TACSI: Dual or single antiplatelet therapy after CABG in patients with acute coronary syndrome
Reported from ESC Congress 2025
Aaysha Cader provides her take on TACSI presented by Anders Jeppsson at ESC Congress 2025 in Madrid.
Courtesy of Aaysha Cader. Source: PCRonline.com
Why this study – the rationale/objective?
Current DAPT and revascularisation guidelines recommend dual antiplatelet therapy (DAPT) of aspirin and a P2Y12 inhibitor for 1 year in case of ACS patients post-CABG, and aspirin lifelong thereafter1-3. Despite this class I recommendation, uptake is low. Indeed, these recommendations are derived from extrapolations of non-CABG studies and sub-studies of ACS studies. Therefore, evidence to support DAPT post-CABG is limited.
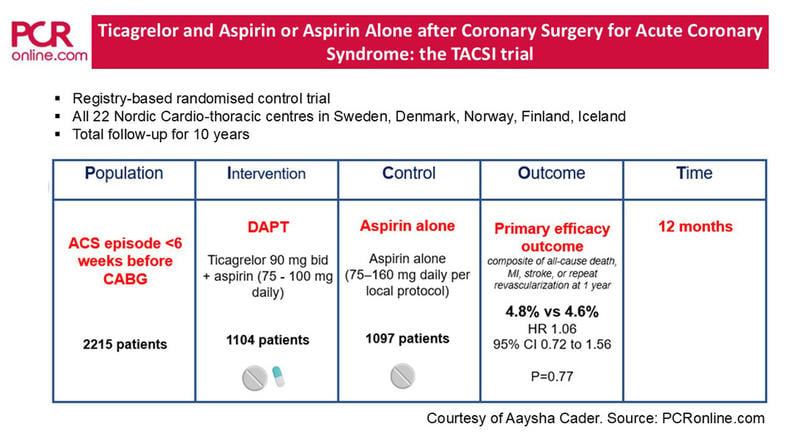
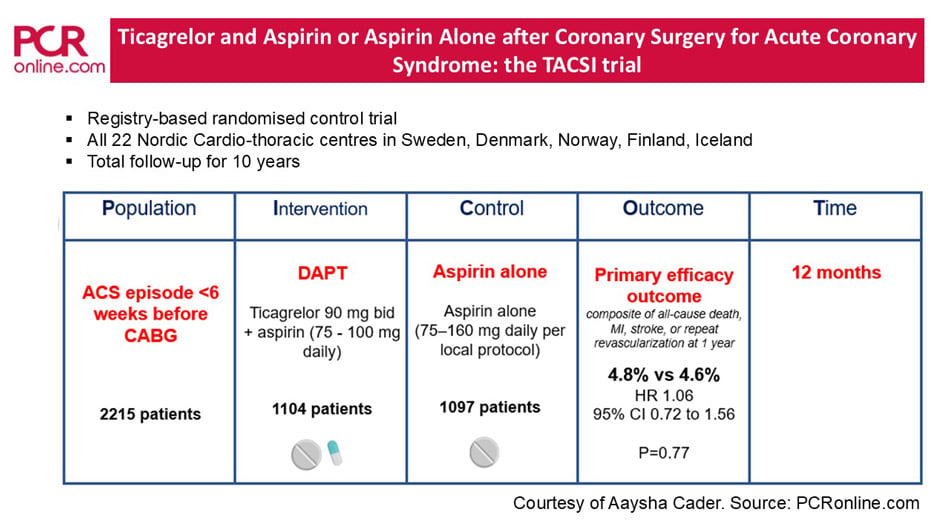
Aim: this registry-based randomised clinical trial (R-RCT) aimed to investigate among patients undergoing CABG after ACS, whether 12 months of ticagrelor + aspirin (DAPT) reduced clinical events as compared to aspirin alone, with respect to a composite major adverse cardiac events (MACE)4.
How was it executed - the methodology
Design: investigator-initiated, pragmatic, open-label, registry-based randomised clinical trial (R-RCT) conducted across all 22 nordic cardiothoracic surgery centres (Sweden, Denmark, Norway, Finland, Iceland). In this pragmatic R-RCT, background and outcome variables were captured from existing national health care registries and databases.
PICO criteria
- Population: Adults > 18 years of age, who had an ACS that occurred within 6 weeks before a primary isolated CABG, and provided written informed consent 3 to 14 days after CABG
Major exclusion criteria:- concomitant surgical procedure
- contraindication to either of the trial drugs, treatment with oral anticoagulants, any other indication for DAPT (e.g. recent stents)
- chronic kidney disease warranting dialysis
- severe liver disease
- bleeding disorder
- Intervention: DAPT: ticagrelor 90 mg bid + aspirin (75 - 100 mg daily)
- Comparator: aspirin alone (75–160 mg daily per local protocol)
- Outcomes: primary efficacy outcomes was composite of all-cause death, MI, stroke, or repeat revascularisation, evaluated in time-to-event analysis at 1 year. Primary safety outcome was the first occurrence of major bleeding (warranting hospitalisation), also evaluated in a time-to-event analysis at 1 year
Randomisation: patients were randomised 3 to 11 days after CABG following an ACS, in 1:1 ratio to receive either DAPT or aspirin alone for 1 year. Randomisation was stratified according to trial centre. P2Y12 inhibitors were omitted at guideline-recommended durations prior to CABG; aspirin was continued.
Sample size: assuming an 8 % incidence of 1 year MACE with aspirin alone, a sample size of 2,200 would be needed for 80 % power to detect a 38.5 % relative risk reduction with DAPT, at two-sided alpha level of 0.05
Main analyses were conducted in the intention-to-treat (ITT) population.
What is the main result?
A total of 2,215 patients were randomised. In the ITT population, 1,104 patients were assigned to DAPT and 1,097 to receive aspirin alone.
Baseline characteristics were well-balanced between both groups. The mean age was 66 years, 14.4 % were women, 27.5 % had diabetes, and the median EuroSCORE II score was 1.6 %. NSTEMI (57.6 %) was the predominant indication, 32.1 % had unstable angina, and 10.2 % had STEMI.
Primary outcome
In the ITT population, the primary efficacy outcome (MACE composite) event occurred in 53 patients (4.8 %) in the ticagrelor-plus-aspirin group, and in 50 patients (4.6 %) in the aspirin-alone group (hazard ratio, 1.06; 95 % confidence interval [CI], 0.72 to 1.56; p = 0.77), with Kaplan-Meier curves crossing three times over the 1 year of analysis. Key secondary outcome of net adverse clinical events (defined as the components of the primary outcome or major bleeding) occurred in 9.1 % in the DAPT arm, and 6.4 % in the aspirin-alone arm (HR, 1.45; 95 % CI, 1.07 to 1.97)
The primary safety outcome, a first occurrence of major bleeding occurred in 4.9 % in the ticagrelor-plus-aspirin group, and in 2.0 % in the aspirin-alone group (HR, 2.50; 95 % CI, 1.52 to 4.11).
An adjusted analysis of the primary and key secondary outcomes in the per-protocol population appeared to be consistent with that in the ITT population.
Critical reading and the relevance for clinical practice
Although DAPT improves short- and long-term outcomes in patients who have had percutaneous coronary intervention (PCI), this can clearly not be extrapolated for CABG patients, likely because revascularisation by CABG involves arterial and venous grafts, wherein pathophysiologies may vary. Furthermore, graft failure may also be compounded by poor harvesting techniques, which are unlikely to be mitigated by antiplatelet therapy.
Previous studies have led to the suggestion that antiplatelet therapy might be associated with better long-term outcomes, likely mediated by reducing graft failure, which in turn predicts events5-7.
A meta-analysis of RCTs comparing DAPT and SAPT in a mixed CABG population (i.e. including urgent and non-urgent CABG), showed lower SVG occlusions at 1 year with DAPT, albeit no differences in cardiovascular death, but higher incidence of major bleeding5. A more contemporary individual patient data meta-analysis including 4 RCTs found that adding ticagrelor to aspirin significantly decreased risk of SVG failure, but also significantly increased risk of clinically important bleeding6.
In a Chinese trial, DAPT was associated with greater graft patency, but no difference in clinical outcomes, although it was not powered to detect them7.
While it is clear from this study that 12 months DAPT vs aspirin does not reduce clinical events, it will be interesting to see what the results of the 360 patients in the graft patency substudy at 12-36 months. It should also shed more light on the concept that perhaps the role of DAPT is in reducing specific mechanisms of graft failure.
Despite its pragmatic registry-based design, which facilitates efficient recruitment of large numbers of patients, the trial had several limitations, notably a lower-than-expected event rate and large effect size of 38.5 % RRR used to calculate the sample size, both of which meant that the trial was underpowered for the detection of small differences in clinical events. The open-label design however is unlikely to have influenced the evaluation of events, which are hard endpoints. Non-adherence was also significant, with the DAPT arm showing thrice as much greater discontinuation of trial treatment than the aspirin arm.
And finally, this trial was of 12 months DAPT, therefore the jury is still out there on whether a shorter period of DAPT, and one commencing prior to the 3rd day post-CABG, might be more advantageous than a 12-month duration, by reducing bleeding complications.
References
- Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for CardioThoracic Surgery (EACTS). Eur Heart J 2018;39:213-60.
- Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J 2023;44:3720-826
- Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022;145(3):e18-e114. 5. Sousa-Uva M, Neumann FJ, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur J Cardiothorac Surg 2019;55:4-90.
- Jeppsson A, James S, Moller CH, et al; TACSI Trial Group. Ticagrelor and Aspirin or Aspirin Alone after Coronary Surgery for Acute Coronary Syndrome. N Engl J Med. 2025 Sep 1. doi: 10.1056/NEJMoa2508026. Epub ahead of print.
- Cardoso R, Knijnik L, Whelton SP, et al. Dual versus single antiplatelet therapy after coronary artery bypass graft surgery: an updated meta-analysis. Int J Cardiol 2018;269:80-8
- Sandner S, Redfors B, Angiolillo DJ, et al. Association of dual antiplatelet therapy with ticagrelor with vein graft failure after coronary artery bypass graft surgery: a systematic review and meta-analysis. JAMA 2022;328:554-62
- Zhao Q, Zhu Y, Xu Z, et al. Effect of ticagrelor plus aspirin, ticagrelor alone, or aspirin alone on saphenous vein graft patency 1 year after coronary artery bypass grafting: a randomized clinical trial. JAMA 2018;319:1677-86
Latest news from ESC Congress 2025




No comments yet!