A stuck Rota burr in a "flintstone" coronary artery
#CardioTwitterCase originally published on Twitter
Step by Step video on how to deal with a stuck Rota burr with the same arterial access. Nice example of Kokeshi phenomenon.
This case was originally published on Twitter by @jorgeachv
Clinical presentation
- 67-year-old man, former smoker, HTN, DMII
- ACS without ST elevation, troponin (106-125 pg/ml), creatinine 1.04 mg/dl
- Echocardiogram with mild mid- and apical hypokinesis at the anterior wall. Ejection fraction 60 %.
- View baseline angiogram on Video 1.
Diagnosis
After stabilization, patient was diagnosed with severe and calcified LM and MVD disease, poor distal bed for bypass. Heart team decision was to perform a PCI with atherectomy.
Burr entrapment (BE) consists of its embedment through a severe stenosis, preventing both further advancement or retrieval. Several bail-out techniques have emerged to deal with this complication. One of these techniques is to use a second wire and to inflate a balloon (balloon-trapping technique).
Case description
We present the case of a 67-year-old male with LM and MVD who underwent two complex coronary interventions with long runs of atherectomy.
During mid-distal rotablation with 1.25 mm burr, a stuck coronary burr due to Kokeshi phenomenon was observed. ACT was confirmed above 250 seconds. A guide extension catheter (GEC) was passed over the shaft of the entrapped burr, a second guidewire over a microcatheter was able to pass through the lesion and the stuck burr, and balloon escalations were used to successfully release the burr (Videos 2 and 3).
A balloon-trapping technique was performed successfully, and this maneuver unblocked the entrapped burr.
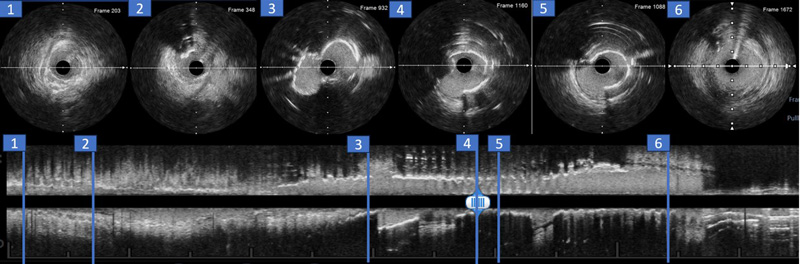
Intravascular imaging with IVUS was performed to rule out iatrogenic complications in the proximal segments of the artery and left main (Figure 1).
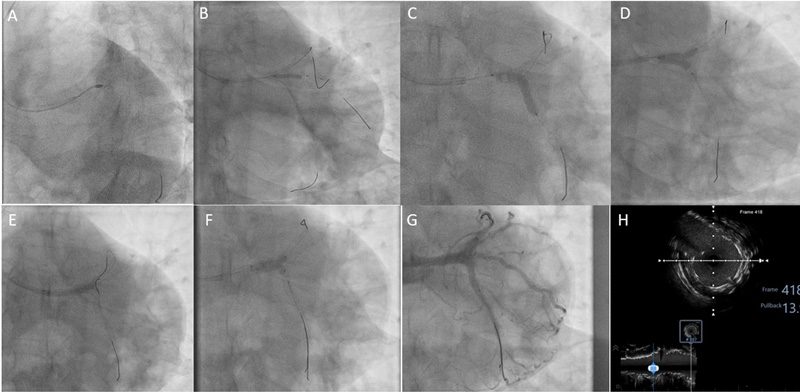
Staged procedure to perform double-kissing culotte in the left main, provisional to intermediate ramus, balloon angioplasty in mid-distal LAD, and diagonal branch, was successfully performed, guided by IVUS (Figure 2 and Video 4).
A 3-month follow-up was scheduled to determine the need for future intervention on the left anterior descending artery.
Videos:
Figures:
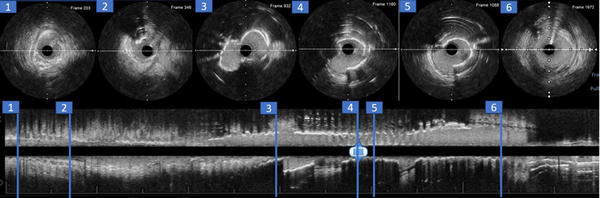
IVUS return from distal LAD to left main after balloon angioplasty at LAD. Cross-sectional views showed several diffuse calcified LAD morphologies and absence of iatrogenic complications after burr extraction and deep vessel intubation.
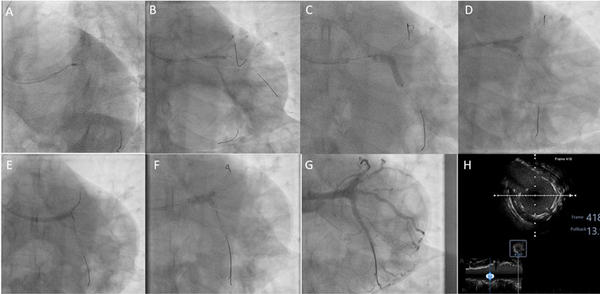
Summary of the left main PCI staged procedure. A. Left circumflex rotational atherectomy. B. Non-compliant 2.5 x 15 mm balloon to intermediate ramus. C. After sequential predilatation with non-compliant balloons, 3.5 mm DES was implanted from LCx to LM. D. First kissing-balloon technique with non-compliant 3.5 mm balloons. E. 3.0 mm DES implanted from LAD to LM. F. Second 3.5 mm kissing-balloon technique with non-compliant balloons. G. Final angiogram from caudal view. H. IVUS imaging at the carina level in the distal left main.
Final remarks
After successful retrieval of an entrapped burr with the help of a second wire and GEC, potential iatrogenic complications can be diagnosed or solved in an efficient and safety way. Intravascular imaging must be performed before the retrieval of distal wires.
Original tweet and Twitter discussion
Halloween nightmare. First time I had to deal with burr entrapment. Long, and heavily ca+2 lesion. > 7 min of atherectomy with 1.5 mm burr wout success, 1.25 did the job partially but got stuck due to pecking motion distal LAD. Fortunate Pt did well, successful IVI DEB PCI pic.twitter.com/2akIKmV5sm
— Jorge A. Chavarria V. . (@jorgeachv) November 2, 2023
Authors







No comments yet!