Moderate aortic stenosis in patients with heart failure and reduced ejection fraction
Selected in Journal of the American College of Cardiology by L. Biasco
The aim of this study was to determine the prognostic impact conferred by the presence of moderate AS on the outcomes of patients with HFrEF.
References
Authors
Guillaume Jean, Nicolas M. Van Mieghem, Tea Gegenava, Lennart van Gils, Jeremy Bernard, Marcel L. Geleijnse, E. Mara Vollema, Ikram El Azzouzi, Ernest Spitzer, Victoria Delgado, Jeroen J. Bax, Philippe Pibarot, and Marie-Annick Clavel
Reference
J Am Coll Cardiol. 2021 Jun, 77 (22) 2796–2803
Published
June 2021
Link
Read the abstractReviewer
Latest contributions
TAVI complications - Part 5 Unusual structural interventions: infective endocarditis, ventricular septal rupture & hypertrophic obstructive cardiomyopathy Tendyne transcatheter mitral valve system in patients with severe mitral annular calcification: one-year outcomes from the SUMMIT Severe MAC cohortMy Comment
Why this study? – the rationale/objective
Choice of the correct timing to refer patients with aortic stenosis (AS) for treatment is a complex clinical decision. So far the paradigm that predominantly symptomatic patients with ascertained severe AS (and all its relative declinations) would represent candidates adequately balancing procedural risks with benefits derived from the resolution of the valvular disease has been the lighthouse that guided our choiches.
This paradigm might not apply to all patients. Patients with heart failure with reduced ejection fraction (HFrEF) might represent an exception. In those patients, lower degrees of aortic stenosis, with its associated increased overaload, might represents an additional prognostic factor on top of a reduced ejection fraction, thus becoming a potential target for treatment.
The aim of the article by Dr. Jean et al was to determine the prognostic impact conferred by the presence of moderate AS on the outcomes of patients with HFrEF.
Source: JACC
How was it executed? – the methodology
Study population, retrospective study design:
- Cases: 262 patients with HFrEF (LVEF < 50%) and moderate aortic stenosis (defined as an aortic valve area [AVA] >1.0 and <1.5 cm2 and peak aortic jet velocity >2 and <4 m/s) enrolled in three academic centers between Canada and the Nederlands.
- Controls: 262 matched patients with HFrEF (LVEF < 50%) but without AS (peak velocity < 2 m/s without echocardiographic abnormalities of aortic leaflets) evaluated between 2010 and 2015.
Endpoints:
- Primary: all-cause mortality after diagnosis.
- Secondary: composite of hospitalization for heart failure (HF) and all-cause mortality.
Survival status was assessed from the respective national registries.
Cumulative mortality was assessed by the Kaplan Meier method while associations between outcomes and clinically relevant cofactors estimated by means of multivariate Cox Proportional hazard adjusted analyses
What is the main result?
- Patients with HFrEF and AS had a mean LVEF of 38.5 ± 9.6 % and a AVA of 1.24 ± 0.17 cm2 while patients without AS had a significantly lower LVEF of 36.6 ± 7.5% while AVA of 2.51 ± 0.58 cm2.
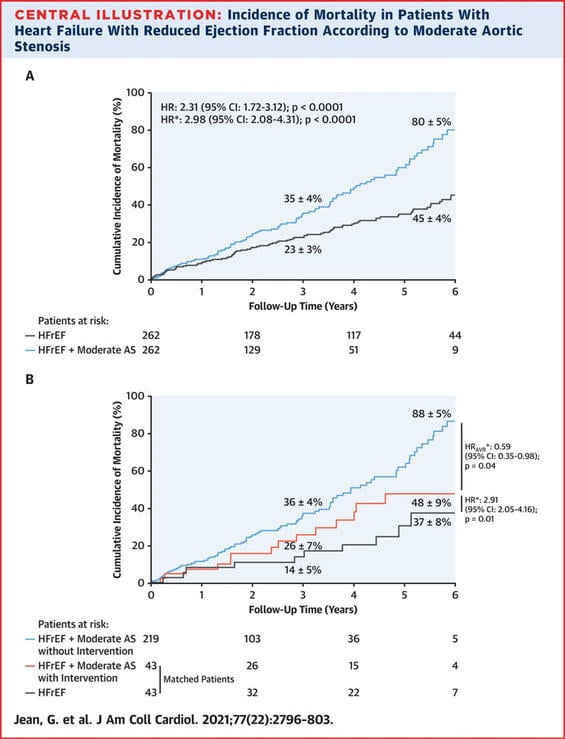
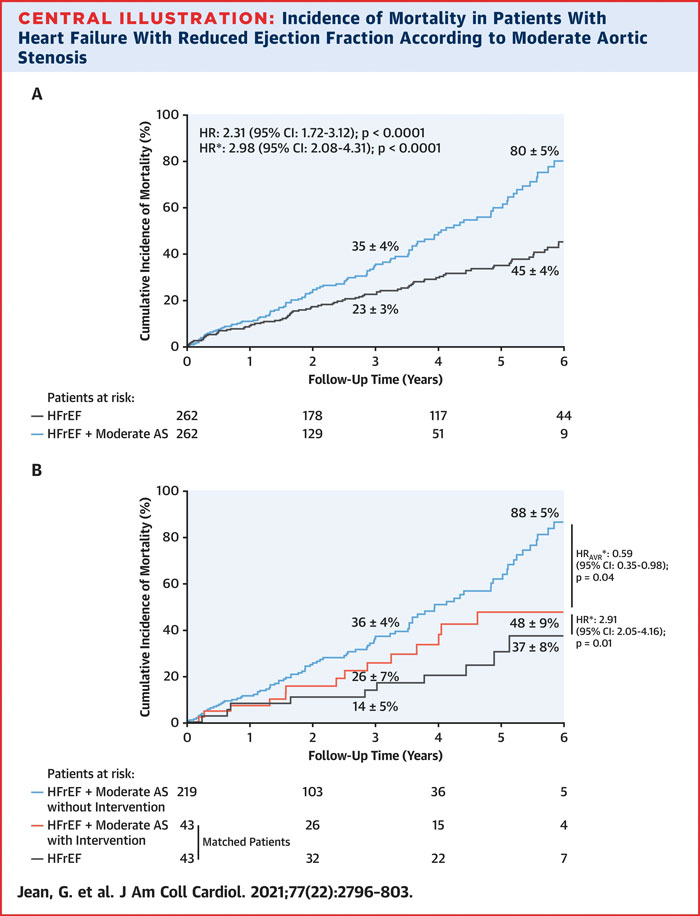
- Cumulative all-cause mortality occurred at 3 years in 35% of patients with HFrEF and moderate AS while only in 23% in HFrEF controls (80% vs 45% at 6 years follow-up; p<0,001).
- Secondary endpoint occurred at 3 years in 47% of patients with HFrEF and moderate AS while in 35% in HFrEF controls (94% vs 57% at 6 years follow-up; p<0,001).
- At a mean follow up of 2.9±2.2 years, at multivariable analysis presence of moderate AS was the strongest independent predictor of the primary (adjusted hazard ratio (HR) 2.98, 95% CI: 2.08 to 4.31; p < 0.0001) and secondary (adjusted HR 2.34, 95% CI: 1. 72 to 3.21; p < 0.0001).
- During follow up a very small group (n= 44 patients) in the moderate AS group underwent aortic valve replacement by surgical (n=29) or transcatheter interventions (n=15). Correction of the valvular disease was able to reduce by 40% the risk of mortality at follow up (HR 0.59, 95% CI: 0.35-0.98; p = 0.04) with an signal suggesting a better survival benefit evident for transcatheter interventions but not for surgery. Nonetheless the available follow up for this subgroup was extremely short (10.9 months).
Critical reading and the relevance for clinical practice:
The classical approach to consider valvular heart diseases, and aortic stenosis in particular, not as a continuum but rather as a black or white condition where treatments might be reserved to patients with severe diseases will probably be challenged in the next future. Evidence is accumulating on the detrimental prognostic impact of even lower degrees of valvular diseases, in particular on the role of moderate AS.
This retrospective analysis, even if biased by the intrinsic limitations evident from the study design (e.g. the relatively small sample size, the lack of data regarding ICD therapies, the unclear matching process and the unplanned subanalysis on patients treated with AVR) provides a clear signal indicating the possibility for a potential paradigm shift in the next future.
While a detrimental prognostic impact of moderate AS with a progressive increase in the risk of mortality with a threshold around mean AV gradient of 20.0 mm Hg and an equivalent peak AV velocity of 3.0 m/s was observed in a large retrospective analysis by Strange et al. published in JACC in 2019, the analysis by Jean et al. clearly shows that presence of even moderate AS might independently impact on the prognosis of patients with impaired LV function. In addition, the signal indicating that AVR might favourably impact on outcomes, while being far from being conclusive, is surey hypothesis generating. Clearly, evidences deriving from the present analysis are not still enough to justify aortic valve replacement in patients with moderate AS and reduced LVEF, nonetheless this manuscript stresses the concept of valvular diseases as a continuum and with a progressive impact on outcomes.
In addition, authors suggest the logical, but still not evidence supported, concept that different rules might apply to patients with a failing left ventricle. Patients with reduced LV functions might have a reduced reserve not able to tolerate even a modest increase in the left ventricular afterload caused by the presence of a moderately stenotic aortic valve. Thus, lower thresholds for interventions might apply to this peculiar patient’s subgroups.
So far both European and American guidelines supported with low class of recommendation and level of evidence the treatment of moderate AS only when other cardiac surgery needed, data derived from this analysis and the ongoing TAVR-UNLOAD RCT comparing TAVI+OMT vs OMT alone in patients with HF and moderate AS will probably change our perspective in the next future.






No comments yet!