Distal radial access
A problem-solving step-by-step tutorial
Distal radial access has rapidly evolved from an alternative technique to a valuable strategy for preserving radial patency while improving patient comfort and access-site safety.
This My Toolkit article provides a practical, problem-solving approach to understanding distal radial anatomy, overcoming technical challenges, and integrating ultrasound guidance to make DRA a reliable option in everyday interventional practice.
Frequency of the problem:
Expert level:
Summary
Less than a decade ago, distal radial access (DRA) emerged as an evolution of the transradial approach, offering improved ergonomics for both patients and operators and the potential for fewer post-procedural complications.
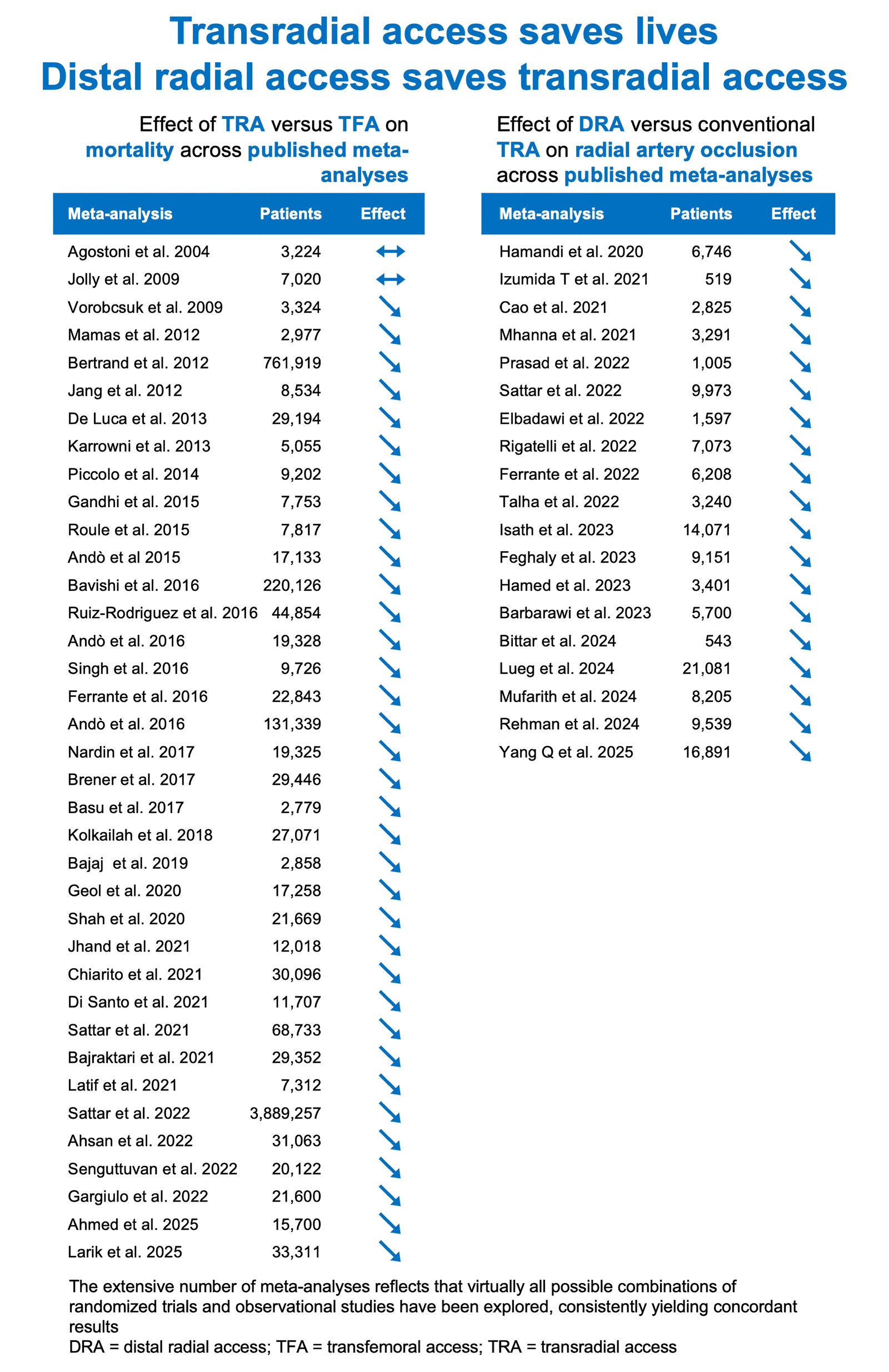
Over recent years, nearly 20 meta-analyses, including varying combinations of randomised and real-world data, have consistently demonstrated decrease in radial artery occlusion and reduced access-site bleeding, despite simpler haemostasis management.
These advantages are particularly relevant in contemporary interventional practice, as innovations in devices and techniques continue to expand radial access across an increasing range of procedures, both as a primary and ancillary route, not only in cardiology but also in interventional radiology and neurointervention.
Within this evolving landscape, DRA presents a coherent strategy for delivering a safer and more comfortable experience for patients, simplifying management for the care team, and ensuring that the long-term benefits of radial access, including reduced mortality, remain available for future interventions.
The problem
Despite the important advantages of DRA, its adoption remains limited, partly because randomised trials report a higher crossover rate compared with conventional TRA, even though most crossovers occur to another radial site and preserve procedural benefits of a radial approach.
These crossovers are largely attributable to anatomical factors. Unlike the forearm radial artery, which runs in a straight, predictable plane, the distal radial artery follows a more curvilinear and variable course in the hand and is generally smaller. Limited familiarity with the relevant distal radial anatomy and the rationale for preserving radial access may also help explain its slower uptake.
Principal idea
Embracing the rationale for preserving radial access in the patient journey provides the foundation for optimising outcomes and implementing DRA.
Consolidating knowledge of the specific anatomical features of the distal radial artery enables adaptation to its unique characteristics.
Developing proficiency in ultrasound assessment and guidance of DRA allows overcoming its technical challenges and ultimately elevates performance in vascular access, enhancing the quality, safety, and consistency of interventional practice.
Material needed
- Rationale
- Key meta-analyses comparing radial with femoral access
- Anatomical landmarks
- Atlas of anatomy
- Ultrasound assessment and guidance
- Linear transducer, ideally handheld
- Vascular access
- Bare metal needle
- Mini guidewire
- Thin-walled introducer sheath
- Haemostatic
- Compression device or bandage
Step-by-step method
Step 1
Landmark meta-analyses
Meta-analyses comparing radial to femoral access have consistently showed reductions in mortality and other complications with radial access, forming the scientific rationale for preserving this approach whenever possible.
Meta-analyses comparing DRA to conventional transradial access have systematically shown a significant reduction of radial artery occlusion with DRA. Together, these findings highlight the role of DRA in contemporary practice, where maintaining long-term arterial patency enhances patient safety and procedural versatility across the care pathway.
Step 2
Fundamental anatomical references
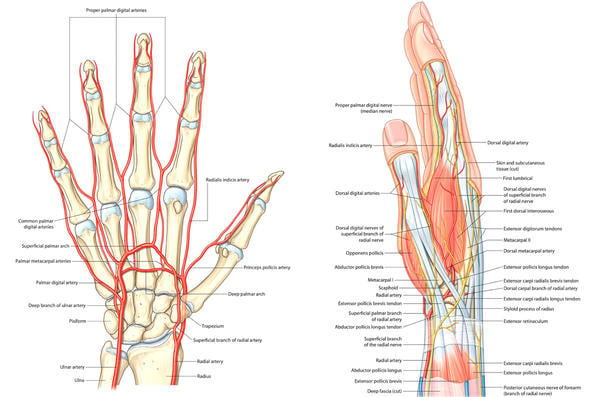
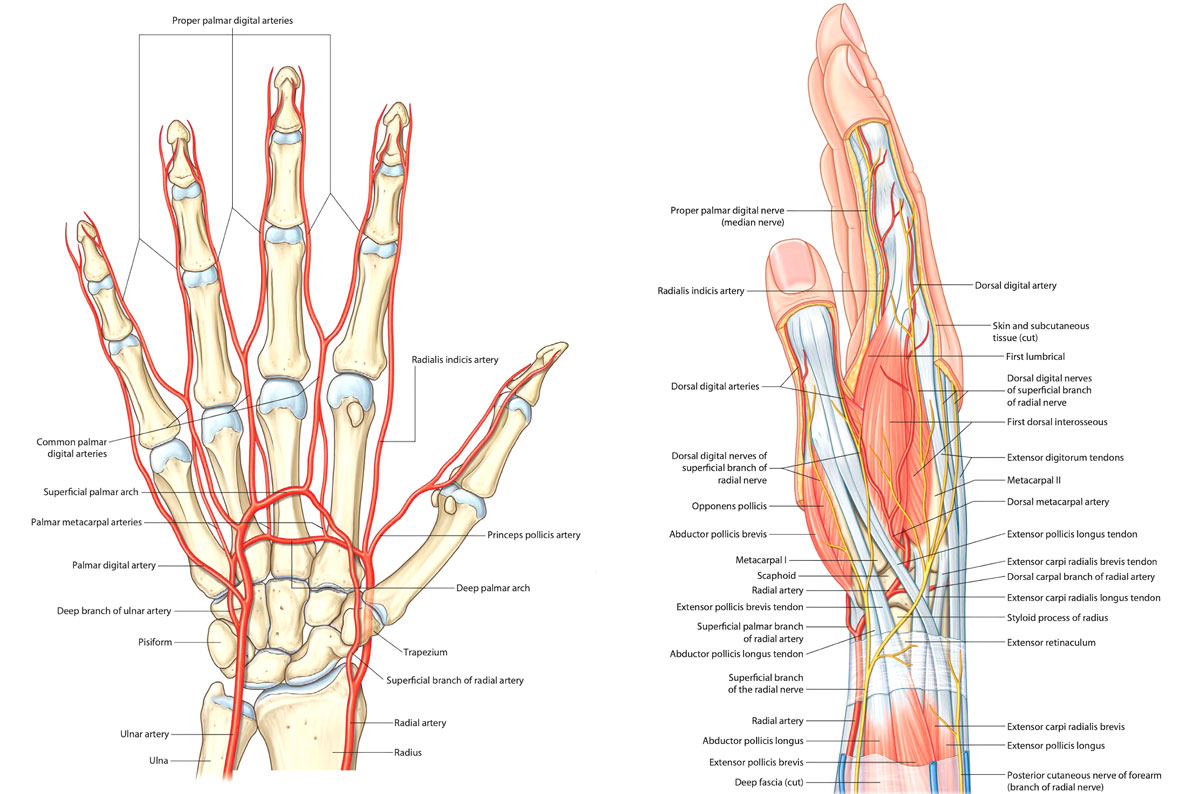
A clear understanding of the arterial vascularisation of the hand is essential to appreciate the physiological advantages of DRA and its role in preserving radial flow. Familiarity with the anatomy of the anatomical snuffbox is equally important for performing a safe, efficient, and well-targeted puncture.
Step 3
Cathlab and operator setups
Three practical configurations for implementing DRA in the cathlab: right DRA; left DRA with puncture performed on the patient’s left side with the upper limb in abduction, followed by adduction to align the hand with the femoral workspace; and left DRA with puncture performed directly with the hand positioned on the groin. These setups facilitate seamless integration of DRA into existing workflows while preserving ergonomic consistency and procedural efficiency.
Step 4
Optimal hand positioning
The hand is oriented with the anatomical snuffbox facing upward. A slight ulnar deviation elongates the distal radial artery, while thumb adduction brings it closer to the surface in the anatomical snuffbox.
This can be achieved by having the patient grasp the thumb, hold a 20 cc syringe, grip a rolled gauze pad, or handle a dedicated radial support.
The handle also allows precise, retained adjustments of hand position before and after draping.
Step 5
Ultrasound assessment
After reducing the depth and optimizing the focus of the ultrasound image, the distal radial artery is first scanned in longitudinal view, with colour Doppler used to clarify its course. The probe is then rotated into the transversal plane to identify the optimal puncture site. Colour Doppler is applied initially to confirm arterial position.
Handheld ultrasound devices can meaningfully streamline this step, as they may be pre-sheathed for immediate sterile use, avoid cable traction and the whole logistical burden of a full-sized machine, and allow rapid arterial assessment even before the patient enters the cath lab.
Step 6
Ultrasound-guided puncture
The needle, probe marker, and arterial “disk” are first aligned in the transversal plane, confirmed by a centred needle echo vertically in line with the artery. The needle is then tilted and advanced to achieve a clean 12 o’clock entry under real-time ultrasound visualisation.
Ultrasound guidance also allows effective needle redirection when initial contact occurs along the lateral wall, ensuring an optimal intraluminal entry.
Step 7
Haemostasis
The haemostatic device is placed around the hand and secured. The air bladder is inflated as the introducer sheath is withdrawn. Haemostasis is then adjusted by deflating the bladder in 2-cc steps until minimal bleeding appears, followed by reinflating the same 2 cc to achieve stable, low-pressure compression that further helps preserve arterial flow.
Haemostasis after DRA can be achieved using an elastic haemostatic bandage, an adhesive haemostatic pressure pad, a classical radial compression device, or a dedicated distal radial haemostasis device. When a TR Band is used, removing the rigid plastic plate allows the device to conform more naturally to the patient’s hand, though attention should be paid to preventing the device from slipping around the hand.
Points of specific attention
- Given the distal radial artery’s superficial course and its minimal distance from underlying bones, an anterior-wall puncture with a bare needle is preferred over a through-and-through approach
- Because the distal radial artery does not run linearly beneath the skin, the arterial-entry angle differs from the skin-entry angle, and the needle trajectory should be adapted to the vessel curvature
- Puncture within the anatomical snuffbox is recommended to leverage the bony floor and tendon boundaries for safer haemostasis
- As the distal radial artery is approximately one French smaller than at the wrist, selecting thin-walled sheaths is a logical choice
A word from the reviewer
Distal radial access (DRA) represents a purposeful extension of the radial-first strategy, with the primary goal of preserving proximal radial artery patency while maintaining procedural safety and patient comfort. As repeat and increasingly complex interventions become more common, safeguarding future access options has gained clear clinical relevance.
This article appropriately anchors DRA within the existing evidence base. Meta-analyses consistently demonstrate lower rates of radial artery occlusion and access-site bleeding with DRA compared with conventional transradial access, together with simpler haemostasis. Although higher crossover rates have been reported, these largely reflect distal radial anatomy and most often remain within the radial spectrum, preserving the benefits of a radial approach.
A key strength of this tutorial is its anatomy-driven, problem-solving framework. The distal radial artery is smaller, more superficial, and follows a curvilinear course over a rigid bony plane, necessitating adapted puncture geometry with preference for anterior-wall entry and trajectory adjustment to vessel curvature.
Ultrasound guidance is therefore central to reliable DRA. Systematic assessment clarifies vessel calibre and course, while real-time guidance enables accurate 12 o’clock arterial entry and controlled needle redirection. When combined with precise puncture and low-pressure haemostasis within the anatomical snuffbox, these principles position DRA as a reproducible and scalable technique that enhances access-site safety while preserving future procedural options.
Conflicts of interest
Dr. Nazmi Calik reports no conflicts of interest.
Disclosures
- Dr Sgueglia reports consulting and lecture fees from Terumo, Cordis, Merit Medical, GE Healthcare, B. Braun, and Philips Volcano, outside the submitted work, and an unrestricted research grant to the institution from Biolife, outside the submitted work.
- Dr Colletti reports consulting fees from Philips Healthcare and honoraria for educational events from Boston Scientific and Abbott Vascular, outside the submitted work.
- Dr Iglesias reports unrestricted research grants to the institution from Biotronik, Concept Medical, and SMT, outside the submitted work; consulting fees from Biotronik, ReCor Medical, Cordis, and Medtronic, outside the submitted work; speaker fees from Abbott Vascular, Biotronik, Biosensors, Bristol Myers Squibb/Pfizer, Cordis, Concept Medical, Medtronic, Penumbra Inc., and ReCor Medical, outside the submitted work; support for attending meetings and/or travel from Biotronik and Medtronic, outside the submitted work; and participation on the DSMB for the Co-STAR (NCT04870424) and REGENERATE-COBRA (NCT05711849) trials, outside the submitted work.
- Dr Aminian reports serving as a consultant for Terumo.
- Dr. Ungureanu, Dr. Mugnolo and Dr. Sciahbasi report no conflicts of interest.
Authors












No comments yet!