Prediction of death or HF hospitalization in patients with severe FMR: the COAPT risk score
Selected in JACC : Cardiovascular Interventions by M. Alasnag , H. Naung Tun
The new analysis from the COAPT trial indicated that lower secondary mitral regurgitation by TEER was strongly associated with reduced heart failure hospitalization, all-cause mortality, and improved quality of life as compared with a higher degree of residual MR.
References
Authors
Neeraj Shah, Mahesh V. Madhavan, William A. Gray, Sorin J. Brener, Yousif Ahmad, JoAnn Lindenfeld, William T. Abraham, Paul A. Grayburn, Saibal Kar, D. Scott Lim, Jacob M. Mishell, Brian K. Whisenant, Zixuan Zhang, Bjorn Redfors, Michael J. Mack, and Gregg W. Stone
Reference
J Am Coll Cardiol Intv. 2022 Oct, 15 (19) 1893–1905
Published
October 2022
Link
Read the abstractReviewers
Our Comment
Why this study – the rationale/objective?
Mitral regurgitation (MR) is the commonest valvular heart abnormality encountered in clinical practice globally1-2.
Over the last decade, the emerging role of catheter-based mitral intervention, such as transcatheter edge-to-edge rapier (TEER) technology, has been introduced for the repair of mitral regurgitation. Recently, some landmark studies on TEER have been published, including the Endovascular Valve Edge-to-Edge Repair Study II (EVEREST II), MitraClip Device for Severe Functional/Secondary Mitral Regurgitation (MITRA-FR) trial, and Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation (COAPT) and MitraClip Therapy Economic and Clinical Outcomes Study Europe (ACCESS-EU) trials3-6.
Such studies have proposed the feasibility and safety of TEER in interventional practice with respect to cardiovascular outcomes. The more contemporary landmark studies on catcher-based intervention for secondary MR in patients with symptomatic heart failure (HF) on guideline-directed medical therapy (GDMT), MITRA-FR, and COAPT trials, were debated extensively, owing to the different outcomes reported in these trials. The COAPT noted a lower rate of hospitalization for heart failure and lower all-cause mortality within 24 months of follow-up, with TEER plus GDMT than GDMT alone with a high rate of freedom from device-related complications. On the other hand, the rate of death or unplanned hospitalization for heart failure at 1 year in the MITRA-FR trial did not differ significantly between patients who underwent percutaneous mitral-valve repair and those who received GDMT alone. The difference was predominantly attributed to the baseline characteristics of the patients and inclusion criteria.
Despite invasive catheter-based interventions and optimal medical therapy for functional MR, patients with secondary MR and HF remain at increased risk of recurrent heart failure hospitalization and cardiovascular mortality. Interestingly, the new analysis from the COAPT trial indicated that lower secondary mitral regurgitation (SMR) by TEER was strongly associated with reduced heart failure hospitalization (HFH), all-cause mortality, and improved quality of life as compared with a higher degree of residual MR7.
How was it executed – the methodology?
Briefly, the sub-analysis from the COAPT trial enrolled symptomatic individuals with systolic HF (LVEF 20-50 %), 3 and 4+ MR, who were randomized to maximally titrated GDMT alone or TEER with MitralClip plus GDMT.
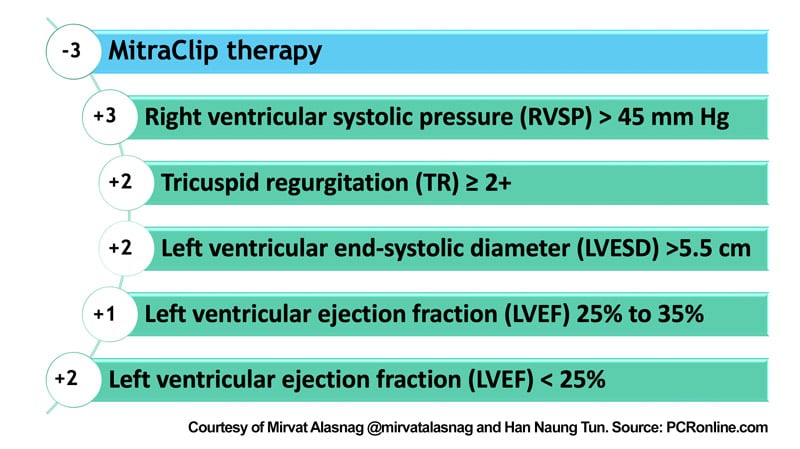
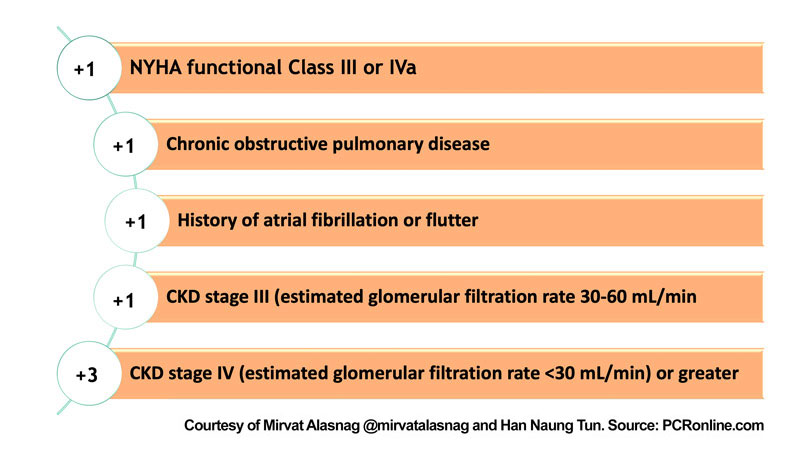
This study was the basis for the COAPT risk score, which consisted of 26 variables that included clinical presentation, echocardiographic parameters, and treatment variables. The score provides prognostic insights for patients with HF with 3 and 4+ MR. The total risk score can range from −3 to 15 points, shown in Figures 1 & 2.
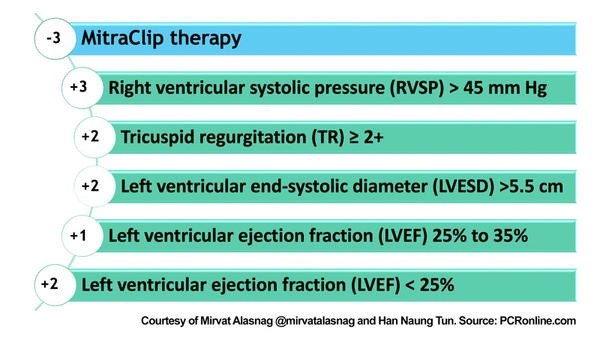
Figure 1: Echocardiographic components of the COAPT Score - figure courtesy of Mirvat Alasnag and Han Naung Tun
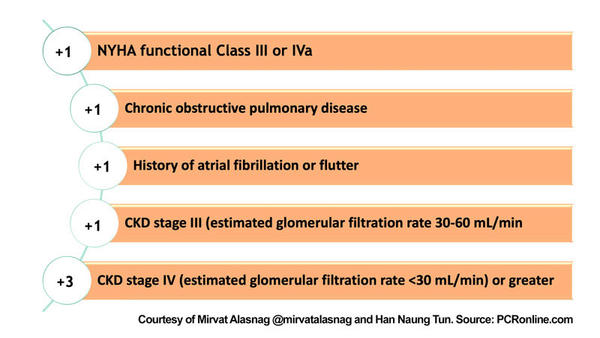
Figure 2: Clinical variables of the COAPT Score - figure courtesy of Mirvat Alasnag and Han Naung Tun
What is the main result?
During the 2-year follow-up, 201 (64.4 %) patients in the GDMT alone group and 133 (44.0 %) patients in the MitraClip group experienced the primary outcome (P < 0.001).
By multivariable analysis, the MitraClip treatment group was the strongest predictor of freedom from death or HF hospitalization (adjusted HR 0.56 ; 9 5% CI: 0.45-0.71, p < 0.001).
Other significant baseline predictors of death or HFH included NYHA III-IV functional class (HR 1.29 ; 95 % CI : 1.02-1.63 , p - 0.04), chronic kidney disease (CKD) with Creatinine Clearance ≤ 60ml/ min (HR: 2.03; 95 % CI: 1.36-3.01; P - 0.008), CKD stage IV or greater (eGFR < 30 mL/min) (HR: 2.03; 95 % CI: 1.36-3.01; P < 0.001), COPD ( HR 1.29 ; 95 % CI :0.96-1.74, p – 0.09) , history of atrial fibrillation or flutter (HR 1.27 ; 95 % CI : 0.97-1.68 , p -0.080) , estimated right ventricular systolic pressure (RVSP) >50 mm Hg (HR: 1.71; 95 % CI: 1.31- 2.22; P < 0.001), and the median value of left ventricular end-systolic dimension (LVESD) > 5.3 cm (HR 1.38 ; 95 % CI : 1.07-1.78 , p – 0.01).
Critical reading and relevance for clinical practice
In patients with HF and severe SMR, mitral-TEER significantly reduces HF hospitalizations or death at 2 years. Clinical CKD, NYHA 3-4 functional class, at least moderate tricuspid regurgitation, RVSP > 50 mm Hg, and LVESD > 5.3 cm predict a worse prognosis. Outcomes of the interventional trials largely depend on the underlying etiologies, co-morbidities, clinical presentations, cardiac imaging parameters of the participants, and operator performance of the procedures, which are too often overlooked when analyzing practice-changing studies. To date, no tool has been elaborated for mitral-TEER that included echocardiographic parameters other than the COAPT and MIDA scores. The MIDA score was derived from the Mitral Regurgitation International Database registries that weren’t designed for secondary MR.
As such, the COAPT score provides a need in clinical practice as the uptake of these therapies increases. As a tool, it appears simple and can prompt a multidisciplinary team discussion on management of these high-risk patients, and potentially identify those who wouldn’t benefit from device therapy.
It is important to note, that although there was a consistent reduction in the hazard of death across groups, it was greater in those with the greatest baseline risk. Overall, the COAPT score performed well, and the sensitivity analysis was reassuring; however, it lacks external validation. This is particularly important since the COAPT trial enrolled a 74 % white population of whom more than 60 % men. Several cohorts have been proposed, including those from the MitraSwiss registry or MITRA-FR study, yet these trials also included a predominantly male cohort (their ethnicity was not specified). In fact, Lung et al did such an analysis on MITRA-FR patients and revealed that COAPT-eligible patients in MITRA-FR tended to have better outcomes than did COAPT-ineligible patients8. Yet, these patients did not extract any additional benefit from TEER. MITRA-FR patients deemed COAPT eligible, had significantly different baseline characteristics making a post hoc analysis difficult to interpret and merely hypothesis generating.
Finally, a model that includes post-therapy assessment of residual MR and reduction in RVSP is attractive. This was not included in the current COAPT score. Despite any limitations, the COAPT score remains a valuable tool that is already unofficially applied to many patients assigned to mitral-TEER therapy. It would be interesting to revisit the performance of this score once externally validated. It would be equally valuable to understand how well the score performs for other transcatheter therapies beyond edge to edge repair such as transcatheter mitral valve replacement or annuloplasty.
References:
- Wu S, Chai A, Arimie S, Mehra A, Clavijo L, Matthews RV, Shavelle DM. Incidence and treatment of severe primary mitral regurgitation in contemporary clinical practice. Cardiovasc Revasc Med. 2018 Dec;19(8):960-963.
- Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368(9540):1005-1011. doi:10.1016/S0140-6736(06)69208-8.
- Mauri L, Garg P, Massaro JM, et al. The EVEREST II Trial: design and rationale for a randomized study of the evalve mitraclip system compared with mitral valve surgery for mitral regurgitation. Am Heart J. 2010;160(1):23-29. doi:10.1016/j.ahj.2010.04.009.
- Maisano F, Franzen O, Baldus S, et al. Percutaneous mitral valve interventions in the real world: early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe. J Am Coll Cardiol. 2013;62(12):1052-1061. doi:10.1016/j.jacc.2013.02.094.
- Obadia JF, Messika-Zeitoun D, Leurent G, et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. N Engl J Med. 2018;379(24):2297-2306. doi:10.1056/NEJMoa1805374.
- Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med. 2018;379(24):2307-2318. doi:10.1056/NEJMoa1806640.
- Kar S, Mack MJ, Lindenfeld J, et al. Relationship Between Residual Mitral Regurgitation and Clinical and Quality-of-Life Outcomes After Transcatheter and Medical Treatments in Heart Failure: COAPT Trial. Circulation. 2021;144(6):426-437. doi:10.1161/CIRCULATIONAHA.120.053061.
- Iung B, Messika-Zeitoun D, Boutitie F, Trochu JN, Armoiry X, Maucort-Boulch D, Obadia JF, Vahanian A. Characteristics and Outcome of COAPT-Eligible Patients in the MITRA-FR Trial. Circulation. 2020 Dec 22;142(25):2482-2484. doi: 10.1161/CIRCULATIONAHA.120.049743. Epub 2020 Dec 21.






No comments yet!