
27 Sep 2021
World Heart Day 2021 - Pandemic and heart diseases: lessons learnt for the future
#WorldHeartDay 2021 on PCRonline!
Giulio Stefanini and Emanuele Barbato take the opportunity of World Heart Day to review the impact of the Covid-19 pandemic on cardiovascular care at a time when the pandemic has highlighted the gaps between different health systems.
In the last two years, Covid-19 pandemic has profoundly impacted healthcare in general and cardiovascular care in particular, with direct and indirect effects on the management of patients with cardiovascular diseases.
Direct effects of Covid-19
Since the first lines of evidence published on Covid-19 in China, it was clear that patients with cardiovascular comorbidities (e.g., arterial hypertension, history of coronary artery disease, atrial fibrillation, etc.) were at higher risk of severe Covid-19 with subsequent mortality.
Data available a few months later from Europe and the United States were consistent with the initial Chinese evidence.
Early investigations also described a cardiac involvement in some patients with Covid-19, suggesting that SARS-CoV-2 could directly damage the myocardium. Multiple case series of confirmed myocarditis due to SARS-CoV-2 have been thereafter reported.
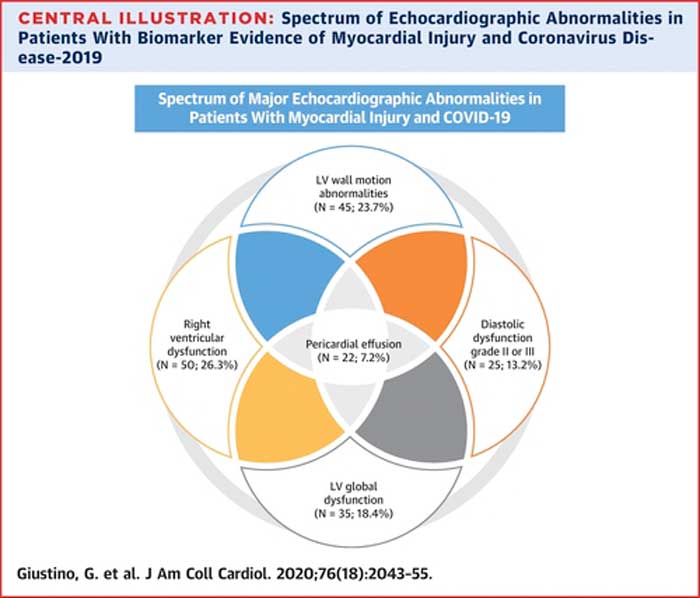
However, the immediate impact of Covid-19 on the myocardium appears to be multifactorial, not only dependent to cardiomyocites infection, with different phenotypes that could represent potentially different pathophysiological pathways of myocardial damage - i.e. left ventricular wall motion abnormalities, global left ventricular dysfunction, diastolic dysfunction, right ventricular dysfunction, and pericardial effusion (Figure 1).
Figure 1. Spectrum of Echocardiographic Abnormalities in Patients With Biomarker Evidence of Myocardial Injury and Coronavirus Disease-2019 (Giustino G et al. J Am Coll Cardiol 2020).
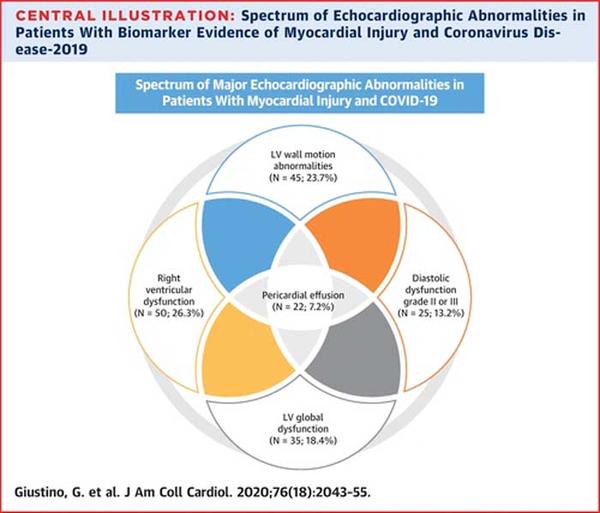
Source: JAAC Journals
The acute cardiac involvement during Covid-19 has been largely managed conservatively, with a focus on medical management of symptoms and inflammation. The mid and long-term effects of Covid-19 cardiac involvement are largely unknown and currently subject to multiple investigations.
Systematic cardiac follow-up of patients who survived Covid-19 should be considered at this point in time, keeping an eye open on possible mid- and long-term cardiovascular complications.
Indirect effects of Covid-19
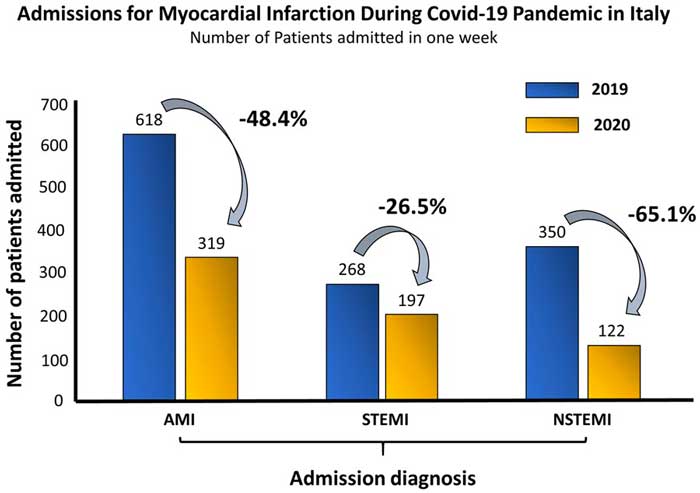
In the early phase of the Covid-19 pandemic, a number of reports raised the issue of a reduction of patients with acute myocardial infarction (AMI) accessing the Hospitals as compared to previous periods. In the absence of other competing mechanisms explaining the reduction in AMI, the observed phenomenon has been alarming.
Patients with acute AMI require prompt treatment with mechanical reperfusion of the occluded coronary artery. During the last 3 decades, AMI-networks have been developed worldwide in order to facilitate early diagnosis, optimizing system delays, and warrant timely reperfusion in patients with AMI. A reduction in the efficiency of these networks has expectedly important socio-economical consequences, translating into increased cardiovascular morbidity and mortality as well as healthcare costs.
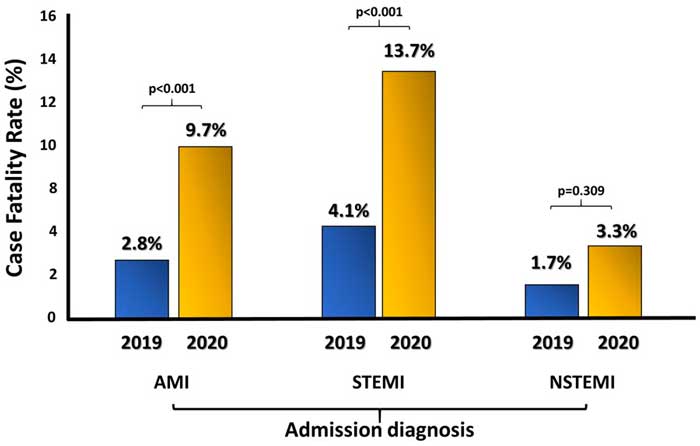
Unsurprisingly, surveys specifically documenting the decrease in AMI patients admitted in the pandemic period showed a parallel marked increase in the case fatality rate and in the number of out-of-hospital cardiac arrests as compared with the pre-pandemic period (Figure 2).
Figure 2. Reduction in AMI access to hospitals along with the increase in case fatality rate (De Rosa S et al. Eur Heart J 2020).
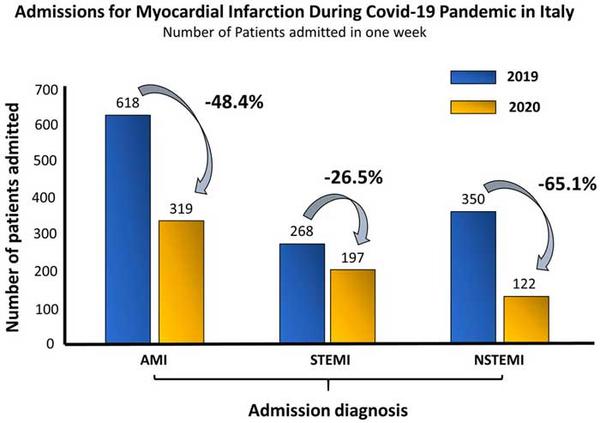
Source: European Heart Journal
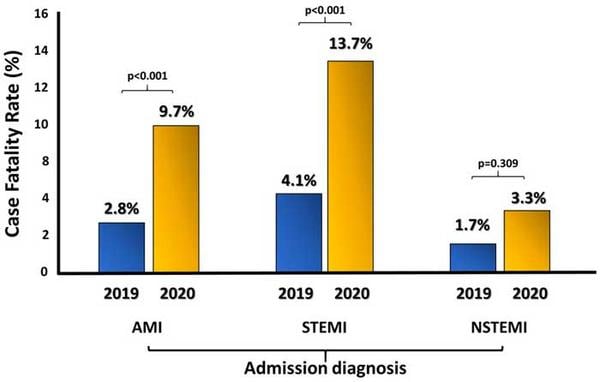
Source: European Heart Journal
The key question is what have been the barriers for patients to access the AMI-network during the early phase of the pandemic?
A number of speculations have been made in this regard. Certainly the state of emergency due to the pandemic has determined a reallocation of resources towards the management of patients with Covid-19 in the hospital setting. In some jurisdictions, this determined the reorganization of regional healthcare systems with a substantial reduction in the number of hospitals delivering care for patients with AMI - which certainly has had an impact on timely access to care.
In addition, a psychological aversion to seeking medical advice might have played a role. Hospitals were largely presented as the sites at high risk of SARS-CoV-2 infection, and patients with AMI symptoms might not have sought assistance in the fear of the contagion.
This phenomenon has determined a social cost in terms of increased cardiovascular mortality during the early phase of the Covid-19 pandemic. However, a potentially larger cost could be paid in the future to the mid- and long-term cardiovascular complications in patients who survived a potentially inadequately treated AMI. In this perspective, the management of chronic coronary syndromes with advanced coronary artery disease and heart failure will need adequate resources in the upcoming years.
Effects of Covid-19 on healthcare provision for patients with chronic cardiovascular conditions
The reallocation of resources to the emergency management of Covid-19 had also major implications on healthcare provision for patients with chronic cardiovascular diseases.
In many hospitals, elective cardiovascular procedures were delayed for several weeks or months, alternatively, the interventions were prioritized based on the patient’s risk profile and clinical status.
Local algorithms were developed to warrant care to patients with chronic coronary artery or valve disease on the waiting list becoming clinically or hemodynamically unstable. Limited availability of intensive care unit beds, largely utilized for Covid-19 patients, determined a larger use of percutaneous therapies for patients normally candidate to surgery: e.g. multivessel PCI were performed in patients candidate to CABG, while TAVI was proposed more often for patients candidate to SAVR.
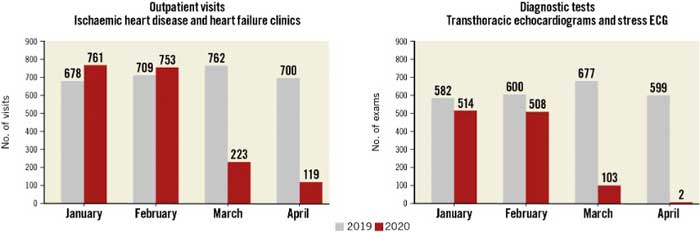
In addition, outpatient visits for ischaemic heart disease and heart failure were largely reduced (Figure 3).
Figure 3. Number of outpatient visits (left panel) and diagnostic tests (right panel) performed in patients with chronic cardiovascular diseases (i.e., ischaemic heart disease and heart failure) at the Cardiovascular Department of IRCCS Humanitas Research Hospital in Milan, Italy, between January-April 2019 and January-April 2020 (Holmes DR et al. EuroIntervention 2020).
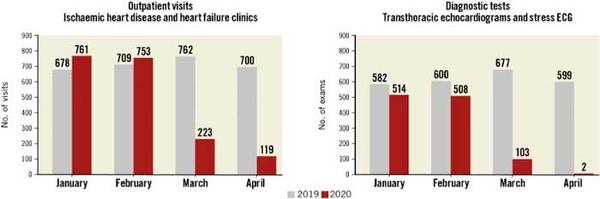
Source: EuroIntervention Journal
The impact on cardiovascular diseases of this reduction in healthcare provision will be measured by the increase in patients requiring visits, diagnostic tests, medical management, and invasive treatment in the upcoming months. It will be interesting to fully evaluate the societal, economical, and medical costs of these indirect effects of the Covid-19 pandemic.
Covid-19 related opportunities and future outlook
After an initial period of uncertainty and unpreparedness, healthcare systems have responded to the unmet clinical need of those stable patients kept out of the hospitals by boosting the adoption of e-Health and telemedicine.
Telephone and virtual consultations have significantly contributed, based on the referred symptoms, to timely identify those patients in need of diagnostic examinations or hospital admission, and to assist in some cases by remote management of milder clinical conditions.
Follow-up visits after cardiovascular interventions in hub centers were regularly performed by remote or coordinated with the support of local hospitals or ambulatory systems.
The changing pattern of access to the healthcare systems adopted during the pandemic is likely going to stay in consideration of the growing number of elderly patients in our societies.
The latter might be either in need of assistance for transportation to the outpatient clinics or at higher risk of hospital infection.
E-monitoring and telemedicine might ease the management of conditions like atrial fibrillation and heart failure beyond the pandemic period. Programs of home-based cardiac rehabilitation might warrant the achievement of secondary prevention targets with related improvement in quality of life and reduced cardiovascular morbidity and mortality.
Conclusion
Overall, the Covid-19 pandemic has changed our societies with a major impact on healthcare systems, by exposing their gaps. Recognising these gaps will undoubtedly open a window of opportunity to improve the intersection between health and society. Since cardiovascular diseases remain the first cause of death worldwide, obtaining an increase in the societal and economical resources for cardiovascular prevention is of paramount importance and, therefore, must be the primary goal to achieve by the end of the pandemic.
Authors





1 comment
The WHF, the ESC, with all their communities, infact, all health care professionals globally, WHO, being the payoneer, since the energence of COVID 19 pandemic virus, have been restless, in research study findings, vaccine manufacturing,, and truals to put an end to this human messile, the pandemic virus, that had claimed lives and properties globally, they have not relent their efforts, many physicians lost their lives to save humanity from this pandemic virus, many have retired from their practice, many have committed suicide due to some human error in their practice, jobs lost, organizations closed up, all aspects of human endeavors had been touched by this COVID 19 pandemic virus with negative impact. Resources had been pumpped into the health sector by all well known economics of the world , to arrest this pandemic, and put an end to it. However, I commend WHF, ESC, Medscape LLC. Kaplan medicals, and so many other pharmaceuticals for their professionalism and commitment to reduce the burden on the global economy, and the entire community of humanity. Dr. ALBERT NWANNE NKWOR.