Does metallic stent ablation by rotational atherectomy influence on the coronary microcirculation?
Supported by the EuroIntervention Journal
Authors
Yuma Hamanaka1, Yohei Sotomi1, Tomoaki Kobayashi1, Yoshiharu Higuchi1
Case summary
An 80-year-old man underwent percutaneous coronary intervention (PCI) with a bare-metal stent for severe stenosis at proximal left anterior descending (LAD) coronary artery 13 years ago. In-stent restenosis was treated by a drug-eluting stent (DES) 1 year later.
The patient recently presented with recurrent chest pain. Emergent coronary angiography revealed subtotal occlusion at left circumflex artery and severe stenosis at distal LAD, both of which were simultaneously treated.
Intravascular ultrasound presented under-expansion of the aforementioned metallic stents at the proximal LAD due to the circumferential calcification (D-c). Optical coherence tomography (OCT) indicated minimum lumen and stent areas of 2.51 mm2 and 2.71 mm2, respectively (D-c).
We performed rotational atherectomy (Boston Scientific Rotablator® system, burr size 1.75 mm; 180,000 rpm) to ablate the under-expanded metallic stent and underlying calcification (B), followed by DES implantation (C). OCT 3-dimensional reconstruction clearly demonstrated the ablated struts at the distal part of the stent (G, H-c).
We examined the influence of metallic stent ablation on the coronary microcirculation by index of microcirculatory resistance (IMR). The IMR increased after rotational atherectomy from 19 to 31 (I, J), resulting in the deteriorated coronary flow reserve (CFR) despite the improved fractional flow reserve (FFR)
Creatine kinase (-MB) peaked at 373 (35) U/L 1 day after the procedure, which did not fulfil the criteria of periprocedural myocardial infarction according to the ARC definition[1]. One month later, the IMR eventually recovered to 13 (K) while CFR also improved.
The present case would be the first report to show the successful recovery of temporary microcirculatory deterioration after metallic stent ablation by rotational atherectomy. Several case reports and case series indicated some controversial insights into the safety of stent ablation[2-4]. The present case demonstrated that the influence of stent ablation on the coronary microcirculation was limited and temporary if imaging-guided appropriate procedure can be performed.
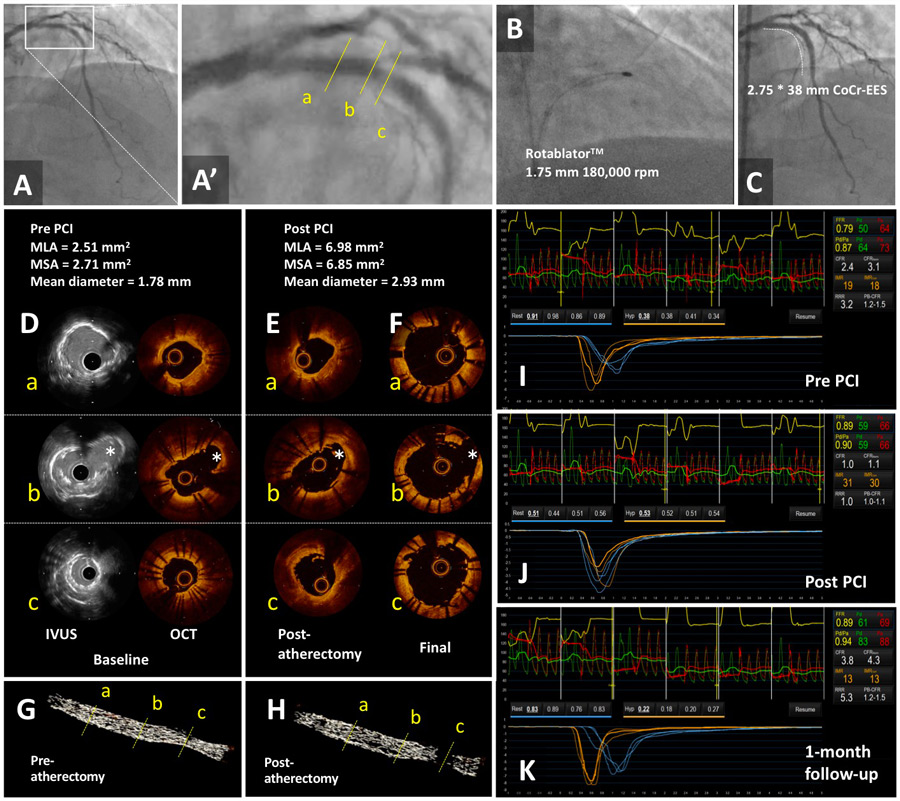
Figure 1. Imaging assessment of stent ablation - Cine angiography at baseline (A, A’ [magnified view]), during rotational atherectomy (B), and post-PCI (C) indicates the successful result of the procedure. Baseline intravascular ultrasound (IVUS) and optical coherence tomography (OCT) are presented in panel D. Post-atherectomy OCT and final OCT are presented in panels E and F, respectively. Three-dimensional reconstruction of the OCT image clearly shows ablated metallic struts at the distal part of the under-expanded stents (G-c and H-c). Impact of rotational atherectomy on coronary microcirculation was assessed by index of microcirculatory resistance (IMR). The IMR increased after rotational atherectomy from 19 to 31 (I, J), resulting in the deteriorated coronary flow reserve (CFR) despite the improved fractional flow reserve (FFR). One-month later, the IMR eventually recovered to 13 (K), suggesting that the influence of stent ablation on the coronary microcirculation was limited and temporary, if imaging-guided appropriate procedure can be performed. * side branch.
Conflict of interest statement
Y. Sotomi and Y. Higuchi received speaker honoraria and grants from Abbott Vascular Japan, Boston Scientific Japan, TERUMO, Cardinal Health, and Medtronic. The authors have no other conflict of interest to declare.
Acknowledgement
The authors wish to thank Takayuki Okamura MD. PhD. for his technical support for the 3D-reconstruction of OCT image.
Affiliations
- Department of Cardiology, Osaka Police Hospital, Osaka, Japan.
References
- Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, McFadden E, Lansky A, Hamon M, Krucoff MW, Serruys PW. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 2007;115(17):2344-51.
- Edes IF, Ruzsa Z, Szabo G, Lux A, Geller L, Molnar L, Nowotta F, Hajas A, Szilveszter B, Becker D, Merkely B. Rotational atherectomy of undilatable coronary stents: stentablation, a clinical perspective and recommendation. EuroIntervention: journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology 2016;12(5):e632-5.
- Koide M, Inoue K, Matsuo A, Fujita H. Optical coherence tomography findings after longitudinal ablation for an underexpanded stent in a heavily calcified lesion: a case report. BMC cardiovascular disorders 2016;16(1):241.
- Vijayan S, Sultan A, West J, Gunn J. Rotational stent-ablation to treat under-expanded stents: Still the best method. International journal of cardiology 2016;223:262-264.







No comments yet!