28 May 2024
Influence of pathophysiological patterns of coronary artery disease on immediate percutaneous coronary intervention outcomes
Selected in Circulation by G. Occhipinti , S. Brugaletta
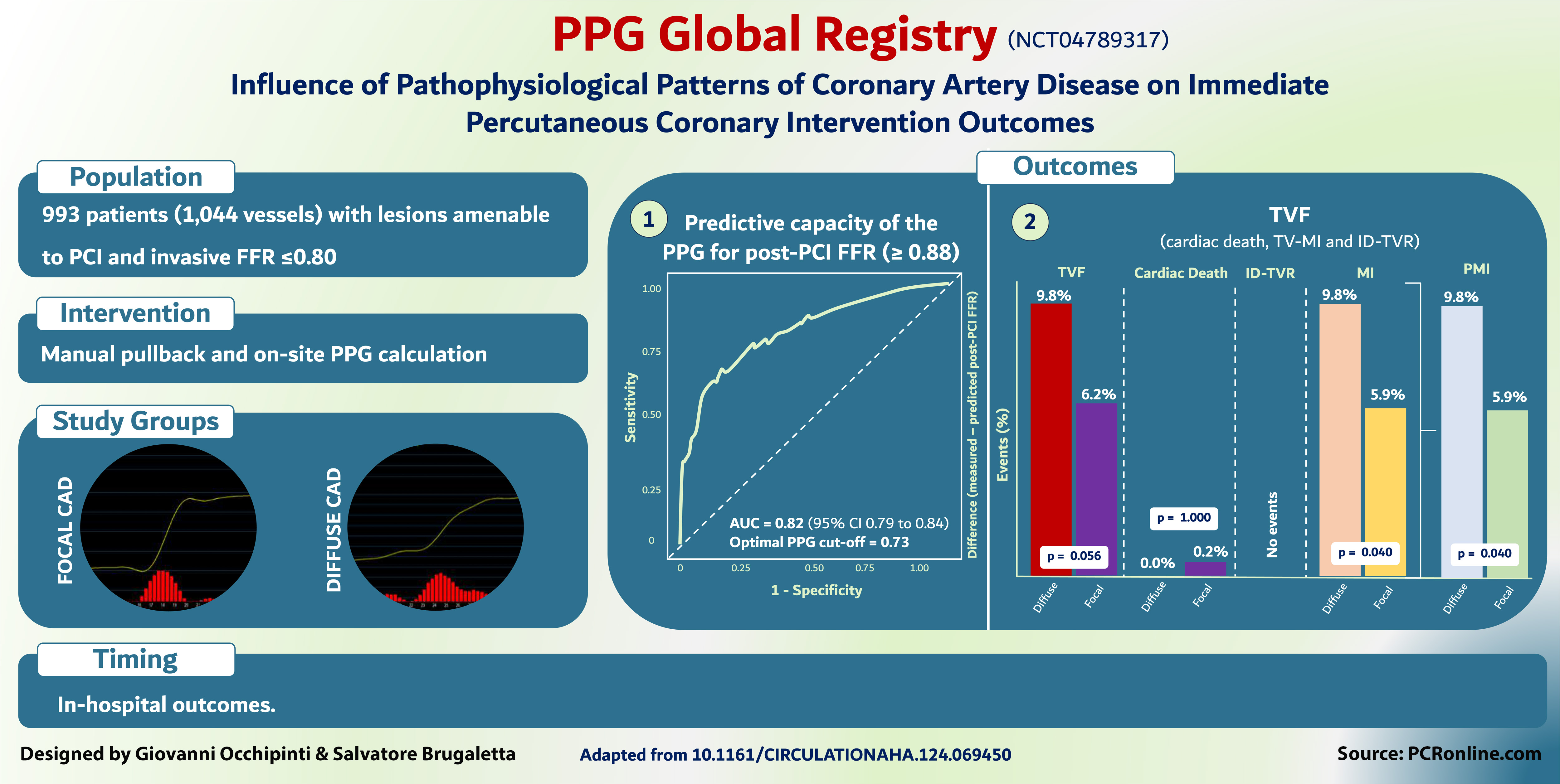
This study demonstrated, for the first time, that PPG - an index to characterize focal vs. diffuse disease - can predict optimal functional revascularization outcomes (post-PCI FFR ≥ 0.88) more accurately than FFR alone.
References
Authors
Carlos Collet, Daniel Munhoz, Takuya Mizukami, Jeroen Sonck, Hitoshi Matsuo, Toshiro Shinke, Hirohiko Ando, Brian Ko, Simone Biscaglia, Fernando Rivero, Thomas Engstrøm, Ketina Arslani, Antonio Maria Leone, Lokien X. van Nunen, William F. Fearon, Evald Høj Christiansen, Stephane Fournier, Liyew Desta, Andy Yong, Julien Adjej, Javier Escaned, Masafumi Nakayama, Ashkan Eftekhari, Frederik M. Zimmermann, Koshiro Sakai, Tatyana Storozhenko, Bruno R. da Costa, Gianluca Campo, Nick E.J. West, Tom De Potter, Ward Heggermont, Dimitri Buytaert, Jozef Bartunek, Colin Berry, Damien Collison, Thomas Johnson, Tetsuya Amano, Divaka Perera, Allen Jeremias, Ziad Ali, Nico H.J. Pijls, Bernard De Bruyne and Nils P. Johnson
Reference
https://doi.org/10.1161/CIRCULATIONAHA.124.069450 | Circulation. 2024;0
Published
Originally published 14 May 2024
Link
Read the abstractReviewers
Our Comment
Why this study – the rationale/objective?
Pullback pressure gradient (PPG) significantly enhances coronary artery disease assessment by mapping the spatial distribution of abnormal epicardial resistance. Unlike fractional flow reserve (FFR), which measures the overall severity of a stenosis and helps determine the need for revascularization, PPG provides detailed insights into whether the disease is focal or diffuse. This distinction may allow clinicians to identify which lesions will benefit most from percutaneous coronary intervention (PCI).
The study aimed to evaluate the PPG’s ability to predict optimal revascularization outcomes, defined as a post-PCI FFR of ≥ 0.88. with the hypothesis that PCI would be more effective in vessels with high PPG values, indicative of focal coronary artery disease.
How was it executed – the methodology?
PPG Global Registry Courtesy of Giovanni Occhipinti & Salvatore Brugaletta. Source: PCRonline.com
The PPG Global Registry (NCT04789317) was a prospective, investigator-initiated, single-arm, multicentre study, that enrolled patients with at least one epicardial lesion with an FFR ≤ 0.80 scheduled for PCI. Manual FFR pullbacks were employed to calculate PPG, resulting in a numerical value ranging from 0.0 (diffuse disease) to 1.0 (focal disease). Based on the PPG value, changes in treatment decision-making were allowed.
The primary outcome of optimal revascularisation was defined as a post-PCI FFR ≥ 0.88. In-hospital target vessel failure (TVF), defined as the composite of cardiac death, target-vessel myocardial infarction, and ischaemia-driven target vessel revascularization, was also evaluated.
What is the main result?
Between December 2020 and September 2023, a total of 993 patients with 1,044 vessels were included.
- The mean FFR was 0.68 ± 0.12, PPG 0.62 ± 0.17, and post-PCI FFR 0.87 ± 0.07.
- PPG was significantly correlated with the change in FFR after PCI (r = 0.65, 95 % CI 0.61-0.69, p < 0.001) and demonstrated excellent predicted capacity for optimal revascularisation (AUC 0.82, 95 % CI 0.79-0.84, p < 0.001).
- Conversely, FFR alone did not predict revascularisation outcomes (AUC 0.54, 95 % CI 0.50-0.57).
- PPG influenced treatment decisions in 14 % of patients, redirecting them from PCI to alternative treatment modalities.
- Peri-procedural myocardial infarction (MI) occurred more frequently in patients with low PPG (< 0.62), compared to those with focal disease.
Critical reading and the relevance for clinical practice
This study demonstrated, for the first time, that PPG - an index to characterize focal vs. diffuse disease - can predict optimal functional revascularization outcomes (post-PCI FFR ≥ 0.88) more accurately than FFR alone.
Moreover, PPG was shown to influence treatment decision in 14 % of the overall cohort of patients, especially those with diffuse disease who were treated by coronary artery bypass graft (CABG) or medical treatment rather than PCI. Diffuse disease by PPG was also associated with higher rate of peri-procedural MI.
Two points should be highlighted to better understand these findings. First, diffuse disease PCI has required use of longer stents in smaller arteries with a high rate of post-dilation: these factors may explain, at least in part, the higher rate of periprocedural MI.
Second, how diffuse vs. focal disease may influence the outcomes or whether CABG/medical treatment is better than PCI for diffuse disease is an open question, which required not only the 3-year follow-up of the present study, but a specific study powered for this hypothesis.
Eventually, these early signals from this pivotal study suggest that PPG is expected to be a revolutionary tool in our cathlab.





1 comment
Excellent study- combining this approach with Intracoronary imaging (?NIRS) to identify high risk plaque might give more information about outcomes.