ESC Practice Guidelines 2024: chronic coronary syndromes
Reported from ESC Congress 2024
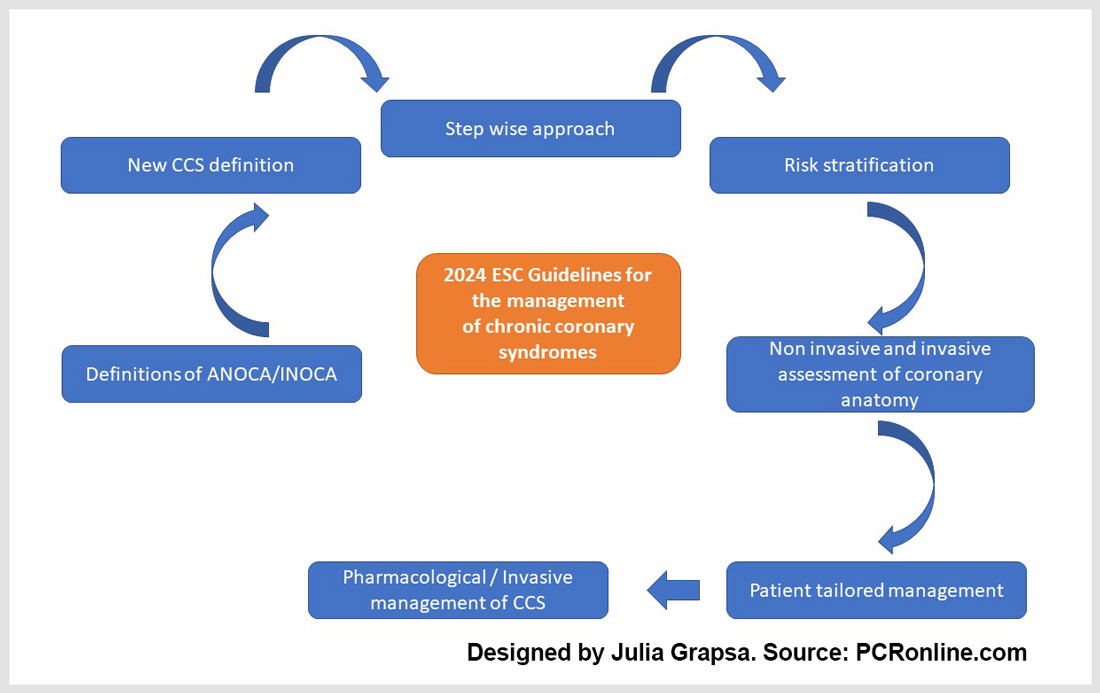
Julia Grapsa provides her take on the Chronic Coronary Syndromes (CCS) Guidelines which were presented by Felicita Andreotti and Christiaan Vrints at ESC Congress 2024 in London.
The new 2024 CCS guidelines pay attention to the new definition of chronic coronary syndromes: a stepwise approach for diagnosis and management, a focus on history and risk stratification, and an appropriate diagnostic assessment of coronary disease, by balancing risk factors and LVEF, and they emphasize the importance of the Heart Team, as well as the patient-centered approach.
Designed by Julia Grapsa. Source: PCRonline.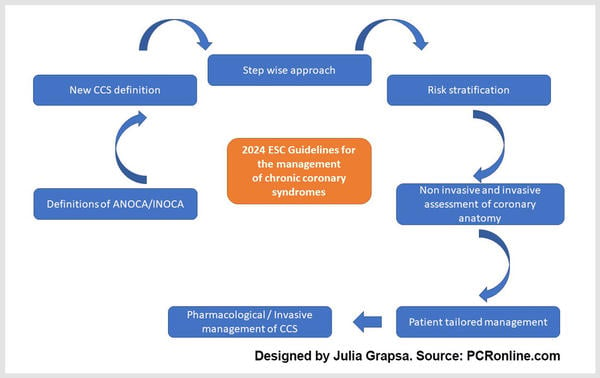
What are the key points to retain:
The authors pay attention to history taking and risk factor assessment and resting electrocardiogram in individuals with suspected CCS.
A detailed assessment of cardiovascular risk factors, medical history, and symptom characteristics is recommended as class Ic.
Symptoms like chest pain triggered by emotional stress, dyspnoea or dizziness on exertion, pain in the arms, jaw, neck, or upper back, or fatigue should be considered as potential angina equivalents (recommendation class IIaB).
Within the initial diagnostic management of individuals with suspected CCS, high-sensitivity C-reactive protein and/or fibrinogen plasma levels should be considered as IIaB.
It is recommended to estimate the pre-test likelihood of obstructive epicardial CAD using the Risk Factor-weighted Clinical Likelihood model (class Ib), while additional clinical data (e.g. examination of peripheral arteries, resting ECG, resting echocardiography, presence of vascular calcifications on previously performed imaging tests) is class Ic.
As a new part of the new ESC guidelines on CCS, ambulatory ECG monitoring should be considered in subjects with suspected vasospastic angina as class IIaB.
With regards to diagnostic imaging tests:
In individuals with suspected CCS and low or moderate (> 5 % – 50 %) pre-test likelihood of obstructive CAD, CCTA is recommended to diagnose obstructive CAD and to estimate the risk of MACE (class IA).
Stress echocardiography is the recommended test to diagnose myocardial ischaemia and to estimate the risk of MACE, as level IB, in patients with moderate or high (> 15 %– 85 %) pre-test likelihood of obstructive CAD. When two or more contiguous myocardial segments are not visualized, it is recommended to use intravenous ultrasound contrast agents to improve diagnostic accuracy – the latter is recommended to improve diagnostic accuracy and to refine risk stratification beyond wall motion (class IB).
In individuals with suspected CCS and moderate or high (> 15 % – 85 %) pre-test likelihood of obstructive CAD, SPECT or, preferably, PET myocardial perfusion imaging is also recommended (IB).
In individuals with suspected CCS and moderate or high (> 15 % – 85 %) pre-test likelihood of obstructive CAD, CMR perfusion imaging is recommended to diagnose and quantify myocardial ischaemia and/or scar and estimate the risk of MACE.
Invasive coronary assessment (ICA):
When this is indicated, radial artery access is recommended as the preferred access site (IA) and it is recommended to have coronary pressure assessment available, and to use it for functional severity of intermediate non-left main stem stenoses prior to revascularization.
In individuals with de novo symptoms highly suggestive of obstructive CAD that occur at a low level of exercise, ICA with a view towards revascularization is recommended as first diagnostic test after clinical assessment by a cardiologist.
The new guidelines provide certain thresholds for invasive indices for the epicardial arterial stenosis.
Suspected chronic coronary syndrome:
To rule out obstructive CAD in individuals with low or moderate (> 5 % – 50 %) pre-test likelihood, CCTA is recommended as the preferred diagnostic modality (IB). Invasive coronary angiography with the availability of invasive functional assessments is recommended to confirm or exclude the diagnosis of obstructive CAD or ANOCA/INOCA in individuals with an uncertain diagnosis on non-invasive testing (B).
An initial stratification of risk of adverse events is recommended based on basic clinical assessment (e.g. age, ECG, anginal threshold, diabetes, CKD, LVEF) (IB) – specific thresholds are mentioned under table 3 of the guidelines.
Patient-centered approach and the value of multidisciplinary discussion:
An informed discussion on CVD risk and treatment benefits tailored to individual patient needs is recommended (IC). It is recommended to tailor the selection of antianginal drugs to the patient’s characteristics, comorbidities, concomitant medications, treatment tolerability, and underlying pathophysiology of angina, also considering local drug availability and cost (IC). Ivabradine should be considered as add-on antianginal therapy in patients with left ventricular systolic dysfunction (IIaB).
When it comes down to lifestyle changes:
The most prominent recommendation (IA) is to adopt a multidisciplinary behavioural approach to help patients achieve healthy lifestyles, in addition to appropriate pharmacological management.
One step further, an informed discussion on CVD risk and treatment benefits tailored to individual patient is recommended as IC, while attention is paid to aerobic activity (IB) home-based cardiac rehabilitation and mobile health interventions (IIaB) which should be considered to encourage long term adherence and to reduce hospitalisations.
With regards to pharmacological treatment, it is recommended to tailor the selection of antianginal drugs to the patient’s characteristics, comorbidities, concomitant medications, treatment tolerability, and underlying pathophysiology of angina, also considering local drug availability and cost (IC).
Ivabradine is important as add-on antianginal therapy in patients with LVEF < 40 % inadequate control of symptoms, or as part of initial treatment in properly selected patients (IIa B).
In terms of antithrombotic therapy, in CCS patients with a prior MI or PCI, clopidogrel 75 mg daily is recommended as a safe and effective alternative to aspirin monotherapy (IA), and after CABG, aspirin 75–100 mg daily is recommended lifelong (IA) as well to those patients without prior MI or revascularization but with evidence of significant obstructive CAD (IB).
Lipid-lowering treatment with an LDL-C goal of 1.4 mmol/L (55 mg/dL) and a > 50 % reduction in LDL-C vs baseline is recommended as IA, while bempedoic acid is recommended as IB in statin-intolerant patients.
Important change in the new CCS guidelines is the implementation of SGLT2 inhibitors as IA, which are recommended in patients with T2DM and CCS to reduce CV events, independent of baseline or target HbA1c and independent of concomitant glucose-lowering medication.
Revascularization in patients with chronic coronary syndrome:
The new guidelines suggest that, when CABG and PCI hold the same level of recommendation, a Heart Team discussion is recommended, including representatives from interventional cardiology, cardiac surgery, non-interventional cardiology, and other specialties if indicated, aimed at selecting the most appropriate treatment to improve patient outcomes and quality of life (Ic).
Furthemore, they suggest a patient-centered approach considering, when possible, patient preferences, health literacy, cultural circumstances, and social support (Ic).
In CCS patients with LVEF ≤ 35 %, it is recommended to choose between revascularization or medical therapy alone, after careful evaluation, preferably by the Heart Team, of coronary anatomy, correlation between coronary artery disease and LV dysfunction, comorbidities, life expectancy, individual risk-to-benefit ratio, and patient perspectives (Ic).
When balancing procedural risks and post procedural outcomes, intracoronary imaging guidance by IVUS or OCT is recommended for performing PCI on anatomically complex lesions, in particular left main stem, true bifurcations and long lesions (IA).
It is striking that for left main disease, in CCS patients at low surgical risk with significant left main coronary stenosis, CABG is recommended over medical therapy alone to improve survival (Ia) and is recommended as the overall preferred revascularization mode over PCI, given the lower risk of spontaneous myocardial infarction and repeat revascularization (Ia).
In CCS patients with significant left main coronary stenosis of low complexity (SYNTAX score ≤ 22), in whom PCI can provide equivalent completeness of revascularization to that of CABG, PCI is recommended as an alternative to CABG, given its lower invasiveness and non-inferior survival.
In terms of management of CCS patients, in heart failure patients with LVEF ≤ 35 % in whom obstructive CAD is suspected, ICA is recommended with a view towards improving prognosis by CABG, taking into account the risk-to-benefit ratio of the procedures (Ib) while in patients with LVEF > 35 % and suspected CCS with low or moderate (> 5 % – 50 %) pre-test likelihood of obstructive CAD, CCTA or functional imaging is recommended (Ic).
The authors recommend that CCS patients with heart failure be enrolled in a multidisciplinary heart failure management programme to reduce the risk of heart failure hospitalization and to improve survival (Ia) while sacubitril/valsartan is recommended as a replacement for an ACE-I or ARB in CCS patients as Ib.
A very important part of the new guidelines is dedicated to diagnosis and management of patients with angina/ischaemia with non-obstructive coronary arteries. The authors emphasize to always take into consideration ANOCA/INOCA and as IA class for the treatment of isolated vasospastic angina calcium channel blockers are recommended to control symptoms and to prevent ischaemia and potentially fatal complications.




No comments yet!