Complex PCI supported by a guide catheter extension system through the frames of a self-expandable trans-catheter heart valve
Supported by the EuroIntervention Journal
Authors
Andrea Buono1, Alfonso Ielasi1, Mattia Glauber2, Maurizio Tespili1
Case summary
An 84-year-old man with arterial hypertension and previous hepatocellular carcinoma was admitted to our Emergency Department for new onset of exertional angina (CCS 3). The patient had a history of three-vessel coronary artery disease treated by complete surgical revascularization in 2007 (left internal mammary artery on left anterior descending artery and sequential saphenous graft to ramus and posterior descending artery). Twelve years later, due to severe symptomatic (effort dyspnoea, NYHA III) aortic valve stenosis, the patient underwent trans-catheter aortic valve replacement (TAVR) with a 29-mm Evolut R transcatheter heart valve (THV, Medtronic, Minneapolis, Minnesota) implantation.
Pre-TAVR coronary angiography revealed the patency of both arterial and venous grafts and the presence of severe ostial left circumflex artery (LCx) stenosis (Figure A), treated conservatively by Heart Team decision (considering the absence of angina and patient’s age and comorbidities).
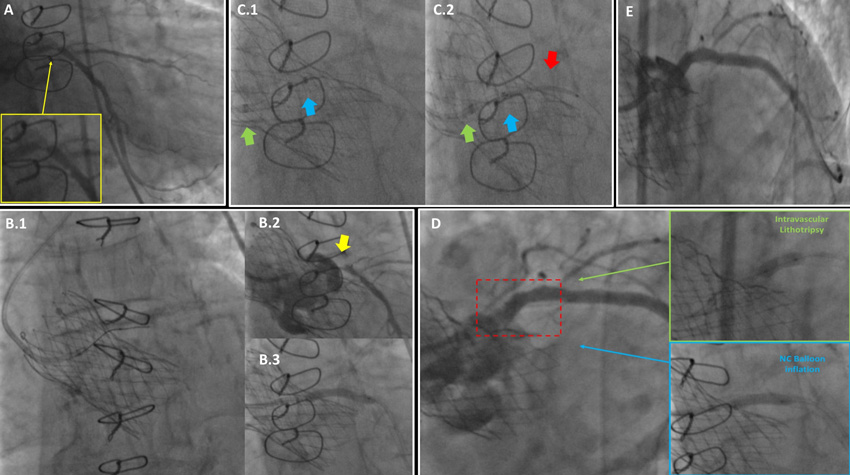
Figure A:
A: Severe ostial left circumflex (LCx) stenosis (zoom in the yellow box), associated with other significant lesion in the mid and distal segment, at pre-TAVR coronary angiography.
B.1: Challenging post-TAVR left coronary artery engagement through the transcatheter heart valve (THV) with 3.5 mm Judkins left (JL) catheter and subsequently vessel wiring;
B.2: subselective vessel opacification, confirming the need to perform LCx percutaneous coronary intervention due to severe ostial stenosis (yellow arrow);
B.3: Ostial LCx lesion pre-dilatation with 3.0x24mm non-compliant balloon, demonstrating full device expansion.
C.1-2: Guideliner catheter (blue arrow), increasing the JL catheter back-up support (green arrow), allowed delivery and implantation through THV of three drug-eluting stents (DES) (3.5x30, 3.5x22 and 4.0x8 mm respectively) from distal LCx to left main shaft (red arrow showing the first implanted one).
D: Ostial LCx DES segment appears under-expanded (dashed red box). Subsequent management by intravascular lithotripsy (green box) and post-dilation with a fully expanded 4.0x15mm non-compliant balloon (blue box).
E: Final angiographic result.
At the moment of our re-assessment (4 months after TAVR), no THV dysfunction was documented at echo and a new invasive angiography was scheduled in suspicion of unstable angina. Left coronary cannulation appeared challenging: a variety of guiding catheter failed to provide a selective engagement, from both radial and femoral accesses.
Finally, a 6 Fr 3.5 mm Judkins left guiding catheter was helpful to partially engage the left coronary ostium, identifying ostial LCx as the culprit lesion, and allowing to wire the distal LCx (Figure B.1-2 and Movie image 1).
Multiple pre-dilatations of the target lesion were performed (Figure B.3).
Due to non-coaxial guiding catheter alignment and suboptimal back-up support, drug-eluting stent (DES) delivery through THV frames failed. A guide catheter extension system (GuideLiner, Vascular Solutions Inc., Minneapolis) was then useful to deeply engage the left main (LM) allowing the delivery of three DES implanted in overlap from distal LCx to LM shaft (Figure C.1-2 and Movie image 2).
Despite optimal pre-dilatation (on the evidence of full expansion of both 3.0 mm semi-compliant and non-compliant balloons, with the latter inflated at maximum 18 atm), proximal DES was not fully expanded (Figure D). As a bail-out strategy intravascular lithotripsy (Shockwave Medical, Fremont, CA) was performed (through the GuideLiner), inflating a 3.5x12mm balloon (at 4-6 atm for 8 cycles of 10 pulses each) followed by a post-dilatation (4.0x15 mm non-compliant balloon, Figure D). Final angiographic view showed the absence of remaining under-expanded stent segments (Figure E and Movie image 3).
Percutaneous coronary intervention (PCI) post-TAVR can be technically difficult for challenging coronary re-engagement, particularly in patients with self-expanding THV that, by design, extend above the coronary ostia (1). In such cases, guide catheter extension is a valid option to provide a more selective engagement and guarantee adequate support during complex PCI requiring the delivery of multiple devices.
Conflict of interest statement
All authors have nothing to disclose.
Affiliations
- Interventional and Clinical Cardiology Unit, S. Ambrogio Cardio-Thoracic Center, Milan, Italy
- Mini-Invasive Cardiac Surgery Unit, S. Ambrogio Cardio-Thoracic Center, Milan, Italy
References
- Yudi MB, Sharma SK, Tang GHL, Kini A. Coronary Angiography and Percutaneous Coronary Intervention After Transcatheter Aortic Valve Replacement. J Am Coll Cardiol. 2018 Mar 27;71:1360-1378.







No comments yet!