27 Jan 2022
Cardiohepatic syndrome is associated with poor prognosis in patients undergoing tricuspid transcatheter edge-to-edge valve repair
Selected in JACC: Cardiovascular Interventions by J. Curio , G. Tang
As the prognostic role of cardiohepatic syndrome (CHS) has not yet been evaluated, Stolz et al. in the present study assessed its impact on T-TEER outcomes.
References
Authors
Lukas Stolz, Mathias Orban, Christian Besler, Karl-Patrik Kresoja, Daniel Braun, Philipp Doldi, Martin Orban, Christian Hagl, Karl-Philipp Rommel, Julia Mayerle, Sebastian Hausleiter, Kornelia Löw, Satoshi Higuchi, Mirjam Wild, Matthias Unterhuber, Steffen Massberg, Michael Näbauer, Holger Thiele, Philipp Lurz, Jörg Hausleiter
Reference
J Am Coll Cardiol Intv. 2022 Jan, 15 (2) 179-189
Published
January 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
Increased awareness for tricuspid regurgitation (TR) as independent predictor of morbidity and mortality in recent years led to the development of several transcatheter treatment devices. Currently, tricuspid transcatheter edge-to-edge repair (T-TEER) is the most commonly performed and best studied of these approaches1.
TR, if left untreated, leads to chronic venous congestion, impairing the function of metabolic organs such as the liver. This congestive stress promotes an increase of cholestatic parameters and, especially in the case of concomitant reduced left ventricular function with decreased arterial hepatic perfusion, also an increase of serum liver parameters.
Several clinical factors like NYHA functional class, kidney function, and pulmonary hypertension may be used as predictors of T-TEER outcomes, while classic echocardiographic parameters of right or left ventricular function did not show predictive relevance2.
As the prognostic role of cardiohepatic syndrome (CHS) has not yet been evaluated, Stolz et al. in the present study assessed its impact on T-TEER outcomes.
How was it executed? - the methodology
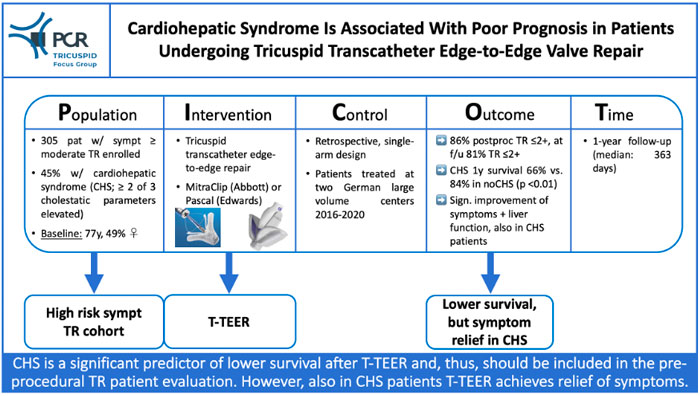
305 patients who underwent isolated T-TEER with either the MitraClip (Abbott Vascular) or the Pascal system (Edwards Lifesciences) between March 2016 and June 2020 at two large volume German centers were included. Patients with combined T-TEER and mitral transcatheter edge-to-edge repair were excluded to reduce the bias of decreased left ventricular function and secondary mitral regurgitation reducing cardiac output and liver perfusion.
Cholestatic parameters, i.e. serum gamma glutamyl transferase (GGT), alkaline phosphatase (AP), and total bilirubin, as well as alanine aminotransferase (ALT) and aspartate aminotransferase (AST) as liver parameters were assessed at baseline. In line with previous reports, CHS resulting from TR was characterized as CHS type 2, namely CHS in the setting of chronically impaired cardiac function leading to chronic liver injury, defined by elevation of at least 2 of 3 cholestatic parameters3.
- Primary endpoint was 1-year all-cause mortality
- Secondary endpoints were: change in NYHA functional class, 6MWD, TR, and hospitalizations for heart failure during 12 months
- A Cox regression model was used to identify predictors of 1-year all-cause mortality
What is the main result?
49 % of patients were women, mean age was 77 years. TR was 3+ (severe) in 69 % and 4+ (massive or torrential) in 30 %, 89 % presented with NYHA functional class III/IV.
At baseline, 81 % showed elevated GGT, 26 % elevated bilirubin, 45 % elevated AP, 18 % elevated AST, and 6 % elevated ALT. Following the used definition, 45 % of patients suffered from CHS.
In 86 %, TR was reduced to ≤ 2+, at follow-up TR remained reduced in 81 %, 1-year survival was 76 %. 17 % were hospitalized for heart failure, and 74 % were in NYHA functional class ≤ II at follow-up.
Key findings regarding the role of CHS were:
- Patients with CHS at baseline presented with significantly reduced right (TAPSE) and left ventricular (LVEF) function, as well as higher degrees of TR
- Also in CHS patients T-TEER significantly reduced TR (83 % post-procedural TR ≤ 2+)
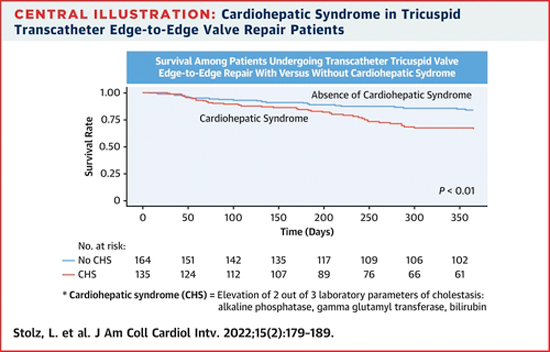
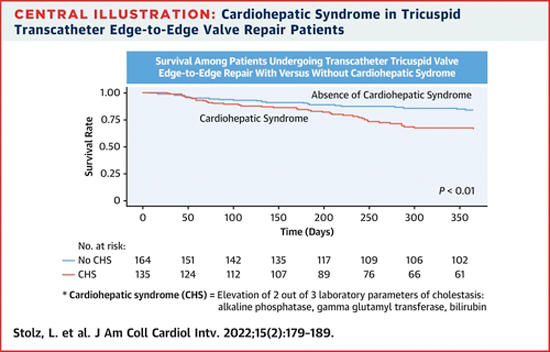
- 1-year survival was significantly lower in CHS patients (66 % vs. 84 % in no CHS); CHS (HR: 1.86, 95 % CI: 1.10-3.31, p = 0.02), creatinine, NYHA functional class IV, TR vena contracta, and post-procedural TR ≥ 3+ in multivariable Cox regression were independent predictors of mortality
- CHS patients experienced significantly more heart failure hospitalizations during 1 year, and, even though NYHA functional class significantly improved, CHS patients had a higher rate of NYHA functional class IV
- At follow-up, in patients with baseline impaired liver function, all laboratory liver parameters were significantly improved
Source: JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice
It is encouraging to see that, in such a large cohort, T-TEER enables profound and durable TR reduction, resulting in symptomatic benefits and measurable amelioration of liver failure - also in patients with CHS.
However, the significantly higher mortality in CHS patients prompts caution. Clinical as well as echocardiographic parameters suggest that CHS patients present at a later stage of disease where chronic heart failure already caused profound cardiac and non-cardiac damage. This adds to previous evidence showing that especially clinical factors (NYHA functional class IV, renal impairment, pulmonary hypertension) predict procedural outcomes following T-TEER, and intervention ideally should be performed at earlier disease stages before the onset of profoundly impaired organ function4.
Recently, several scoring systems to grade the severity of systemic disease and potential outcomes in TR patients were presented. The TRI-SCORE, based on over 450 patients undergoing isolated TR surgery in France, incorporates eight easily assessable parameters to predict in-hospital mortality5. In terms of US data, Gorav Ailawadi at TCT 2021 presented a clinical risk score based on the STS database, predicting mortality and major morbidity, potentially enabling identification of a cohort C, in which intervention might come too late. However, both these scoring systems do not include liver function. Here, the study by Stolz et al. raises important awareness, highlighting liver function as a critical parameter and potential indicator of progressed disease resulting in limited therapeutic effects.
Such assessment of disease stages and their impact on outcomes following T-TEER needs to be evaluated in the setting of randomized trials. Indeed, for the TriClip device, the TRILUMINATE Pivotal Trial (ClinicalTrials.gov Identifier: NCT03904147) as well as the TRI-FR study (ClinicalTrials.gov Identifier: NCT04646811) and for the Pascal device the Clasp II TR trial (ClinicalTrials.gov Identifier: NCT04097145) are currently enrolling patients. The data of these trials will allow us to further understand how different degrees of liver dysfunction impact hard endpoints.
In the meantime, the study by Stolz et al. gives important input for heart-teams evaluating TR patients for intervention: the take-home message of this study is that, while T-TEER might ameliorate liver function also in CHS patients, distinct evaluation of liver dysfunction should be integrated into the pre-procedural patient evaluation, as this potentially helps to identify patients at later disease stages with impaired treatment response.
Picot scheme highlighting key aspects of the study. Source: courtesy of Jonathan Curio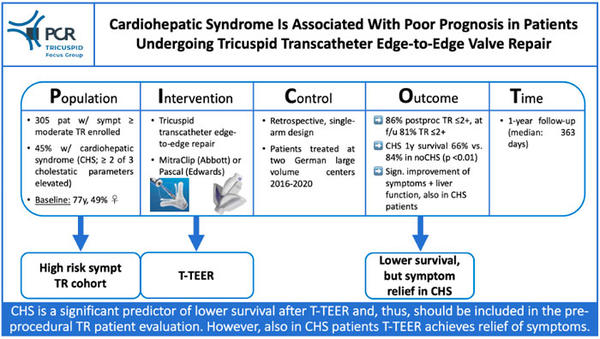
References
- Lurz, P., Stephan von Bardeleben, R., Weber, M., et al. "Transcatheter Edge-to-Edge Repair for Treatment of Tricuspid Regurgitation." J Am Coll Cardiol 2021;77:229-239.
- Karam, N., Mehr, M., Taramasso, M., et al. "Value of Echocardiographic Right Ventricular and Pulmonary Pressure Assessment in Predicting Transcatheter Tricuspid Repair Outcome." J Am Coll Cardiol Intv 2020;13:1251-1261.
- Poelzl, G., Auer, J. "Cardiohepatic syndrome." Curr Heart Fail Rep 2015;12:68-78.
- Praz, F., Muraru, D., Kreidel, F., et al. "Transcatheter treatment for tricuspid valve disease." EuroIntervention 2021;17:791-808.
- Dreyfus, J., Audureau, E., Bohbot, Y., et al. "TRI-SCORE: a new risk score for in-hospital mortality prediction after isolated tricuspid valve surgery." Eur Heart J 2021;ehab679