177.
Affiliation
- Sussex Cardiac Centre, Royal Sussex County Hospital, University Hospitals Sussex NHS Foundation Trust, England
Conflicts of interest
- Dr. James Cockburn reports he is a proctor/advisory for Boston and Medtronic.
- Prof. David Hildick-Smith reports he is a proctor/advisory for Boston, Edwards Lifesciences, Medtronic and Abbott.
- The remaining authors report no relationships with industry and other entities.







No comments yet!