Transcaval versus transaxillary TAVR in contemporary practice - a propensity-weighted analysis
Selected in JACC: Cardiovascular Interventions by J. Curio , S. Brugaletta
As there has been no systematic comparison of transcaval and transaxillary access so far, the present study aimed to compare these two approaches with each other, as well as with transfemoral access.
References
Authors
Robert J. Lederman, Vasilis C. Babaliaros, John C. Lisko, Toby Rogers, Paul Mahoney, Jason R. Foerst, Jeremiah P. Depta, Kamran I. Muhammad, James M. McCabe, Andrei Pop, Jaffar M. Khan, Christopher G. Bruce, Giorgio A. Medranda, Jane W. Wei, Jose N. Binongo, and Adam B. Greenbaum
Reference
J Am Coll Cardiol Intv. 2022 May, 15 (9) 965–975
Published
15 May 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
In current transcatheter aortic valve replacement (TAVR) practice, the transfemoral (TF) route is established as the gold standard arterial access site.
However, even though over 90 % of TAVR procedures can be performed TF, in some cases (such as tortuous anatomy, severe calcification, or small vessel size), an alternative access is required1. Several approaches have been used, with the trans-subclavian/trans-axillary (TAX) one being the most commonly performed.
Greenbaum et al., in 2014, presented an out-of-the-box thinking approach, namely transcaval (TC) TAVR, staying femoral, but puncturing the vein and then crossing from the inferior vena cava to the parallel running abdominal aorta, utilizing electrosurgical techniques to enable access towards the diseased aortic valve2. Relatively higher retroperitoneal pressure, as compared to venous pressure, prevents larger hemorrhage, and following the procedure, the puncture is closed with a nitinol occluder device.
As there has been no systematic comparison of TC and TAX access so far, the present study aimed to compare these two approaches with each other, as well as with TF access.
How was it executed? - the methodology
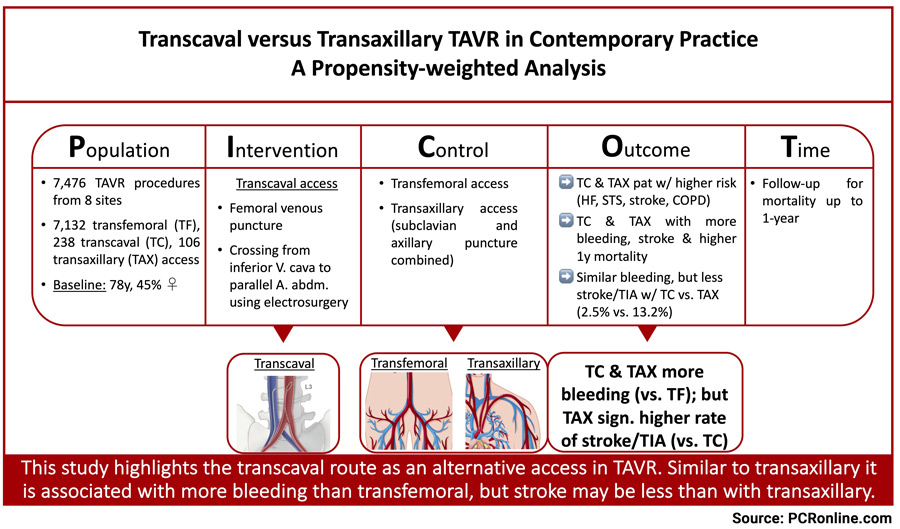
A total of 7,476 procedures from eight sites, performed between January 2017 and December 2020, were collected for analysis and were stratified according to TF, TC, and TAX (subclavian and axillary combined) accesses. Choice of access route was left at local heart team and operator discretion.
Incorporating pre-procedural characteristics, using generalized boosted modeling, a propensity score was estimated, and, based on this score, the sample was weighed to have an equal distribution of pre-procedural characteristics across the different access groups.
Absolute standardized mean difference was used to assess how well imbalances between groups were corrected.
- Primary outcomes of interest were bleeding complications and stroke, defined by VARC-3
- A post-hoc composite outcome (survival to discharge, discharge directly to home instead of another institution, and without stroke/transient ischemic attack (TIA)) was created
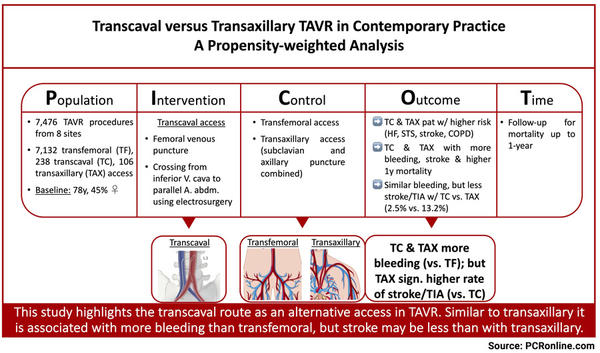
Study analysis according to the Picot scheme. Source: courtesy of Jonathan Curio and Salvatore Brugaletta
What is the main result?
Of the evaluated cases, 7,132 were TF, 238 (3.2 %) were TC, and 106 (1.4 %) were TAX.
44.5 % of the patients were women, mean age was 77.6 ± 9.9 years, and STS-PROM score was 3.9 (2.4, 6.5).
- Patients undergoing TC or TAX tended to have a worse risk profile than patients undergoing TF (higher STS-PROM score, more NYHA functional class III or IV, higher prevalence of previous stroke/TIA, more moderate to severe chronic lung disease)
- Technical success was high and similar among groups (99 %, as per VARC-3), but fluoroscopy time (TF: 15.0 min, TC: 33.6 min, TAX: 24.9 min; each median) as well as contrast volume (TF: 88 ml, TC: 131 ml, TAX: 101 ml; each mean) were higher among the non-femoral access routes, elevated in TC compared to TAX (p < 0.01, respectively); general sedation was used more often in non-femoral access (TF: 18 %, TC: 55 %, TAX: 84 %; p < 0.01 for comparison of latter two)
- Non-femoral routes showed worse outcomes regarding bleeding (VARC-3 types 1-4: TF: 4.6 %, TC: 13.0 %, TAX: 17.9 %), stroke or TIA (TF: 1.7 %, TC: 2.5 %, TAX: 13.2 %), and 1-year mortality (TF: 5.8 %, TC: 8.8 %, TAX: 9.4 %) as compared to TF access.
- Within non-femoral accesses, while bleeding complications were comparable (VARC-3 ≥ type 2: TC: 10.0 % vs. TAX: 13.2 %), stroke or TIA were significantly more common after TAX (13.2 % vs. 2.5 % in TC; unweighted: p = 0.0004, weighted: p = 0.014), and significantly more patients were discharged directly to home after TC (92.6 % vs. 69.6 % in TAX, p < 0.0001), resulting in a significantly lower patient-oriented composite endpoint of discharge to home without stroke/TIA in TAX (62.3 % in TAX vs. 87.8 % in TC, p < 0.0001; 90.3 % in TF)
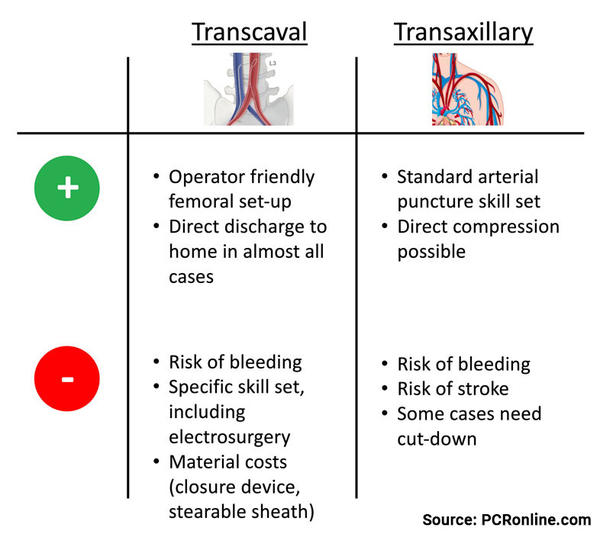
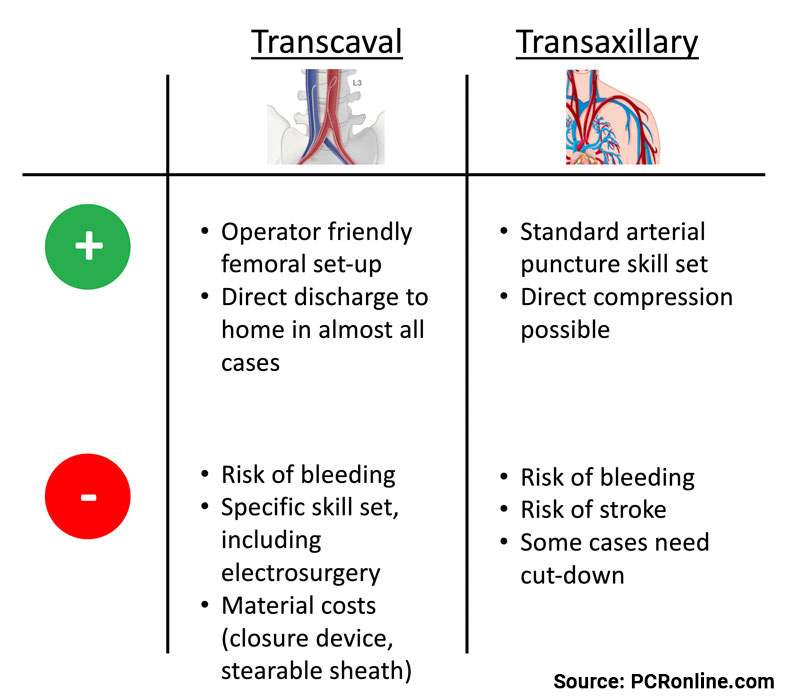
Potential merits and eventual downsides of both transcaval and transaxillary alternative TAVR access routes.
Source: courtesy of Jonathan Curio and Salvatore Brugaletta
Critical reading and the relevance for clinical practice
With the expansion of TAVR to a larger and younger patient population, it becomes a critical obligation to operators to be able to provide a safe and effective procedure, including sufficient arterial access, also in those who cannot undergo standardized and streamlined TF TAVR.
TC access may represent an at-first-sight rather counter-intuitive approach, however, it might bear its very own advantages, such as operator convenient femoral set-up, potentially lower stroke rates, and independence from a surgical cut-down which may be needed to safely puncture any inconveniently located large arterial vessels.
The data herein presented by Lederman et al. are very promising, showing that TC access does not compromise in terms of bleeding, when compared with TAX access, and might even be superior in terms of cerebrovascular events.
However, the data have to be interpreted with caution, as there might be several biases: as allocation to groups was not randomized, it is likely that only ideal patients have been enrolled to undergo the respective procedures. Selection likely was mainly based on anatomical factors, which the clinical characteristics propensity weighing, even though some of its details remain vague, cannot correct for.
Of note, 3 sites reported only TC cases as they use it as their preferred, well-established, non-femoral access, implying a lot of built expertise, which likely impairs the external validity of the study.
Also, as the physicians reporting the data have been pioneers in the field, publishing their experience with already 100 cases in the year the present study only started, a potential learning curve might be excluded from the current data3.
Discussing subclavian arterial puncture, it is true that it uses an existing skillset, while TC access requires unique techniques.
However, even in centers with highly experienced interventional cardiologists, as present in the study, the rate of complications is substantial and, especially, the reported stroke rate at least should be taken as a warning signal. It is questionable whether the mechanism of stroke, likely being the actual instrumentation in the neck vessels, can be addressed by cardioembolic protection devices.
However, most of these protection devices cover all three branches of the aortic arch and would not work in this setting as they would block also the TAVR access route.
Moreover, data on area of stroke are lacking, remaining unclear whether any debris would go in the way of such device or if the access vessel itself is the main carrier of stroke.
In conclusion, the present study is an important perspective on TC as one of the alternative access routes, that are needed to bring the benefit of a safe and effective TAVR procedure to patients with infeasible TF access.
While it is associated with an increased rate of bleeding, similar to TAX access, it might be associated with a lower incidence of stroke compared to TAX.
Eventually, the generally high rate of complications in both non-femoral routes also calls for continued improvement of TF access, such as intravascular lithotripsy tackling cases of severe calcification, to enable as many patients as possible to benefit from this most ideal access site.
There are many roads leading to Rome, which all are important to map and know, to be able to choose the ideal route for each individual patient.
References:
- Carroll, J. D.; Mack, M. J.; Vemulapalli, S.; Herrmann, H. C.; Gleason, T. G.; Hanzel, G.; Deeb, G. M.; Thourani, V. H.; Cohen, D. J.; Desai, N.; et al. STS-ACC TVT Registry of Transcatheter Aortic Valve Replacement. J Am Coll Cardiol 2020, 76 (21), 2492-2516. DOI: 10.1016/j.jacc.2020.09.595.
- Greenbaum, A. B.; O'Neill, W. W.; Paone, G.; Guerrero, M. E.; Wyman, J. F.; Cooper, R. L.; Lederman, R. J. Caval-aortic access to allow transcatheter aortic valve replacement in otherwise ineligible patients: initial human experience. J Am Coll Cardiol 2014, 63 (25 Pt A), 2795-2804. DOI: 10.1016/j.jacc.2014.04.015.
- Greenbaum, A. B.; Babaliaros, V. C.; Chen, M. Y.; Stine, A. M.; Rogers, T.; O'Neill, W. W.; Paone, G.; Thourani, V. H.; Muhammad, K. I.; Leonardi, R. A.; et al. Transcaval Access and Closure for Transcatheter Aortic Valve Replacement: A Prospective Investigation. J Am Coll Cardiol 2017, 69 (5), 511-521. DOI: 10.1016/j.jacc.2016.10.024.







No comments yet!