09 Apr 2021
Giant right coronary artery aneurysm unmasked in the setting of STEMI: killing two birds with one stone
Consult this Twitter case from Ricardo Sanz: an 80-year-old man presenting with inferior STEMI, primary PCI being complicated by the presence of a giant coronary aneurysm in the RCA that hindered the advancement of wires and material towards a small and hidden entry point. Creative off-label tools were the only way to achieve recanalization and finally coronary patency.
This case was originally published on Twitter by @RiSanz2020 via #CardioTwitterCase
Clinical presentation
We present an 80-year-old gentleman, with history of hypertension, dyslipidemia and former smoker, admitted to our center because of inferior STEMI, two hours after symptom onset (Figure 1).
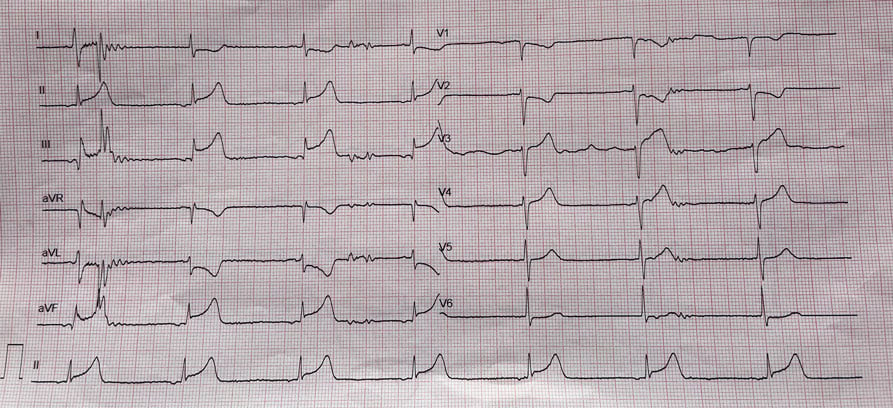
Figure 1
Case management
After dual antiplatelet treatment and heparinization, emergent coronary angiography showed no stenoses in the LCA, and a proximal RCA occlusion after a giant coronary artery aneurysm (CAA, Video 1). With a JR4 guiding catheter, the wire did not reach the point that we presumed to be the entry point to the acute occlusion. Even after changing the JR4 for an AL1 guiding catheter, and also using a Guideliner extension catheter, it still did not work (Video 2).
Guideliner was too soft, and pointed always towards the posterior aspect of the aneurysm.
Then, we decided to use a “more curved”, stiffer and smaller catheter to orient the wire to the presumed thrombotic occlusion point. To do that, we cut the 6Fr AL1 guiding and advanced a 4Fr LIMA diagnostic catheter into the aneurysm and towards its anterior aspect (Video 3). This allowed a more precise orientation, and finally the advancement of a 300 cm long BMW wire, crossing the thrombotic occlusion and reaching the distal RCA (Video 4).
Coronary angiography showed for the first time the whole RCA anatomy, with the aneurysm and the culprit thrombotic complicated plaque just afterwards, with thrombus burden downstream.
Pre-dilation and thrombus aspiration were needed to improve the flow (Video 5), and then two covered stents (Papyrus 3.5/20 and 4.5/20) were implanted, aiming at treating the culprit plaque and also at excluding the aneurysm (Video 6).
Overlap was confirmed with angiography and afterwards with OCT. This intracoronary imaging technique also demonstrated excellent apposition at both ends on “normal” vessel, and a good sealing result in the gap between stents, precluding future blood entry to the aneurysm. Final angiographic result is shown in Video 7.
A distal posterolateral branch still revealed some thrombotic content, but it was left for medical treatment.
Follow-up
The patient developed no complications, was followed in the CCU and discharged on day 3 with optimal medical therapy, including DAPT for one year, and with the suggestion of prolonging it for more than 12 months.
Final remarks
This case shows the efficacy of covered stents for CAA exclusion, being at the same time able to repair the culprit ruptured plaque. In-stent restenosis is a concern with these stents, but with these large diameters, this eventuality was considered not likely. Regarding stent thrombosis, we think that prolonged DAPT is the best option. Finally, when dealing with these complex anatomies, intracoronary imaging is mandatory to achieve the best outcomes.
Original tweet and Twitter discussion
80-yo male, 2-hours of CP. STEMI code with the following EKG. No stenosis in the left coronary artery, and surprise in the right #scarymoviepic.twitter.com/hL5be9zzLR
— Ricardo Sanz (@RiSanz2020) March 26, 2021




2 comments
Wow! Amazing case! Thanks for sharing! Why did you have to cut the AL1? Doesn't the 4F LIMA catheter go through otherwiese? In your video, the LIMA-catheter is totaly straight. Is this just due to projection? Or did you manipulate thisone too? Thanks again!
Excellent idea the catheter in catheter technique to advance the wire into the site of occlusion!