Impact of anesthesia strategy and valve type on clinical outcomes after transcatheter aortic valve replacement
Selected in Journal of American College of Cardiology by M. Pighi
The current analysis aimed to compare the safety and efficacy of the Edwards Sapien S3 and Medtronic Corevalve. Furthermore, conscious sedation (CS) and local anaesthesia have been reported to reduce adverse events compared to general anaesthesia (GA) in several observational studies, with a lack of randomised trials.
References
Authors
Hans-Josef Feistritzer, Thomas Kurz, Georg Stachel, Philipp Hartung, Philipp Lurz, Ingo Eitel, Christoph Marquetand , Holger Nef, Oliver Doerr, Ursula Vigelius-Rauch, Alexander Lauten, Ulf Landmesser, Sascha Treskatsch, Mohamed Abdel-Wahab, Marcus Sandri, David Holzhey, Michael Borger, Jörg Ender, Hüseyin Ince, Alper Öner, Roza Meyer-Saraei, Rainer Hambrecht, Harm Wienbergen, Andreas Fach, Thomas Augenstein, Norbert Frey, Inke R König, Reinhard Vonthein, Anne-Kathrin Funkat, Astrid E Berggreen, Matthias Heringlake, Steffen Desch, Suzanne de Waha-Thiele, Holger Thiele, SOLVE-TAVI Investigators
Reference
10.1016/j.jacc.2021.03.007
Published
May 2021
Link
Read the abstractReviewer
My Comment
Why this study? – the rationale/objective
Transcatheter aortic valve replacement (TAVR) is an established therapy for elderly patients with severe symptomatic aortic stenosis at all surgical risk categories. With the expansion of TAVR procedures to younger low-risk populations, long-term data on the safety and efficacy of transcatheter heart valves become even more important. With this purpose, the current analysis aimed to compare the safety and efficacy of the Edwards Sapien S3 and Medtronic Corevalve. Furthermore, conscious sedation (CS) and local anaesthesia have been reported to reduce adverse events compared to general anaesthesia (GA) in several observational studies, with a lack of randomised trials.
How was it executed? – the methodology
- A 2x2 investigator-initiated multicentre non-inferiority randomised clinical trial.
- 447 all-comers patients randomized in a 1:1 fashion to
- a new-generation self- (SEV; Evolut R, Medtronic Cardiovascular; n = 219) versus balloon-expandable (BEV; Sapien 3, Edwards Lifesciences; n = 219) valves,
- and general (n = 220) versus local (n = 218) anesthesia.
- Patients included were all-comers with symptomatic severe aortic stenosis, adequate transfemoral access, age ≥ 75, and high-risk score for conventional surgical aortic valve replacement (STS ≥ 10 %).
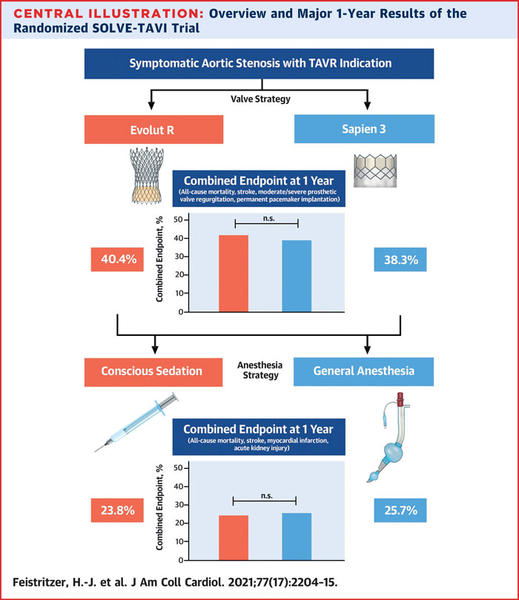
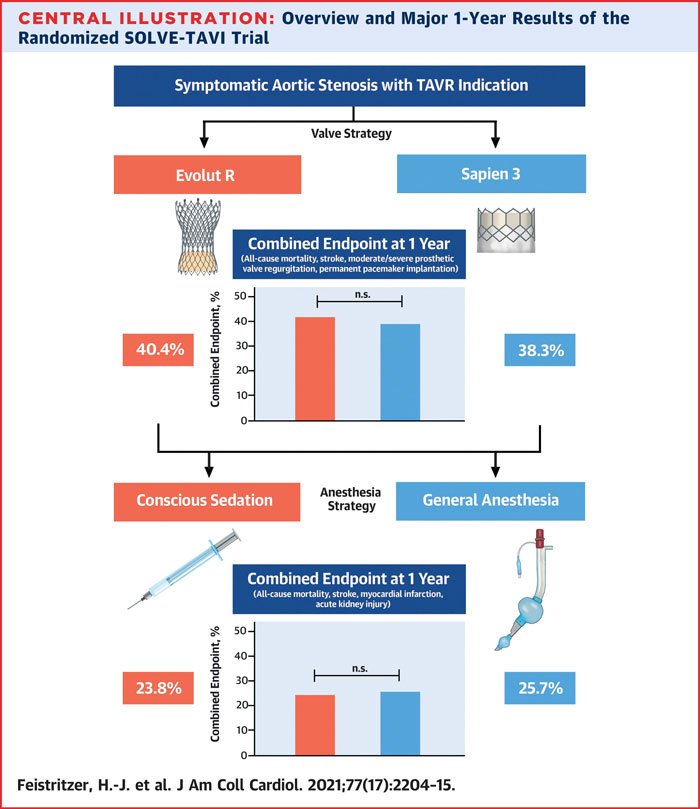
- The primary composite endpoint for the valve strategy analysis was 1-year all-cause death, stroke, moderate-to-severe regurgitation, or permanent pacemaker implantation, while for the anaesthesia strategy was a combined endpoint of all-cause mortality, stroke, myocardial infarction, and acute kidney injury.
What is the main result?
- In the valve-comparison strategy, the rates of combined endpoint were similar between BEV and SEV (38.3 % vs 40.4 %; HR 0.94; 95 % CI: 0.70-1.26; p = 0.66), with a higher stroke rate in BEV group compared with SEV (6.1 % vs 0.8 %; HR 6.63; 95 % CI: 1.50-29.2; p = 0.013). At the echocardiographic 1-year follow-up, the BEV group showed higher mean and maximum valve gradients.
- In the anaesthesia comparison strategy, the rates of combined endpoint were similar between GA and CS (25.7 % vs 23.8 %; HR 1.09; 95 % CI: 0.76-1.57; p = 0.63). However, according to a landmark analysis of events occurring between 30-day and 1-year, the combined endpoint occurred significantly more often in the GA group (22.0 % vs 14.6 %, p = 0.027).
Source: JACC
Critical reading and the relevance for clinical practice:
This report represents the largest prospective head-to-head comparison between the two commercially available contemporary TAVR prostheses. The results showed that both the Edwards Sapien S3 valve and Medtronic CoreValve Evolut R have equivalent clinical outcomes at 1-year follow-up, considering an all-comers intermediate-to-high-risk TAVR population (STS score 4.8 %), with a prevalence of frailty of 40 %.
The incidence of stroke was significantly higher in the BEV group (6.1 %) than SEV (0.8 %), with a similar stroke incidence in landmark analysis between 30 days and 1 year, with a consequent difference attributable to events occurring during or early after the procedure. Stroke rate in BEV treated patients was higher compared to previously reported data (2.7-4.6 %)1, but CHOICE and SCOPE I trials have already shown a trend towards a higher incidence of stroke in BEV as compared to SEV treated patients2,3. A clear causal explanation of these data is not provided by the authors, with a potential role of balloon pre-dilatation, used in 39.8 % of overall patients, that was numerically more frequent in those with stroke than in those without.
The 1-year rate of permanent pacemaker (PPM) implantation was similar in the two groups (24.5 % for SEV vs 20.0 % for BEV; p = 0.24). In addition, the rate of PPM implantation for SEV was similar to the previously reported data in the FORWARD study (22.1 %)4. In contrast, in the current analysis, an 8 % higher rate of PPM implantation was described in the population treated with BEV compared to previous studies.
The trial also shows no difference in adverse events between conscious sedation and general anaesthesia for TAVR, with no differences in all-cause mortality, stroke, myocardial infarction, and acute kidney injury. National registries worldwide have shown a progressive transition from a GA standard protocol to CS. Nowadays, most high-volume academic centres seem to apply local anaesthesia or CS5. Previous confirmed that TAVR under LA or CS was as effective and safe as under GA with favourable effects in procedural time, less use of inotropic agents, shorter hospital stay, and lower costs6. However, despite the theoretical advantage of CS over GA on procedural and short-term results, no evidence of improvement in the efficacy endpoints has been reported in randomised clinical trials. In the 30-day sub-analysis of the SOLVE-TAVI trial, a similar incidence of all-cause mortality, myocardial infarction, infection requiring antibiotics, and AKI were described. The study showed a lower need for inotropes and vasopressors with CS (62.8 %) versus GA (97.3 %), suggesting CS can be safely applied for TAVR procedures.
References:
- Wendler O, Schymik G, Treede H, Baumgartner H, Dumonteil N, Neumann FJ, Tarantini G, Zamorano JL, Vahanian A. SOURCE 3: 1-year outcomes post-transcatheter aortic valve implantation using the latest generation of the balloon-expandable transcatheter heart valve. Eur Heart J. 2017;38:2717–26.
- Abdel-Wahab M, Mehilli J, Frerker C, Neumann FJ, Kurz T, Tölg R, Zachow D, Guerra E, Massberg S, Schaf̈er U, El-Mawardy M, Richardt G. Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcatheter aortic valve replacement: The CHOICE randomised clinical trial. JAMA - J Am Med Assoc. 2014;311:1503–14.
- Lanz J, Kim WK, Walther T, Burgdorf C, Möllmann H, Linke A, Redwood S, Thilo C, Hilker M, Joner M, Thiele H, Conzelmann L, Conradi L, Kerber S, Schymik G, Prendergast B, Husser O, Stortecky S, Heg D, Jüni P, Windecker S, Pilgrim T. Safety and efficacy of a self-expanding versus a balloon-expandable bioprosthesis for transcatheter aortic valve replacement in patients with symptomatic severe aortic stenosis: a randomised non-inferiority trial. Lancet. 2019;394:1619–28.
- Manoharan G, Van Mieghem NM, Windecker S, Bosmans J, Bleiziffer S, Modine T, Linke A, Scholtz W, Chevalier B, Gooley R, Zeng C, Oh JK, Grube E. 1-Year Outcomes With the Evolut R Self-Expanding Transcatheter Aortic Valve: From the International FORWARD Study. JACC Cardiovasc Interv. 2018;11:2326–34.
- Patel PA, Ackermann AM, Augoustides JGT, Ender J, Gutsche JT, Giri J, Vallabhajosyula P, Desai ND, Kostibas M, Brady MB, Eoh EJ, Gaca JG, Thompson A, Fitzsimons MG. Anesthetic Evolution in Transcatheter Aortic Valve Replacement: Expert Perspectives From High-Volume Academic Centers in Europe and the United States. J Cardiothorac Vasc Anesth. 2017;31:777–90.
- Butala NM, Chung M, Secemsky EA, Manandhar P, Marquis-Gravel G, Kosinski AS, Vemulapalli S, Yeh RW, Cohen DJ. Conscious Sedation Versus General Anesthesia for Transcatheter Aortic Valve Replacement: Variation in Practice and Outcomes. JACC Cardiovasc Interv. 2020;13:1277–87.






No comments yet!