How should I treat? - How to reduce cardiac conduction disturbance with Sapien 3 valve?
Conduction disturbances remain the most common complications of TAVI and its main drawback compared to surgery. How would you treat this 82-year-old man, height 1.68 m, weight 112 kg, with peripheral artery disease, who presented with severe aortic stenosis and symptoms of NYHA Class 3 breathlessness?
Author
Learning objectives
- to understand the concept of Radiolucent line of Sapien 3 valve
- to learn how to use cusp overlap view (COL) for depth implantation
- to learn how to perform a High deployment technique with Sapien 3 valve
Case Summary
- An 82-year-old man, height 1.68 m, weight 112 kg, with peripheral artery disease was referred to our hospital with severe aortic stenosis and symptoms of NYHA Class 3 breathlessness.
- Co-morbidity included hypertension, permanent atrial fibrillation.
- Echocardiography confirmed severe aortic stenosis with a peak aortic velocity of 5.2 m/s, mean pressure gradient 55mmHg.
- LV systolic function was 45%
- Coronary angiogram showed no coronary artery disease.

Multi-slice computed tomography demonstrated an annulus area of 503 mm2 (area-derived diameter 25.3mm).
LVOT measured 23.1x28.2mm, average 25.8mm.
The sinus of valsalva was spacious (average 31 mm). Sino tubular jonction was large 31 mm. Right coronary height was 14 mm and left coronary 13 mm. Length of membranous septum was 4 mm. Iliofemoral access vessels were of large calibre.
We decided to perform a Sapien 3 26 mm valve, transfemoral access. STS score 5.2% and the PPI risk was estimated at 8%.
Emerging question
Share your opinion now!
Conflict of Interest Statement
The author has no conflict of interest to declare
Actual treatment & management of the case
Cusp overlap view of the annulus
TAVI was performed under local anaesthesia with minimal sedation administered by an anesthesiologist.
The marker pigtail was delivered via 5Fr right radial access, and pacing was through the LV wire. Vascular access was left femoral 14Fr, with Proglide pre-closure.
Cusp overlap view was LAO 2 CAU 7.
The most inferior point of the annulus is the NCC where the pigtail is.
The objective of this view is multiple:
- to reduce the parallax of the device
- to show the lowest point of the annulus
Analysis of the Sapien3 valve in COL view
- Because of anatomic consideration, TAVI devices have an anteroposterior angulation in the annulus.
- Here, we can see no parallax of the device in COL view.
- A pigtail flush catheter is positioned at the base of the NCC and left in place after the deployment aortogram to confirm valve stent coverage of the most inferior point of the aortic annulus.
- The valve is positioned by aligning the radiolucent line that is located at the superior aspect of the lowest set of stent struts of the crimped valve at the base of the noncoronary cusp (NCC).
- Indeed, we can see a gap between the valve and the balloon; the valve is above the balloon.
The pigtail is left in the NCC during the inflation to show that the valve deployed finished at the radiolucent marker.

Final result
The valve is implanted in the highest position:
- The lowest point of the annulus is covered by the lowest point of the valve.
- All other points of the annulus are above that point.
- In subsequent, we can minimize at maximum membranous septum injury.
- A good final result was achieved, with a high implant, trivial aortic regurgitation.
- Out of room, no modification of the EKG was noted.
- Echocardiography post-procedure confirmed trivial AR, mean gradient 8 mmHg.
- Next day discharge was possible without modification of the EKG.
Discussion
Coplanar 3 cusps view (video 1):
We can see that the valve is located in the NCC-RCC commissure. Too much parallax is noted in this view. We cannot anticipate where the device will end after deployment in coplanar 3 cusps view.
Cusp overlap view (video 1):
In this case, there was no parallax of the device. It is easiest to control depth implantation.
After inflation, in coplanar 3 cusps view, the persistent parallax doesn’t allow us to understand the depth implantation (video 2).
When using cusp overlap view, we can see no parallax (video 2).
Here is the highest position that we can implant the device to reduce septum membranous injury and conduction disturbance.
Here is a modelisation of our implantation (video 3).
It begins with a coplanar three cusps view; parallax of the valve can be noted; the shortest part of the device is posterior.
We can see that the most inferior point of the annulus (violet point) is at the most inferior point of the Sapien 3 valve and no point of the valve is above the annulus plane.
That explains no PVL and also the minimum stress with MS (located between NCC and RCC).
- Sammour and Al published a systematic approach of high deployment of sapien 3 valve and a lower rate of conduction abnormalities (left bundle block branch and pacemaker implantation). Thirty-day permanent pacemaker rates were lower with HDT (5.5% versus 13.1%; P<0.001), as were rates of complete heart block (3.5% versus 11.2%; P<0.001) and new-onset left bundle branch block (5.3% versus 12.2%; P<0.001).
- In this case, the perpendicular plane was obtained between the device and the annulus in COL view.
- Frequently, a parallax device persists in COL view (figure 1a); it means that the valve orientation from aorta to ventricle has an important anteroposterior orientation.
- To correct this parallax, it’s necessary to add more caudal view (figure 1b); it impacts annular plane; the RCC is above the valve plane.
- The depth implantation (radiolucent line) is not significantly impacted.
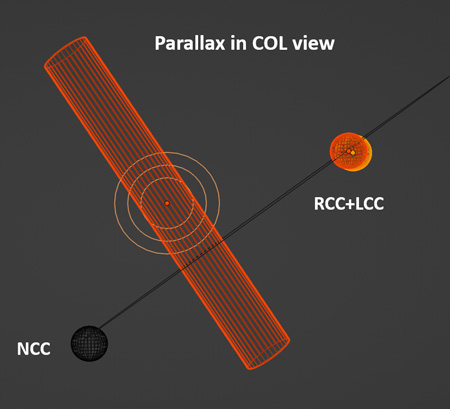
Figure 1a
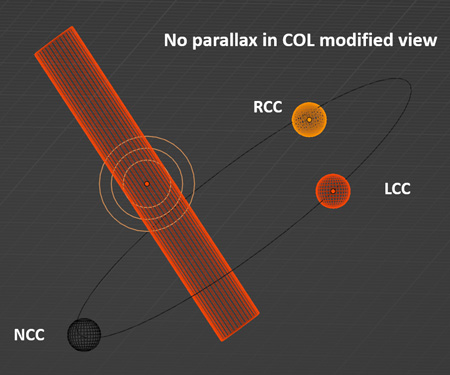
Figure 1b
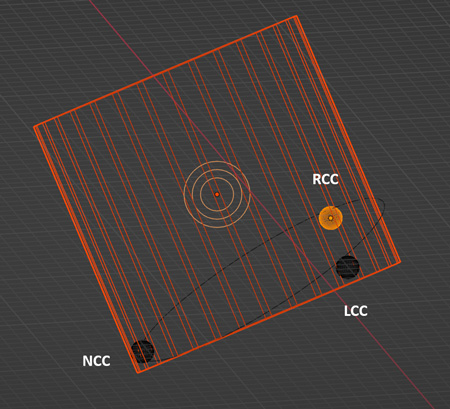
Figure 2. Sapien 3 expanded valve in COL modified view with an important anteroposterior misalignment in the annulus.
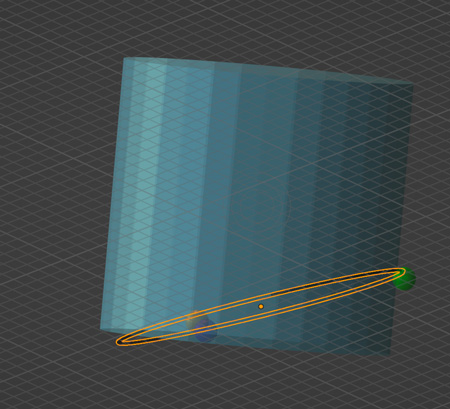
Figure 3
Due to an important anteroposterior misalignment, the Sapien 3 can be expanded above the annulus plane which may induce PVL in the posterosuperior part of the annulus (figure 3).
It is necessary to implant the device lower or to apply some manipulations to reduce the anteroposterior de-axing.
Conclusion
- The cusp-overlap view allows to understand implant depth.
- It reduces the parallax of TAVI devices.
- This imaging technic is not only used for auto expandable devices.
- The radiolucent line is a valve marker independent of the balloon marker; it’s the end of the foreshortening of Sapien 3 valve.
- High deployment reduces membranous septum stress and conduction cardiac disturbance.
- Length of stay is directly impacted. High implantation facilitates early discharge.
The invited Expert's opinion
Conduction disturbances remain the most common complications of transcatheter aortic valve implantation (TAVI) and its main drawback compared to surgery. Indeed, recent data suggest a poorer outcome in patients having new onset left bundle branch block and needing pacemaker implantation after TAVI. Thus, the individual risk of a pacemaker remains central to discussion with the patient and the heart team when the patient is eligible for surgery.
Thanks to efforts made in the last years to understand mechanisms and predictors of this complication, the technique of valve implantation has been refined and the risk of pacemaker implantation has finally decreased. Among these technical enhancements, high implantation of the transcatheter heart valve (THV) is the strongest protector of conduction disturbances.
The standard coplanar view used for the implantation of the device does not assure proper implantation in a very high position beneath the aortic annulus, in particular when using self-expanding devices. This is due to the frequent presence of parallax of the delivery catheter, which requires further adjustments and final implantation in a non-coplanar view, and a more difficult appreciation of the true depth of the THV.
Recently, the cusp-overlap view (a coplanar projection by overlapping the right and left coronary cusps, generally a right anterior oblique caudal view) has been adopted first for self-expanding devices1 and lastly for the SAPIEN 3/Ultra2. This view reduces the parallax of the delivery catheter and elongates the left ventricular outflow tract allowing a more accurate estimation of the depth of the THV.
In this case, Dr Zouaghi perfectly illustrates the advantages of the cusp-overlap view compared to the standard coplanar view in order to achieve a very high THV implantation when using a SAPIEN 3 device. I congratulate Dr Zouaghi for the successful procedure with optimal results and the very comprehensive teaching points proposed in this case.
However, this technique might have potential drawbacks, which have to be mentioned:
- The access to coronary ostia might be compromised in patients with low coronary takeoffs and, importantly, in case of TAV in TAV, which might be crucial in low-risk younger patients.
- There exists a potential risk for valve aortic embolization/malposition (one patient in the case series published by Sammour et al)2.
- The deployment of a THV using a projection right anterior oblique/caudal projection might be challenging in obese patients and impossible in certain cases requiring extreme angulations. While this technique seems to be unavoidable when using self-expanding prostheses, it has fewer advantages when implanting balloon-expandable valves because of:
- Less impact of parallax, and better control of final depth implantation.
- The foreshortening of the SAPIEN 3 THV (which ultimately conditions the depth of implantation), which depends on the expansion of the prosthesis. An asymmetrical foreshortening may be observed when the valve is open from a commissure, which is more difficult to detect using the cusp-overlap view3.
- Reduced risk of pacemaker implantation and conduction abnormalities when using the classical technique, which was similar to surgery in the PARTNER 3 trial.
The continuous advances in technique and technology of TAVI and the consequent reduction of complications have allowed the expansion of this therapy to low-risk younger patients. The recent introduction of the cusp-overlap technique shows the efforts made in this direction and might be associated with a reduction of the risk of pacemaker implantation. Nonetheless, it has potential risks. An accurate balance of potential benefits and risks is mandatory and the technique of THV implantation should be customized according to the risk of pacemaker implantation of an individual patient, the expected impact of this potential pacemaker, and the risk of compromise of coronary access according to the anatomy of the aortic root and the need of a TAVI-in-TAVI procedure in the future.
Conflict of Interest Statement
Marina Urena has no conflict of interest to declare.
References
- Tang GHL, Zaid S, Michev I, Ahmad H, Kaple R, Undemir C, Cohen M, Lansman SL. "Cusp-Overlap" View Simplifies Fluoroscopy-Guided Implantation of Self-Expanding Valve in Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2018;11:1663-1665. doi: 10.1016/j.jcin.2018.03.018
- Sammour Y, Banerjee K, Kumar A, Lak H, Chawla S, Incognito C, Patel J, Kaur M, Abdelfattah O, Svensson LG, Tuzcu EM, Reed GW, Puri R, Yun J, Krishnaswamy A, Kapadia S. Systematic Approach to High Implantation of SAPIEN-3 Valve Achieves a Lower Rate of Conduction Abnormalities Including Pacemaker Implantation. Circ Cardiovasc Interv. 2021;14:e009407. doi: 10.1161/CIRCINTERVENTIONS.120.009407.
- Pop A, Kasel M. Line of Lucency Method – Clarifications on Its Use, Structural Heart, 2021; 5: 338-339, DOI: 10.1080/24748706.2021.1896823





No comments yet!