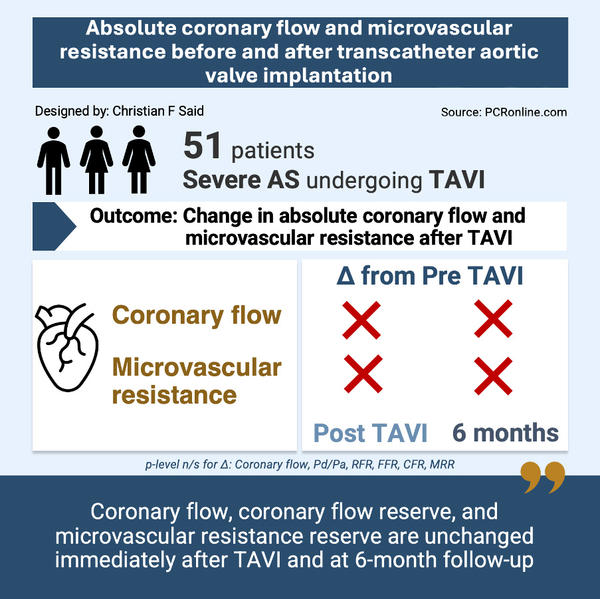
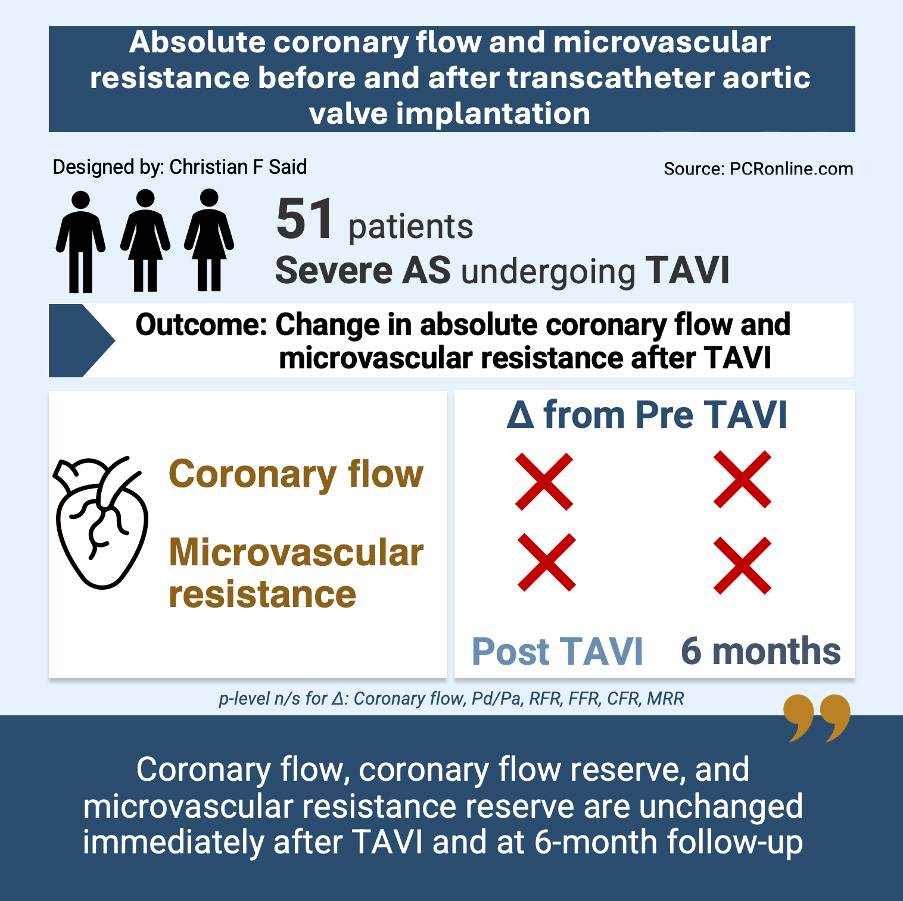
Absolute coronary flow and microvascular resistance before and after transcatheter aortic valve implantation
Selected in EuroIntervention Journal by C. Said , N. Ryan
This study aims to evaluate changes in microcirculatory function post-TAVI, specifically assessing resting and hyperaemic absolute coronary flow and microvascular resistance before TAVI, immediately post, and at 6-month follow-up.
References
Authors
Emanuele Gallinoro, Pasquale Paolisso, Dario Tino Bertolone, Giuseppe Esposito, Marta Belmonte, Attilio Leone, Michele Mattia Viscusi, Monika Shumkova, Cristina De Colle, Ivan Degrieck, Filip Casselman, Martin Penicka, Carlos Collet, Jeroen Sonck, Eric Wyffels, Jozef Bartunek, Bernard De Bruyne, Marc Vanderheyden, Emanuele Barbato
Reference
DOI: 10.4244/EIJ-D-24-00075
Published
Oct 7, 2024
Link
Read the abstractReviewers
Our Comment
Absolute coronary flow and microvascular resistance before and after transcatheter aortic valve implantation.
Source: PCRonline.com
Why this study – the rationale/objective?
Severe aortic valve stenosis (AS) leads to increased left ventricular afterload1, wall stress1, and remodelling2, which are thought to alter coronary blood flow and microvascular resistance3. Coronary microvascular dysfunction (CMD) is common in AS4 and is associated with extra valvular cardiac damage5,6.
Previous studies suggest that, while myocardial perfusion is sustained at rest, it diminishes during hyperaemia, as left ventricular hypertrophy progresses7. The authors hypothesised that transcatheter aortic valve implantation (TAVI) may enhance myocardial perfusion and microcirculatory function by reducing resistance to coronary flow8.
Prior studies have been limited by the lack of precise measurements of volumetric flow and absolute microvascular resistance9,10. This study aims to evaluate changes in microcirculatory function post-TAVI, specifically assessing resting and hyperaemic absolute coronary flow and microvascular resistance before TAVI, immediately post-, and at 6-month follow-up.
How was it executed – the methodology?
In this observational, single centre study, 51 patients with severe AS, no angiographically significant LAD disease, and preserved ejection fraction, undergoing TAVI, were included. Pre-TAVI planning included cardiac computed tomography (CCT), transthoracic echocardiography (TTE), and left and right heart catheterisation.
Continuous intracoronary thermodilution was used to record resting and hyperaemic measurements of absolute coronary flow (Q) and microvascular resistance (Rµ) in the left anterior descending coronary artery, immediately before and after TAVI in all and at six-month follow-up in 20 patients. The Coronary Flow Reserve (CFR) and Microvascular Resistance Reserve (MRR) were calculated.
Myocardial mass and percentage of LAD mass were calculated from the TAVI planning CCT, using Voronoi’s algorithm. Myocardial perfection at rest (QN,rest) and during hyperaemia (QN,hyper) were calculated by dividing absolute flow by the specific myocardial mass subtended by the LAD.
Patients were followed up both clinically and with echocardiogram at 6 months.
What is the main result?
51 patients were recruited, the majority female, with a mean age of 83.7 ± 5.0 years. All patients completed 6-month clinical and echocardiographic follow-up, with 20 patients (39 %) undergoing repeat coronary assessment at that time.
- Absolute coronary flow at rest [Qrest ml/min 68 (56-88) vs 69 (55-92), p = 0.776] and during hyperaemia [Qhyper ml/min 159 (129-201) vs 172 (132-216), p = 0.449] were unchanged pre and post TAVI.
- Microvascular resistance was unchanged pre- and post-TAVI at rest [Rµ,rest WU 1,145 (796-1,277) vs 1147 (822-1299) p = 0.944] and during hyperaemia [Rµ,hyper WU 438 (370-532) vs 422 (332-520) p = 0.458].
- In patients with six-month follow-up physiological assessment, there was no significant difference in absolute coronary flow or microvascular resistance between baseline and follow-up.
- There was a numerically but not statistically significant increase in resting perfusion at six-month follow-up [QN,res: 0.34 (0.30-0.48) vs 0.47 (0.36-0.64) mL/ min/g, p = 0.061].
- Hyperaemic perfusion increased at follow up [QN,hyper: 0.86 (0.69-1.06) vs 1.20 (0.99-1.32) mL/min/g; p = 0.008].
Critical reading and the relevance for clinical practice
This comprehensive assessment of coronary flow demonstrates no difference in absolute resting and hyperaemic flow in patients with severe AS, pre-, immediately post-, and at six-month follow-up post-TAVI. In contrast TAVI lead to significant LV reverse remodelling with a reduction in LV mass and septal thickness. Reduction in the LV mass lead to improved hyperaemic but not resting perfusion at six months follow up.
A significant limitation of the paper is the quantification of absolute myocardial mass from CT. The Voronoi algorithm used in the paper has been compared to relative mass, percentage of the left ventricle, rather than absolute mass measured in grams which is used in this paper. The resting myocardial perfusion valve observed in the study (0.34ml/min/g) is lower than those reported in prior studies using alternate techniques, predominantly CMR and PET, suggesting the measurements of LV mass may require refinement. Overall the study sample size was small with only 20 patients undergoing physiological assessment at six months which may influence the overall analysis.
The lack of change in resting and hyperaemic flow suggests that the damage to the microcirculation due to severe AS is not reversible. Future research should involve larger, multicentred randomised trials to explore microcirculatory dysfunction as a potential marker for early adverse cardiac remodelling in AS and investigate the prognostic significance of coronary microvascular dysfunction in AS.
References
- Huber D, Grimm J, Koch R, Krayenbuehl HP. Determinants of ejection performance in aortic stenosis. Circulation. 1981;64(1):126-34.
- Hein S, Arnon E, Kostin S, Schönburg M, Elsässer A, Polyakova V, et al. Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: structural deterioration and compensatory mechanisms. Circulation. 2003;107(7):984-91.
- McConkey HZR, Marber M, Chiribiri A, Pibarot P, Redwood SR, Prendergast BD. Coronary Microcirculation in Aortic Stenosis. Circulation: Cardiovascular Interventions. 2019;12(8):e007547.
- Rajappan K, Rimoldi OE, Dutka DP, Ariff B, Pennell DJ, Sheridan DJ, et al. Mechanisms of Coronary Microcirculatory Dysfunction in Patients With Aortic Stenosis and Angiographically Normal Coronary Arteries. Circulation. 2002;105(4):470-6.
- Galiuto L, Lotrionte M, Crea F, Anselmi A, Biondi-Zoccai GG, De Giorgio F, et al. Impaired coronary and myocardial flow in severe aortic stenosis is associated with increased apoptosis: a transthoracic Doppler and myocardial contrast echocardiography study. Heart. 2006;92(2):208-12.
- Nemes A, Balázs E, Csanády M, Forster T. Long-term prognostic role of coronary flow velocity reserve in patients with aortic valve stenosis - insights from the SZEGED Study. Clin Physiol Funct Imaging. 2009;29(6):447-52.
- Paolisso P, Gallinoro E, Vanderheyden M, Esposito G, Bertolone DT, Belmonte M, et al. Absolute coronary flow and microvascular resistance reserve in patients with severe aortic stenosis. Heart. 2022;109(1):47-54.
- Gallinoro E, Paolisso P, Bertolone DT, Esposito G, Belmonte M, Leone A, et al. Absolute coronary flow and microvascular resistance before and after transcatheter aortic valve implantation. EuroIntervention. 2024;20(19):e1248-e528.
- Melikian N, Kearney MT, Thomas MR, De Bruyne B, Shah AM, MacCarthy PA. A simple thermodilution technique to assess coronary endothelium-dependent microvascular function in humans: validation and comparison with coronary flow reserve. Eur Heart J. 2007;28(18):2188-94.
- Gutiérrez-Barrios A, Gamaza-Chulián S, Agarrado-Luna A, Ruiz-Fernández D, Calle-Pérez G, Marante-Fuertes E, et al. Invasive assessment of coronary flow reserve impairment in severe aortic stenosis and ecochadiographic correlations. Int J Cardiol. 2017;236:370-4.
- Candreva A, Gallinoro E, Fernandez Peregrina E, Sonck J, Keulards DCJ, Van't Veer M, et al. Automation of intracoronary continuous thermodilution for absolute coronary flow and microvascular resistance measurements. Catheter Cardiovasc Interv. 2022;100(2):199-206.
- Candreva A, Gallinoro E, van 't Veer M, Sonck J, Collet C, Di Gioia G, et al. Basics of Coronary Thermodilution. JACC Cardiovasc Interv. 2021;14(6):595-605.
- van 't Veer M, Adjedj J, Wijnbergen I, Tóth GG, Rutten MC, Barbato E, et al. Novel monorail infusion catheter for volumetric coronary blood flow measurement in humans: in vitro validation. EuroIntervention. 2016;12(6):701-7.14.
- Costa G, Pilgrim T, Amat Santos IJ, De Backer O, Kim WK, Barbosa Ribeiro H, et al. Management of Myocardial Revascularization in Patients With Stable Coronary Artery Disease Undergoing Transcatheter Aortic Valve Implantation. Circ Cardiovasc Interv. 2022;15(12):e012417.
- Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(3):e18-e114.






No comments yet!