Performing BASILICA: a step-by-step guide to prevent coronary obstruction during TAVI
A problem-solving step-by-step tutorial
Frequency of the problem:
Expert level:
Summary
Coronary obstruction (CO) is a rare but catastrophic complication of transcatheter aortic valve implantation (TAVI), especially in valve-in-valve or anatomically high-risk patients. The BASILICA procedure — Bioprosthetic or Native Aortic Scallop Intentional Laceration to prevent Iatrogenic Coronary Artery obstruction — offers a reproducible technique to mitigate this risk.
This Toolkit article provides a step-by-step overview based on hands-on experience with the procedure. It emphasises patient selection, necessary equipment, intraprocedural imaging, and practical tips to increase safety and success. A visual roadmap showing all steps and procedural tips are provided to help operators incorporate BASILICA effectively into their TAVI programs.
The problem
CO during TAVI, particularly in valve-in-valve procedures, can result in hemodynamic collapse, myocardial damage, and even mortality. Standard preventive strategies like chimney stenting may not suffice in selected anatomies.
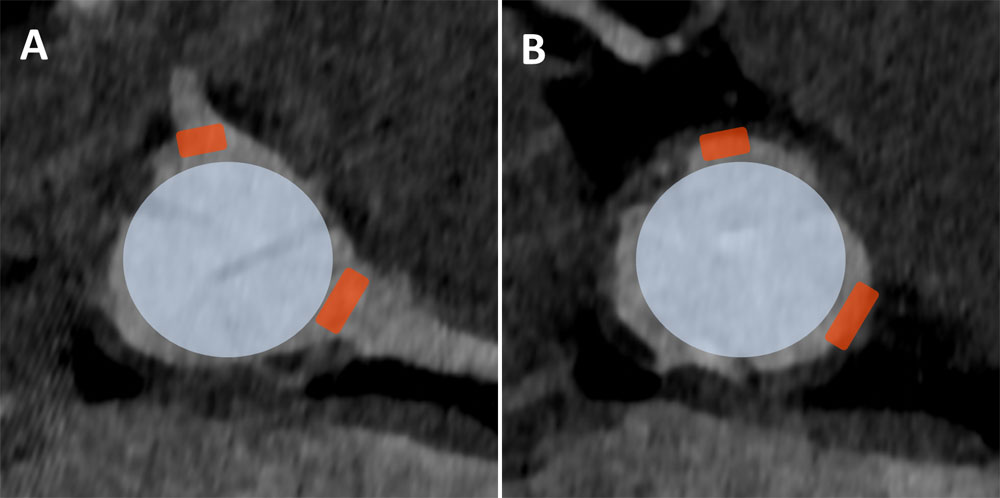
There is a need for a leaflet modification technique that reduces this risk in high-risk patients with unfavourable virtual valve-to-coronary (VTC) or valve-to-sinotubular-junction (VTSTJ) distances1. These measurements can be used to risk stratify patients according to risk for CO2.
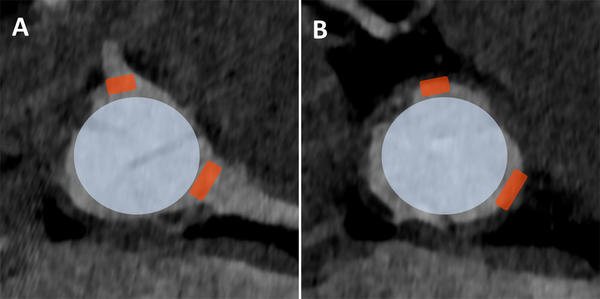
A. Valve-to-coronary distance (VTC) measured at both coronary arteries
B. Valve-to-sinotubular-junction distance (VTSTJ) measured at the corresponding location of the coronary arteries, at the level of sino-tubular-junction
Principal idea
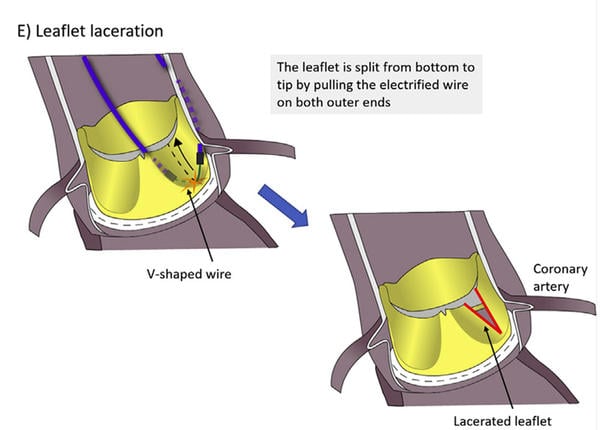
The BASILICA technique involves intentional leaflet laceration using an electrified guidewire prior to valve implantation, thereby creating a path for coronary perfusion. This results in the lateral displacement of the lacerated half-leaflets, thus preventing the displaced leaflet from occluding the coronary ostium, making it a proactive solution for high-risk anatomies.
The technique is increasingly accepted and can be safely adopted with appropriate training and planning, with reproducible results. The principal idea of leaflet laceration to protect the coronaries forms the basis for later developed dedicated mechanical devices that facilitate leaflet laceration3.
Material needed
- Vascular access
- DrySeal Flex 14-22 F x 33 cm
- Vascular closure device: only suture-based, or in combination with plug-based
- Targeting and traversing
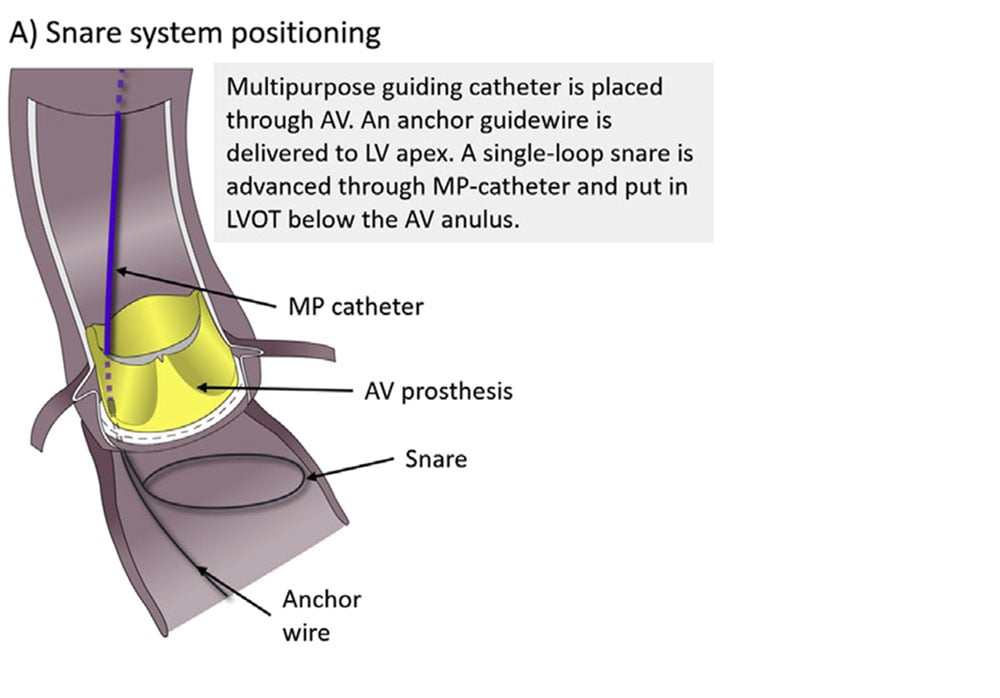
- Single-loop snare 20-30 cm
- Guidewire: 0.018” stiff (such as V-18, Boston Scientific) or 0.014” stiff (such as Spartacore, Abbott) anchor guidewire
- 6 F x 100 cm JR4 or MP guiding catheter
- Left leaflet: 7-8 F x 100 cm AL (2-4) or EBU (3.75, 4 or 5) guiding catheter
- Right leaflet: 7-8 F x 100 JR4, MP, IM or AR1 guiding catheter
- IM diagnostic 5 F x 125 cm
- PiggyBack® Wire Converter or microcatheter
- Stiff 0.014” x 300 cm wire: Astato XS 20
- Electrosurgical generator
- Electrosurgery pencil
- Laceration
- Torquers: 0.014” and 0.035”
- 50-60 mL Luer Lock syringes and glucose 5 % solution
- Standard TAVI equipment
- TEE (Trans-esophageal echocardiography)

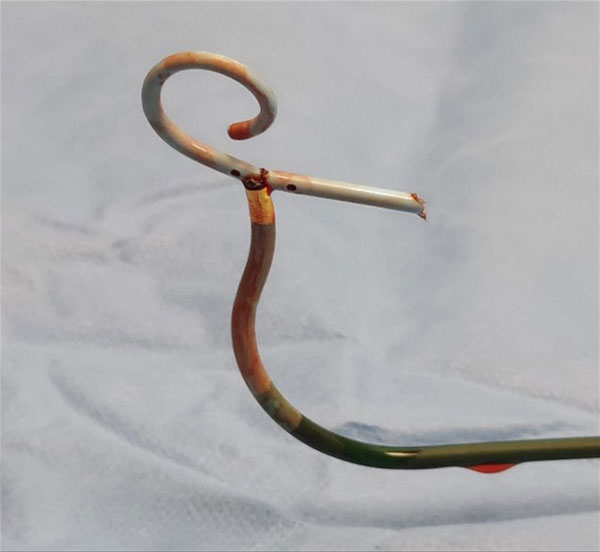
Electrosurgical pencil
Step-by-step method
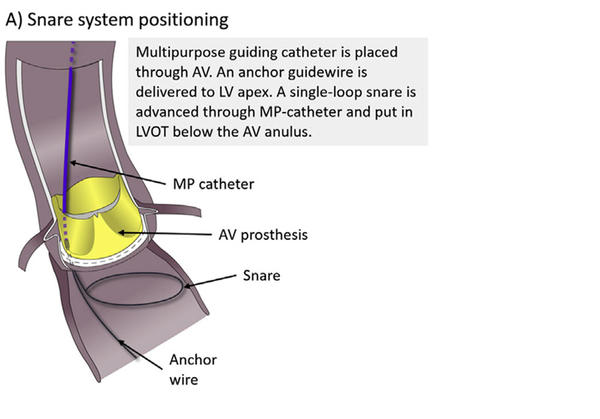
Step 1
Access & snare positioning4
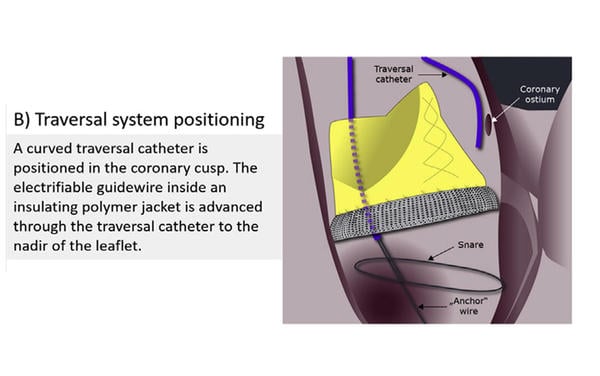
Step 2
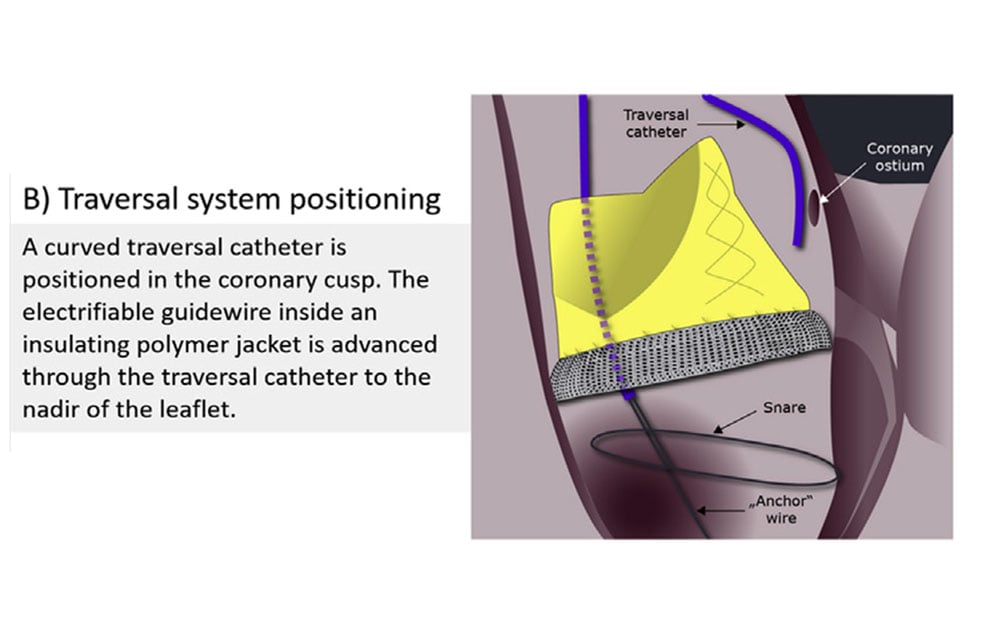
Traversal system positioning
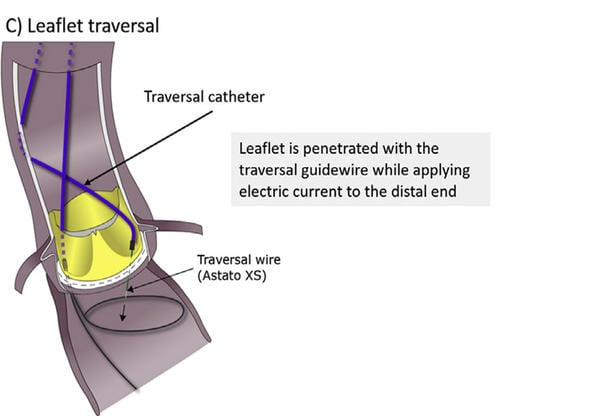
Step 3
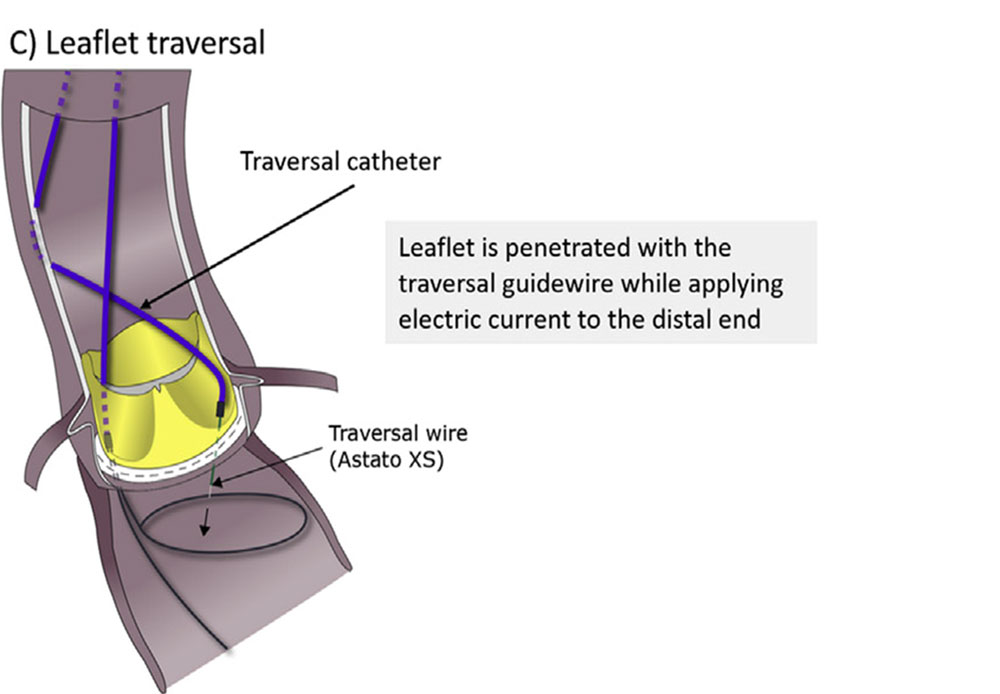
Leaflet traversal
Step 4
Snaring and delivering the flying “V”
- The traversal wire is snared in the left ventricular outflow tract (LVOT) and retrieved through the aortic valve in the MP catheter (video 4)
- The anchor wire is removed from the LV
- The V-shaped portion of the traversal wire is delivered to the traversed leaflet (video 5)
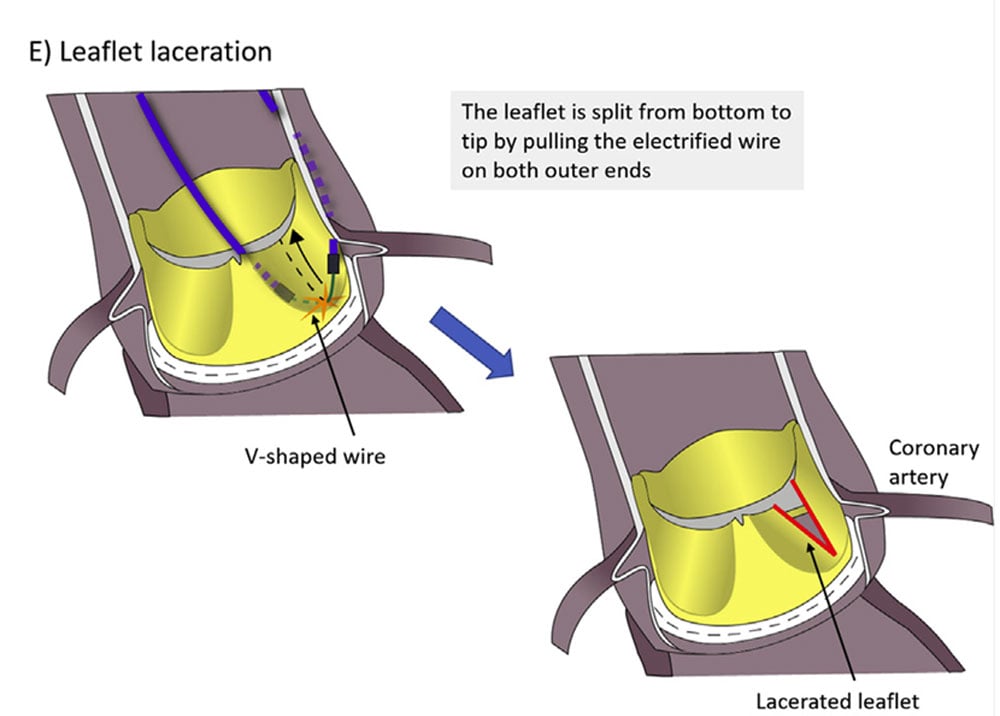
Step 5
Leaflet laceration
Points of specific attention
- Bulky calcific nodules on the leaflets may limit the success.
- Proper wire positioning and loop tension are critical for a successful laceration.
- Avoid crossing or lacerating the mitral valve apparatus.
- Continuous hemodynamic and imaging guidance is key – TEE can guide positioning.
- Electrical isolation of the guidewire is necessary for effective laceration.
- Proctoring with first few cases can be very helpful.
References
- Lederman, R. J., Babaliaros, V. C., Rogers, T., Khan, J. M., Kamioka, N., Dvir, D., & Greenbaum, A. B. (2019). Preventing Coronary Obstruction During Transcatheter Aortic Valve Replacement: From Computed Tomography to BASILICA. In JACC: Cardiovascular Interventions (Vol. 12, Issue 13, pp. 1197–1216). Elsevier Inc. https://doi.org/10.1016/j.jcin.2019.04.052
- Kitamura, M., Wilde, J., Dumpies, O., Richter, I., Obradovic, D., Krieghoff, C., Gohmann, R. F., Majunke, N., Desch, S., Gutberlet, M., Borger, M., Marwan, M., Thiele, H., Holzhey, D., & Abdel-Wahab, M. (2022). Risk Assessment of Coronary Obstruction During Transcatheter Aortic Valve Replacement: Insights From Post-BASILICA Computed Tomography. JACC: Cardiovascular Interventions, 15(5), 496–507. https://doi.org/10.1016/j.jcin.2022.01.003
- Dvir, D., Leon, M. B., Abdel-Wahab, M., Unbehaun, A., Kodali, S., Tchetche, D., Pibarot, P., Leipsic, J., Blanke, P., Gerckens, U., Manoharan, G., Harari, E., Hellou, E., Wolak, A., Ben-Assa, E., Jubeh, R., Shuvy, M., Koifman, E., Klein, C., & Kempfert, J. (2023). First-in-Human Dedicated Leaflet Splitting Device for Prevention of Coronary Obstruction in Transcatheter Aortic Valve Replacement. JACC: Cardiovascular Interventions, 16(1), 94–102. https://doi.org/10.1016/j.jcin.2022.10.050
- Protsyk, V., Meineri, M., Kitamura, M., Flo Forner, A., Holzhey, D., Thiele, H., Mackensen, G. B., Dvir, D., Abdel-Wahab, M., & Ender, J. K. (2021). Echocardiographic Guidance of Intentional Leaflet Laceration prior to Transcatheter Aortic Valve Replacement: A Structured Approach to the Bioprosthetic or Native Aortic Scallop Intentional Laceration to Prevent Iatrogenic Coronary Artery Obstruction Procedure. In Journal of the American Society of Echocardiography (Vol. 34, Issue 6, pp. 676–689). Mosby Inc. https://doi.org/10.1016/j.echo.2021.01.015
The invited Expert's opinion
Since its first description by Khan et al.2, the BASILICA technique (Bioprosthetic or Native Aortic Scallop Intentional Laceration to prevent Coronary Artery obstruction) has been increasingly adopted as a viable and effective method of leaflet modification. While dedicated devices for leaflet laceration are not yet commercially available, BASILICA remains the preferred approach to prevent CO in many experienced centers.
In their My Toolkit article, Ahmed Abdelhafez and Mohamed Abdel-Wahab provide an excellent, practical summary of the procedural steps and required tools for BASILICA. When performed as outlined, the technique can be executed safely and reproducibly by experienced operators. However, interventionists must be aware of key pitfalls and potential complications. First, BASILICA acutely increases aortic regurgitation (AR). Although most patients remain hemodynamically stable, a pressure drop is frequently observed. Therefore, a baseline systolic pressure > 120 mmHg is advisable before leaflet laceration. While many centers, including ours, now routinely use over-the-wire pacing for standard TAVI, a temporary pacemaker is recommended for BASILICA to allow rapid pacing, should acute AR cause hemodynamic compromise.
It is also important to recognise that successful leaflet splitting does not guarantee coronary patency. Coronary obstruction may still occur, particularly in TAVI-in-TAVI cases, where a balloon-expandable valve may overextend the index THV and displace native leaflets toward the sinuses. In patients with severely effaced sinuses, lacerated leaflets may prolapse into the coronary ostia resulting in partial obstruction. Finally, operators should respect the power of electrosurgery: an electrified wire can inadvertently transect other catheters if they are caught by the “flying V” (Figure 1).
In conclusion, BASILICA exemplifies a new era in structural heart intervention where procedural safety depends increasingly on meticulous planning, high-resolution imaging, and technical skill. While multicenter data confirm its high success rates, wider adoption is limited by perceived complexity and training demands. In this context, the present article provides an outstanding and practical contribution to bridging the gap between evidence and clinical practice.
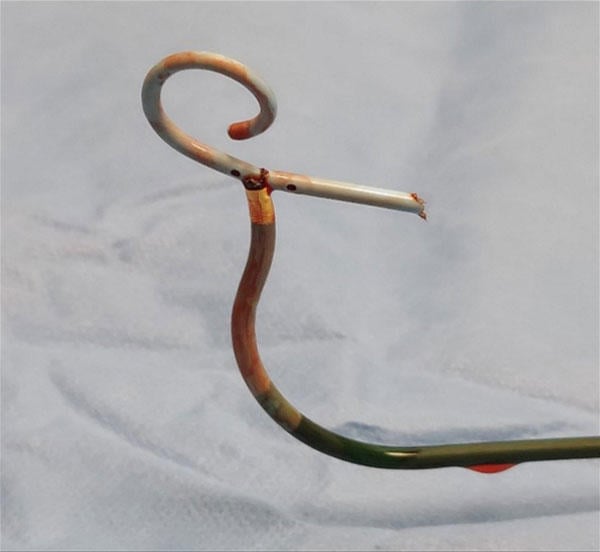
Figure 1: In this BASILICA case, the pigtail catheter parked in the left ventricle was accidentally caught by the ‘flying V’ and cut during leaflet laceration. It was retrieved using a snare.
References
- Tang GHL, Komatsu I, Tzemach L, Simonato M, Wolak A, Blanke P, Dvir D. Risk of coronary obstruction and the need to perform BASILICA: the VIVID classification. EuroIntervention. 2020 Oct 9;16(9):e757-e759. doi: 10.4244/EIJ-D-20-00067. PMID: 32364501.
- Khan JM, Dvir D, Greenbaum AB, Babaliaros VC, Rogers T, Aldea G, Reisman M, Mackensen GB, Eng MHK, Paone G, Wang DD, Guyton RA, Devireddy CM, Schenke WH, Lederman RJ. Transcatheter Laceration of Aortic Leaflets to Prevent Coronary Obstruction During Transcatheter Aortic Valve Replacement: Concept to First-in-Human. JACC Cardiovasc Interv. 2018 Apr 9;11(7):677-689. doi: 10.1016/j.jcin.2018.01.247. PMID: 29622147; PMCID: PMC6309616.
Disclosures
The authors declare no conflicts of interest to disclose.
Authors









No comments yet!