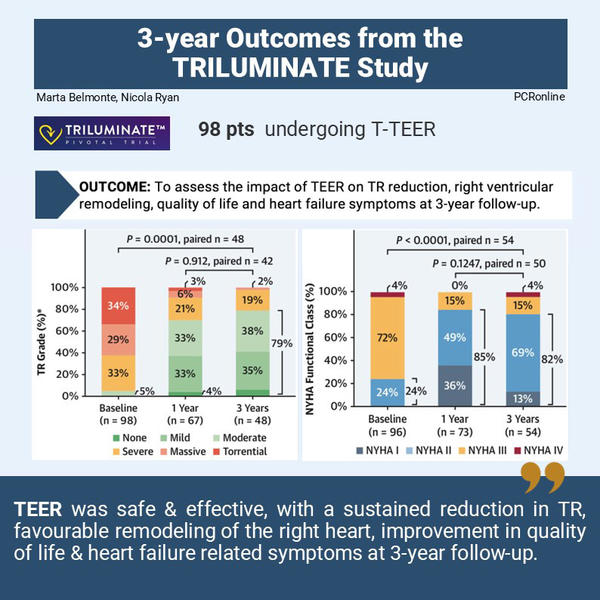
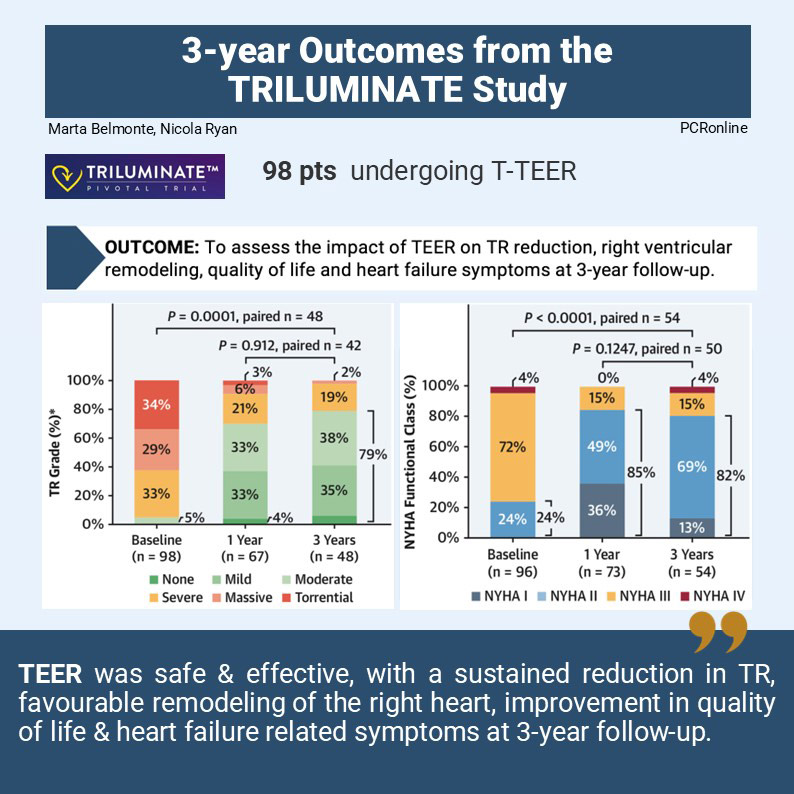
Percutaneous edge-to-edge repair for tricuspid regurgitation: 3-year outcomes from the TRILUMINATE study
Selected in JACC: Cardiovascular Interventions by M. Belmonte , N. Ryan
In this analysis, the 3-year outcomes of the TRILUMINATE study are presented, evaluating the long-term effectiveness of the TriClip T-TEER system on TR reduction, right ventricular remodeling, quality of life, and heart failure symptoms.
References
Authors
Georg Nickenig, Philipp Lurz, Paul Sorajja, Ralph Stephan von Bardeleben, Marta Sitges, Gilbert Tang, Jörg Hausleiter, Jean-Noel Trochu, Michael Näbauer, Megan Heitkemper, Shih-Wa Ying, Marcel Weber, Rebecca T. Hahn, TRILUMINATE Investigators
Reference
DOI: 110.1016/j.jcin.2024.05.036. . Epub 2024 Sep 4.
Published
SEPTEMBER 23, 2024
Link
Read the abstractReviewers
Our Comment
Why this document - the rationale/objective?
The TRILUMINATE study demonstrated that percutaneous tricuspid transcatheter edge-to-edge repair (T-TEER) for severe symptomatic tricuspid regurgitation (TR) is safe and associated with reduced severity of TR and improved clinical outcomes at 6 months, 1 year, and 2 years. In this analysis, the 3-year outcomes of the TRILUMINATE study are presented, evaluating the long-term effectiveness of the TriClip T-TEER system on TR reduction, right ventricular remodeling, quality of life, and heart failure symptoms.
How was it executed – the methodology?
The TRILUMINATE study was a prospective, single-arm, multicenter trial enrolling 98 participants aimed at assessing the safety and performance of T-TEER in symptomatic patients at high surgical risk with moderate or greater TR. Participants had no indications for left-sided or pulmonary valve intervention, severe pulmonary artery systolic pressure (>60 mmHg), previous tricuspid valve procedures, or coaptation gaps greater than 10 mm. Three year follow up visit was completed in 60 of 98 participants; 25 deaths, 10 withdrawals and 3 missed visits.
What is the main result?
At enrollment two thirds of the patients were female with a mean age of 77 years, with three quarters NYHA III/IV. At 3-year follow-up, echo evaluable TR severity was available in 48 patients and NYHA functional class in 54.
- Reduction to moderate or less TR was demonstrated in 79% of patients (38/48) at three years (P<0.0001) with no difference between 1 & 3 years (p=0.912)
- TR reduction of at least one grade was achieved in 92% (44/48) of patients at three years.
- NHYA functional class III/IV reduced from 76% of participants at baseline to 19% at three years (P=<0.001) with no difference between 1 & 3 years.
- Quality of life as assess by the KCCQ decreased from 1-3 years (-12 ±21 points, p=0.0001) however remained improved compared to baseline (mean improvement baseline to three years 10 ± 3 points, p=0.006)
- Echocardiographic parameters of RV remodeling including right ventricular end-diastolic volume (5.2±0.1cm baseline 4.9±0.1cm 3 years, p<0.0001) and tricuspid annular diameter (4.3±0.6cm baseline 4.1±0.6cm 3 years, p=0.0145) improved at three year follow up.
- Site reported HF hospitalisations were reduced by 75% with T-TEER (0.56 events/patient year 1 year pre-device to 0.14 events/patient year 3 years post device, p<0.0001).
Critical reading and the relevance for clinical practice
The three year follow up of TRILUMINATE demonstrates that the initial safety and efficacy benefits of T-TEER remain at medium term follow up. The initial reduction in TR is sustained with improvements in functional class maintained throughout follow up. Patient reported quality of life decreases from one year to three year follow up but remains improved compared to baseline. Importantly the procedure is safe with no requirement for cardiovascular surgery or endocarditis through longer term follow up.
TR is a common condition with many patients unsuitable for surgical intervention due to their co-morbidities, even in patients suitable for surgical intervention surgery carries a high morbidity and mortality perhaps due to the advanced nature of the disease (1,2). T-TEER is an attractive solution to treat TR in patients with valvular anatomy suitable for intervention in order to improve quality of life and outcomes. TRILUMINATE is the first prospective multicentre trial to evaluate outcomes in patients treated with T-TEER for moderate or greater TR
The initial improvements in TR severity previously reported are maintained at three-year follow up with 79% of patients maintaining moderate or less TR and at least one grade reduction in TR seen in 92%. This is encouraging data as the trial enrolled participants using an early generation of the T-TEER device, current generations of the T-TEER device allow independent leaflet grasping as well longer and wider devices. Echocardiographic parameters assessed remained significantly improved at three years, [vena contracta width (1.7 ± 0.6 to 0.6 ± 0.3 cm; P < 0.0001), EROA (0.6 ± 0.3 to 0.3 ± 0.1 cm2; P < 0.0001), regurgitant volume (51.3 ± 18.2 to 22.6 ± 10.8 mL/beat; P < 0.0001), and PISA (0.9 ± 0.2 to 0.6 ± 0.2 cm; P < 0.0001)]. Studies with contemporary T-TEER devices have demonstrated increase efficacy in reducing TR severity and may translate to improved medium- and long-term outcomes (3,4).
The initial improvement in NYHA functional class was maintained at three years, though quality of life as assessed by the KCCQ deteriorated from year 1 to year 3. This is likely multifactorial including progressive cardiac dysfunction, other co-morbidities as well as aging of the population given the absence of deterioration in echocardiographic parameters. Importantly despite the deterioration between year 1 and 3 quality of life remained improved compared to baseline. Hospitalisations for heart failure is an important PROM and T-TEER reduced hospitalisation from 0.56 events/patient year in the year prior to T-TEER to 0.14 events/patient year at three years follow up. All-cause mortality over the three year period was 27% with 18 of 25 deaths cardiovascular. The relatively high mortality likely reflects the age and underlying co-morbidities of the population enrolled in the trial.
Degree of reduction of TR appears to be important in longer term outcomes as those with moderate or less TR at 30 days were less likely to experience heart failure hospitalization or death during three year follow up compared to those with severe or greater TR. Registry data from TriValve (5) demonstrated similar findings with reduced mortality in patients with TR <2+.
There are a number of important limitations to this trial including the lack of a control arm as well as the use of early generation devices. Furthermore there is likely a learning curve in implantation of T-TEER devices and whilst the enrolling centers were high volume heart valve centers this was the first use of the device. Overall, this trial represents the longest follow-up to date for T-TEER demonstrating sustained benefits in patients with symptomatic moderate or greater TR.
References
- Wang TKM, Akyuz K, Xu B et al. Early surgery is associated with improved long-term survival compared to class I indication for isolated severe tricuspid regurgitation. J Thorac Cardiovasc Surg 2023;166:91-100.
- Park SJ, Oh JK, Kim SO et al. Determinants of clinical outcomes of surgery for isolated severe tricuspid regurgitation. Heart 2021;107:403-410.
- Sorajja P, Whisenant B, Hamid N et al. Transcatheter Repair for Patients with Tricuspid Regurgitation. N Engl J Med 2023;388:1833-1842.
- Lurz P, Besler C, Schmitz T et al. Short-Term Outcomes of Tricuspid Edge-to-Edge Repair in Clinical Practice. J Am Coll Cardiol 2023;82:281-291.
- Taramasso M, Alessandrini H, Latib A et al. Outcomes After Current Transcatheter Tricuspid Valve Intervention: Mid-Term Results From the International TriValve Registry. JACC Cardiovasc Interv 2019;12:155-165.






No comments yet!