17 Apr 2023
Prognostic value of tricuspid valve gradient after transcatheter edge-to-edge repair : insights from the TriValve registry
Selected in JACC: Cardiovascular Interventions by E. Zancanaro
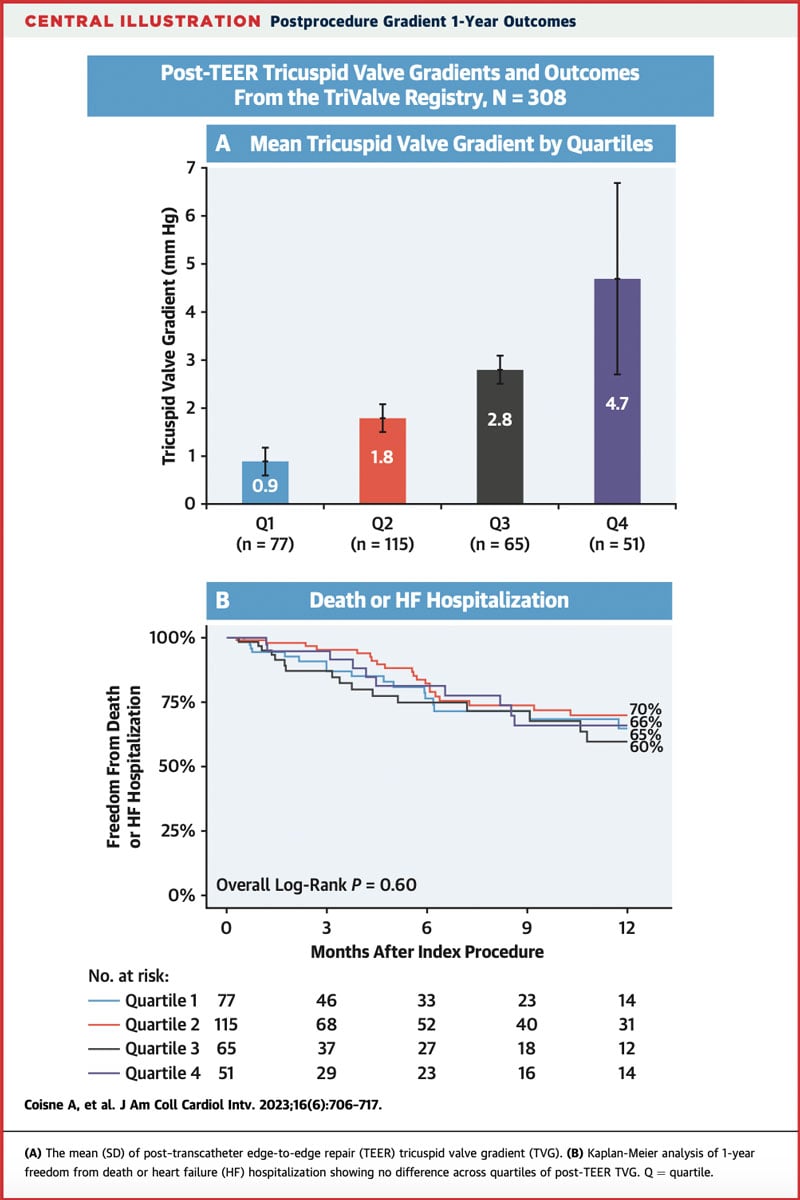
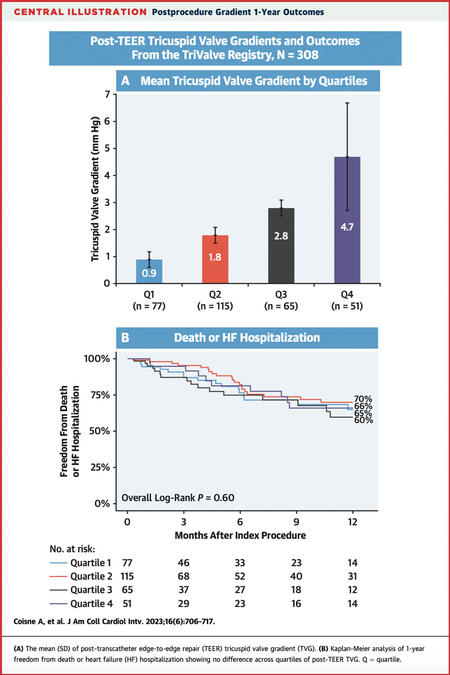
The present study aimed to address the association between the mean TVG at discharge and outcomes among patients who underwent tricuspid TEER within the TriValve Registry.
References
Authors
Augustin Coisne, Andrea Scotti, Maurizio Taramasso, Juan F. Granada, Sebastian Ludwig, Josep Rodés-Cabau, Philipp Lurz, Jörg Hausleiter, Neil Fam, Susheel K. Kodali, Alberto Pozzoli, Hannes Alessandrini, Luigi Biasco, Eric Brochet, Paolo Denti, Rodrigo Estevez-Loureiro, Christian Frerker, Edwin C. Ho, Vanessa Monivas, Georg Nickenig, Fabien Praz, Rishi Puri, Horst Sievert, Gilbert H.L. Tang, Martin Andreas, Ralph Stephan Von Bardeleben, Karl-Philipp Rommel, Guillem Muntané-Carol, Mara Gavazzoni, Daniel Braun, Edith Lubos, Daniel Kalbacher, Kim A. Connelly, Jean-Michel Juliard, Claudia Harr, Giovanni Pedrazzini, François Philippon, Joachim Schofer, Holger Thiele, Matthias Unterhuber, Dominique Himbert, Marina Ureña Alcázar, Mirjam G. Wild, Ulrich Jorde, Stephan Windecker, Francesco Maisano, Martin B. Leon, Rebecca T. Hahn, Azeem Latib
Reference
JACC: Cardiovascular Interventions, Volume 16, Issue 6, 27 March 2023, Pages 706-717 - https://doi.org/10.1016/j.jcin.2023.01.375
Published
27 March 2023
Link
Read the abstract
Reviewer
My Comment
Why this study – the rationale/objective?
Transcatheter Edge-To-Edge Repair (TEER) has emerged as an optimal therapy option in case of Mitral Regurgitation (MR). TEER has been also established as a valid solution for Tricuspid Regurgitation (TR) treatment in surgical unfeasible patients. TEER is associated with valve area reduction and increasing transvalvular gradients, and its hemodynamic effect is particularly relevant in cases of small valve areas, or the need for multiple clips to minimize the TR. It is important to understand the clinical and outcome impact of residual increased TV (Tricuspid Valve) gradient (TVG) after TEER.
The present study aimed to address the association between the mean TVG at discharge and outcomes among patients who underwent tricuspid TEER within the TriValve Registry.
Of notice, TriValve Registry is a registry that included patients with symptomatic TR who underwent TTVI across 24 centers in Europe and North America; also all patients had symptomatic heart failure (HF) and significant TR > = 2+.
How was it executed? - the methodology
In the present study, the TEER patients have been divided into 4 quartiles of mean TVG distribution:
- Q1: 0.0-1.1 mm Hg;
- Q2: 1.2-2.0 mmHg;
- Q3: 2.1-3.0mmHg;
- Q4: 3.1-16.2 mmHg.
The baseline characteristic showed that patients in Q4 had more previous left-side valve interventions while, on the other side, Q4 had higher frequency of TR > = 3+ and lower procedural success, concerning post-echocardiographic control.
Study Endpoints
- Primary: mortality from any cause or HF hospitalization.
- Secondary: overall mortality, HF hospitalization, and functional class.
What is the main result?
A total of 308 patients who underwent tricuspid TEER from August 2015 to March 2022 were included in the present study. The overall mean TVG at discharge echocardiography was 2.3-1.5 mm Hg. The median (Q1-Q3) duration of follow-up was 174 days. The main results are:
- At 1 year, the composite endpoint of all-cause mortality and HF hospitalization occurred in 63 (20.4 %) patients, all-cause mortality in 34 (11.0 %) patients, and HF hospitalization in 48 (15.6 %) patients.
- No differences among TVG quartiles for the freedom from the composite endpoint of all-cause mortality or HF hospitalization at 1 year.
- After multivariable adjustment, TVG in Q4 compared with Q1 to Q3 was not independently associated with 1-year rates of the primary combined endpoint (HR: 0.97; 95 % CI).
- No difference between patients in Q4 and patients in Q1 to Q3 regarding New York Heart Association functional class III to IV before TEER, at 30 days, and at the last follow-up.
- The ROC curve did not show any predictive capacity of the post-TEER TVG for all-cause mortality or HF hospitalization.
Clinical outcomes
The results of this study demonstrated:
- Higher TVGs were associated with higher residual TR and lower procedural success.
- Patients with a higher TVG after tricuspid TEER had similar rates of all-cause mortality, HF hospitalization, and comparable functional capacity after the 1-year follow-up compared with those with a lower TVG.
- Baseline TVG and the number of implanted clips are independently associated with the post-TEER TVG.
Source: Journal of the American College of Cardiology
Critical reading and the relevance for clinical practice
Two considerations have to be made:
- The principal message that has to be highlighted, seeing these results, is the lesser importance of gradient in the case of the TV after TEER compared to what we know from the mitral valve; in fact, in the case of MV, several studies have demonstrated worse prognostic results in case of high post-TEER gradient1,2.
So, TEER in MV cannot be compared to TV, which has to be considered a different entity, taking into consideration that TV anatomy is more compliant in case of more clips implanted compared to MV. - In the case of TV and TEER, it has been established that an “acceptable” gradient after clipping was arbitrarily defined as a TVG < 3 mmHg. The fluctuation in this value does not interfere with distant results and makes the operator freer to maneuver during the TEER procedure.
It differs from residual TR after TEER, which instead impacts negatively the patient prognosis3.
This represents a very important message for daily practice, since the aim is to reduce as much as possible the TR also at expense of increase of gradient.
In conclusion, TVG post-TEER does not show a significant impact on the patient’s prognosis, and residual TR seems to be the real entity to address carefully during TEER procedure.
It’s still important to remember that further investigations and longer follow-up are needed to better guide the intraprocedural decision-making process.
References
- Hahn RT, Hausleiter J. Transmitral gradients following transcatheter edge-to-edge repair. J Am Coll Cardiol Intv. 2022;15(9):946–949.
- Neuss M, Schau T, Isotani A, Pilz M, Schöpp M, Butter C. Elevated mitral valve pressure gradient after MitraClip implantation deteriorates long- term outcome in patients with severe mitral regurgitation and severe heart failure. J Am Coll Cardiol Intv. 2017;10(9):931–939.
- Nickenig G, Kowalski M, Hausleiter J, et al. Transcatheter treatment of severe tricuspid regurgitation with the edge-to-edge MitraClip technique. Circulation. 2017;135(19):1802–1814.