Angiography-based quantitative flow reserve in coronary vasospastic angina
Supported by the EuroIntervention Journal
A 60-year-old woman with a history of cardiac arrest associated with MINOCA (myocardial infarction with no coronary artery disease) event in the territory of the left main artery, underwent coronary angiography for recurrent episodes of chest pain leading to 4 hospitalizations in the last 2 years...
Authors
Sebastian Steven1, Majid Ahoopai,1, Thomas Münzel1, Tommaso Gori1
Case summary
A 60-year-old woman with a history of cardiac arrest associated with MINOCA (myocardial infarction with no coronary artery disease) event in the territory of the left main artery (LAD) in 2017, underwent coronary angiography for recurrent episodes of chest pain at rest and under effort leading to 4 hospitalizations in the last 2 years.
Coronary angiography showed only coronary sclerosis without relevant epicardial stenosis. To clarify the role of CVsA (Coronary Vasospastic Angina) in this patient's angina pectoris symptoms, provocation testing by acetylcholine was performed during coronary angiography. Additionally, we used post-hoc quantitative flow ratio (QFR, Medis Suite 3.2) to quantify the severity of acetylcholine-induced vasospasm.
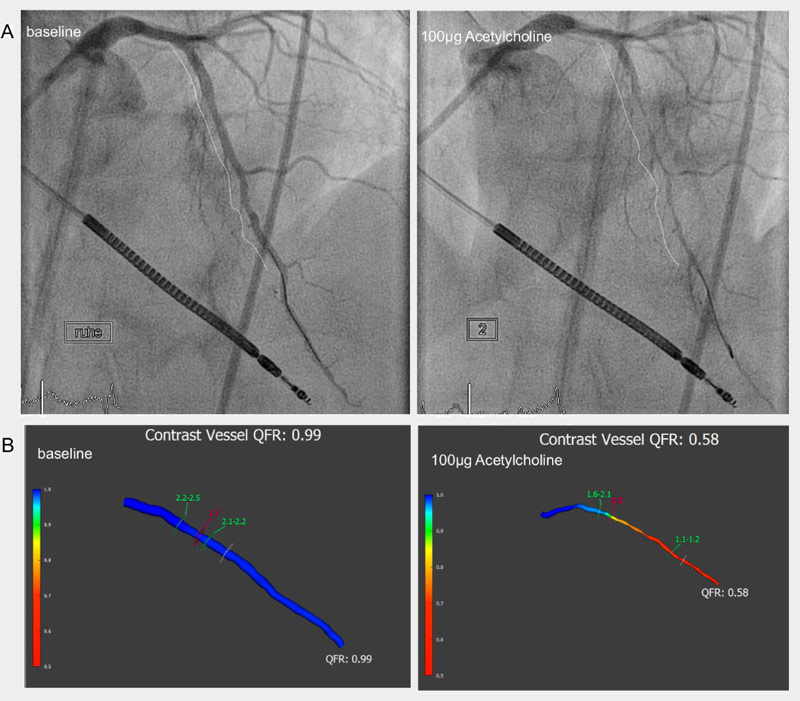
Figure 1. Angiography-based quantitative flow reserve in coronary vasospastic angina
A: Baseline angiography of a patient's left anterior descending artery (LAD). Intra coronary i.c. injection of 100µg Acetylcholine revealed vasospastic angina in this patient.
B: Segment 7 and 8 of the LAD were analyzed by Quantitative Flow Reserve (QFR) before (0.99) and after (0.58) injection of acetylcholine.
Coronary angiography of the LAD at rest excluded the presence of any epicardial stenosis (Figure 1A); the corresponding QFR value was normal (QFR 0.99, Figure 1B). Provocation of vasospastic angina was induced by intra coronary (i.c.) injection of 2, 20 and 100µg acetylcholine infused over 3 minutes. Evidence of vasospasm was present at 20µg in segment 7 and 8, and QFR dropped to 0.65 (not shown). Infusion of 100µg acetylcholine was associated with chest pain, a 1mm ST-elevation, and severe spasm of segments 7 and 8. QFR demonstrated a severe hemodynamic relevant stenotic LAD (QFR 0.58 (Figure 1A/B). Finally, application of nitroglycerin (i.c.) resolved patients' chest pain, ECG changes and vasospasm.
The patient was discharged with the diagnosis of vasospastic angina and medical therapy (calcium antagonist, short-acting nitrate).
Vasospastic angina is an underestimated cause of chest pain and myocardial infarction1. Acetylcholine testing is recommended by current guidelines2, and a 3D-quantitative coronary angiography coupled with QFR imputation might provide an accurate estimate of vascular responses to acetylcholine. Further research is needed to elaborate reference values for QFR in CVsA and how they might correlate to patients' risk for fatal cardiac events.
Conflict of interest statement
None
Affiliations
- Kardiologie I, Universitätsmedizin Mainz, and DZHK Standort Rhein-Main, Germany
References
- Bugiardini R and Cenko E. A Short History of Vasospastic Angina. J Am Coll Cardiol. 2017;70:2359-2362.
- Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ and Group ESCSD. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407-477.




No comments yet!