29 Jan 2026
How to close vascular access with a combined suture-/plug-based strategy using one ProStyle and one Angio-Seal in TAVI
A problem-solving step-by-step tutorial
Large-bore femoral access closure remains a critical step in transfemoral TAVI, where access-site complications can significantly impact outcomes.
This My Toolkit article presents a step-by-step tutorial on a combined suture- and plug-based closure strategy using one ProStyle™ and one Angio-Seal®. The technique aims to achieve rapid, reliable haemostasis while reducing vascular complications in routine and challenging TAVI cases.
Frequency of the problem:
Expert level:
Summary
Over the last decade, remarkable progress in technology and techniques has contributed to increasing efficacy of TAVI procedures, leading to its expansion to patients with lower surgical risks, where even higher levels of safety are required.
Although transfemoral access has been reported as superior to other routes of access, access-site complications remain one of the most common Achilles’ heels of transfemoral TAVI. With the combined suture-/plug-based vascular closure strategy using one ProStyle and one Angio-Seal, you can:
- Experience fewer access-site related vascular complications;
- Shorten time to haemostasis;
- Reduce the risk of subacute access-site bleeding;
The problem
Access-related vascular complications such as peripheral limb ischaemia, access-site stenosis, pseudo-aneurysm, and haematoma are encountered on a frequent basis, having a detrimental effect on morbidity and mortality of patients undergoing TAVI.
With the availability of several types of vascular closure devices (VCD), strategies have varied between operators. The recent ACCESS-TAVI trial demonstrated that patients undergoing TF-TAVI have significantly fewer access site-related vascular complications and shorter time to haemostasis with a combined suture- and plug-based VCD strategy using one ProGlide™/ ProStyle™ (Abbott Vascular) and one Angio-Seal® (Terumo) versus a suture-only VCD strategy using two ProGlides™/ ProStyles™ 1. This highlights the increasing need to master the combined strategy.
Principal idea
ProGlide™/ ProStyle™ are nitinol-guided, suture-based VCD used to close the arterial access site. Angio-Seal® is a plug-based VCD containing three bio-absorbable components for active vascular access closure : an extra-vascular bioabsorbable collagen, an intra-vascular anchor, and a bio-absorbable suture that holds the two other active components together. It is available in two sizes : 6F or 8F.
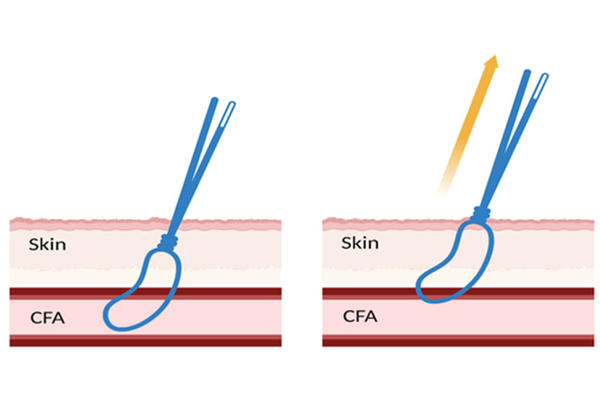
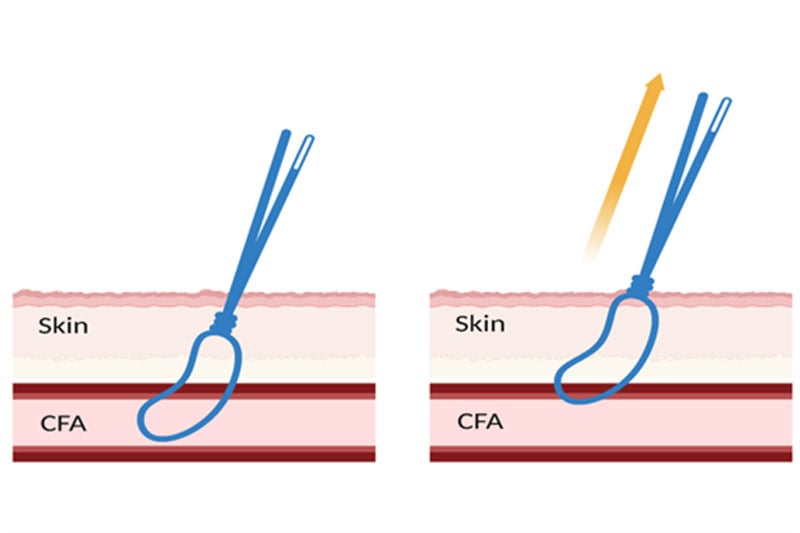
At the beginning of the TAVI procedure, one ProStyle™ is deployed before inserting the large-bore introducer sheath. After valve deployment, the suture of ProStyle™ is tightened as the introducer sheath is removed, with a safety wire left in the artery, followed by the application of one 8F Angio-Seal®.
Material needed
- One ProGlide™/ ProStyle™, wire (0.0035 inch), mosquito forceps, one Angio-Seal®
- Preferably: peripheral ultrasound with colour Doppler
Method step-by-step
Step 1
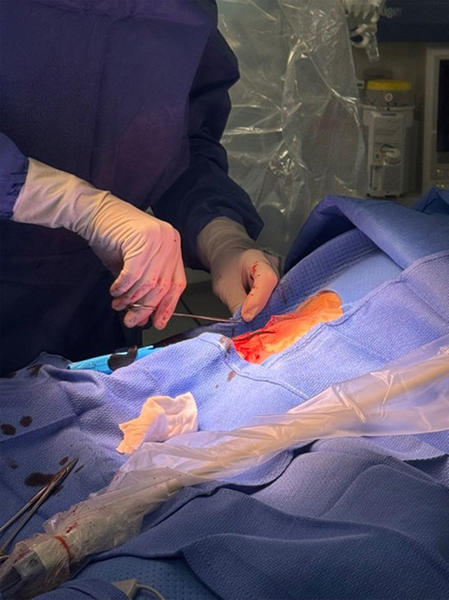
The arterial site is preferably scanned with ultrasound, so the area with minimal calcification is punctured under its guidance. After puncture, dissect the subcutaneous tissue with blunt forceps, then dilate the artery with a minimum of 6Fr sheath.
Advance ProStyle™, lift the lever open (labelled #1 on the device), maintain retraction, and depress the plunger (labelled #2). While maintaining retraction, pull back the plunger to deploy suture (labelled #3). Then, cut the plunger off by cutting the blue suture and lower the foot (labelled #4).

Step 2
Remove the two suture ends from the device, and gently keep it in place with mosquito forceps (remove the slack) while the procedure continues.
A 0.0035" wire is inserted into the guidewire exit port of the ProStyle™, and then ProStyle™ is exchanged with a larger-bore introducer sheath. During TAVI, aim for an ACT to 250 seconds.

Step 3
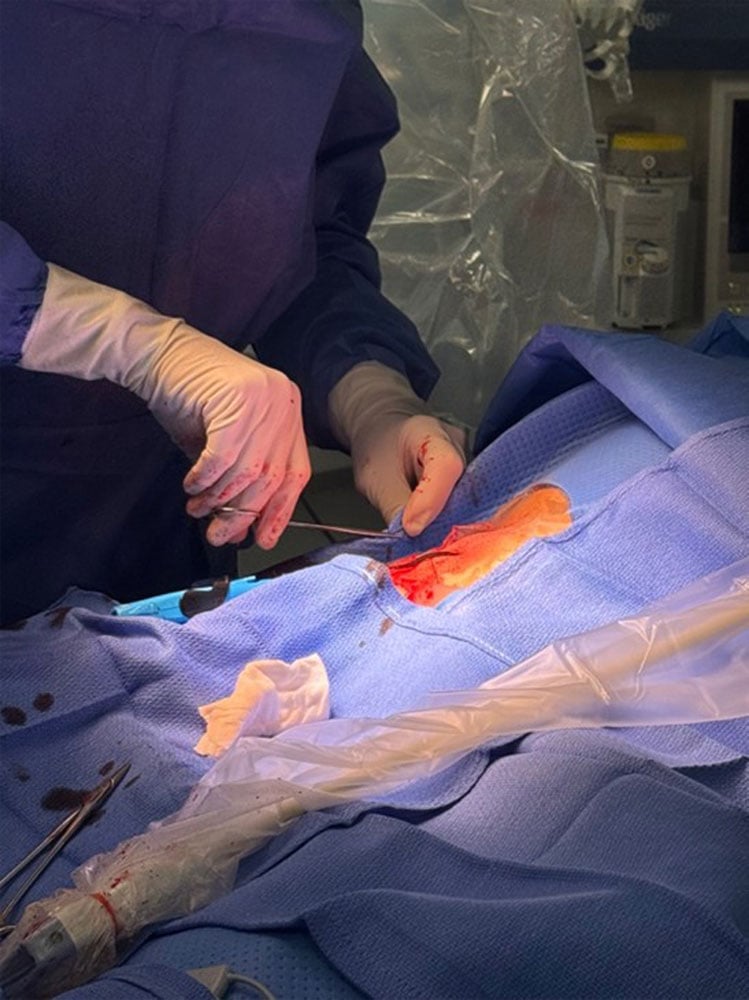
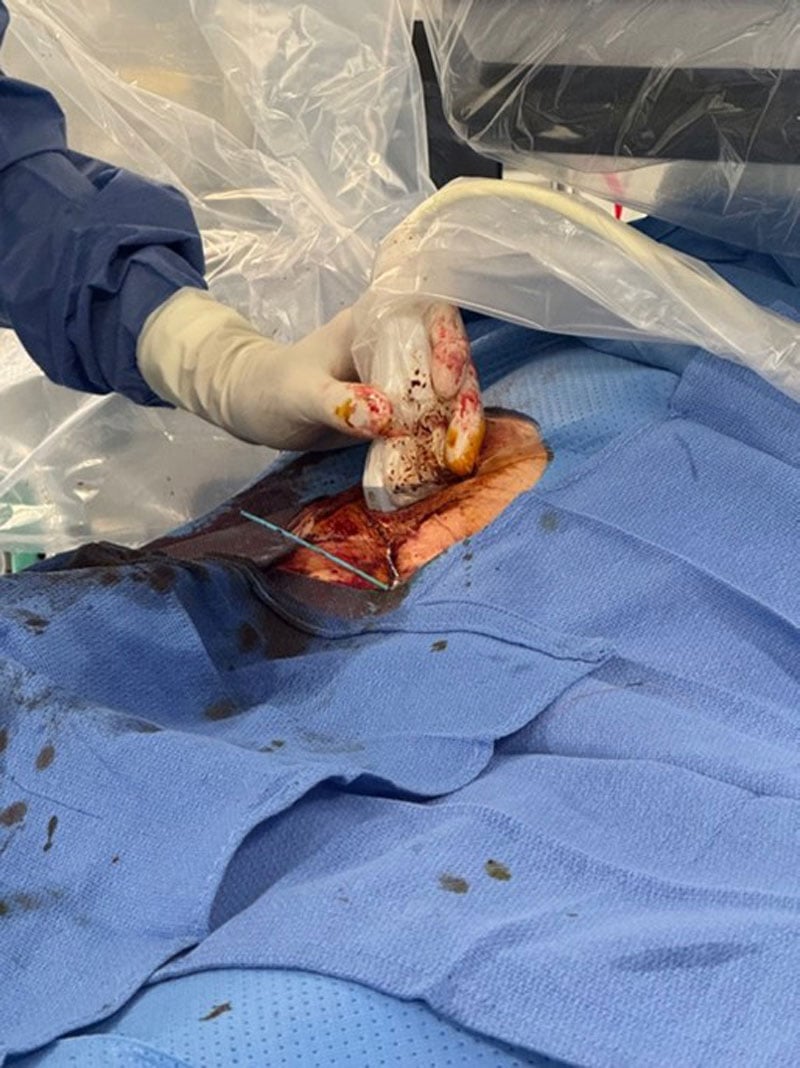
After the valve deployment, as the introducer sheath is extracted with the safety wire left in the artery, apply tension to the blue suture (rail suture) of ProStyle™ by wrapping it around your left index finger and advancing the suture trimmer with your left thumb, while the tension is applied co-axially to the direction of the artery. Advance the knot gently by maintaining soft, coaxial tension.

Step 4
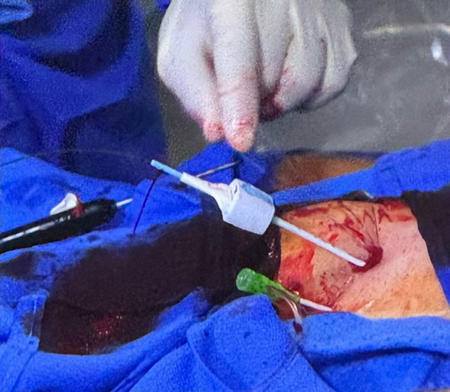
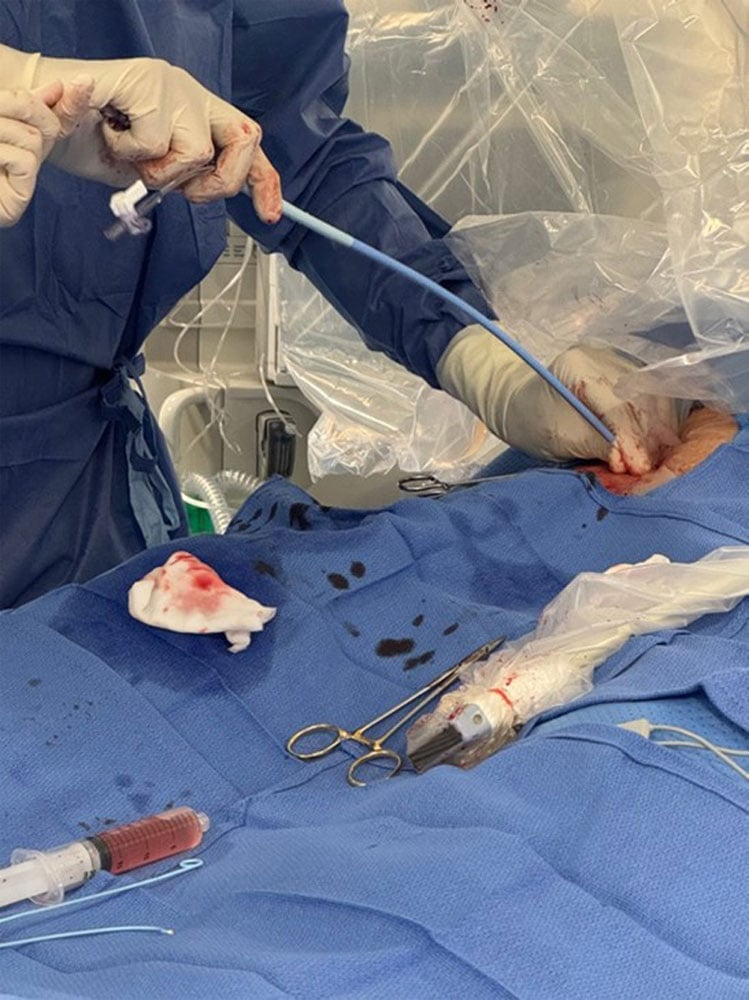
Allow the second operator to advance 8F Angio-Seal® locator system through the safety wire. Assess the degree of oozing from around the locator system. If there is no or minimal oozing, proceed to Step 5.
Step 5
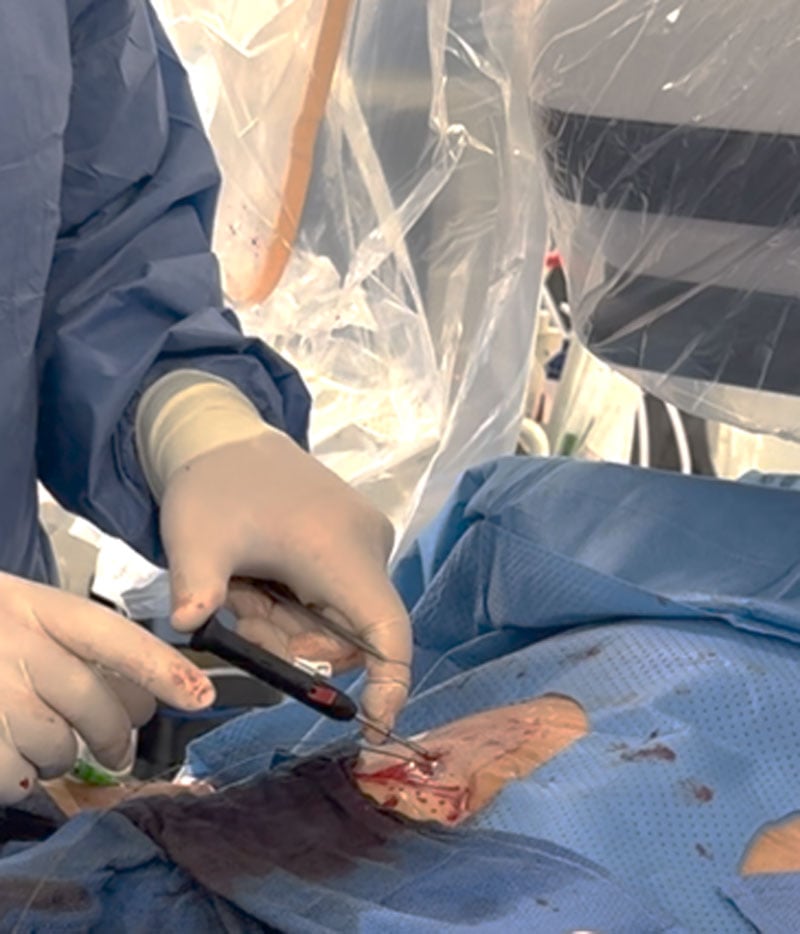
With the locator in the proper depth, insert the Angio-Seal VIP device into the sheath. Maintain grip on the insertion sheath and gently pull the device cap straight back until resistance is felt and both device sleeve bands are fully visible.
Gently pull back on the Angio-Seal® VIP device, following the angle of the puncture tract until the suture stops spooling. Maintain tension on the suture and gently advance the compaction tube until resistance is felt.
Cut the suture of Angio-Seal® below the clear stop and remove the device. Cut the remaining sutures of Angio-Seal® and ProStyle™ below the skin level.
Step 6
Check the degree of residual oozing from the puncture site. If there is residual bleeding, apply manual compression for at least 3 minutes before additional measures, such as endovascular ballooning or covered stent implantation. Full or half heparin antagonisation (1000 IU of protamine/1000 IU of heparin or 500 IU of protamine/1000 IU of heparin) may be considered in case of subcutaneous bleeding.
Step 7
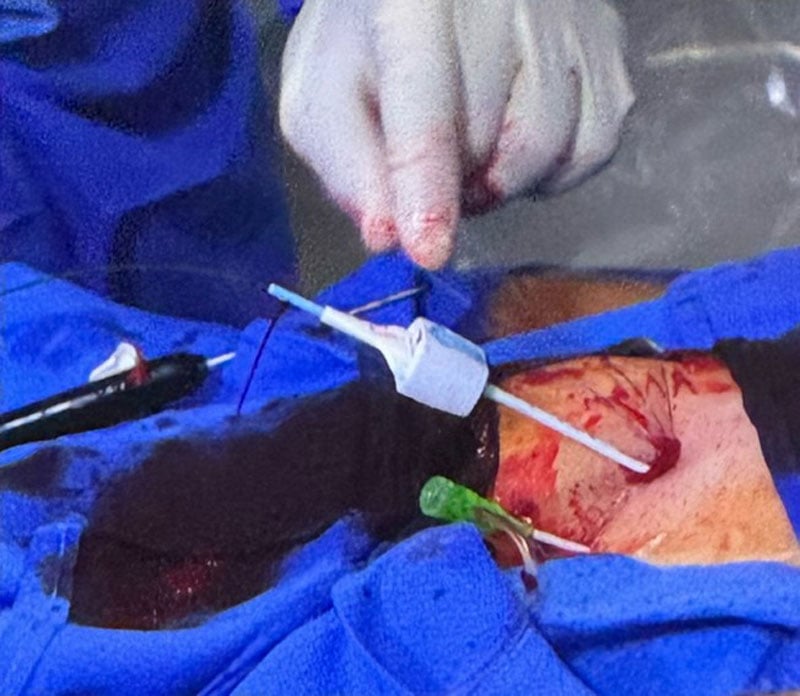
Check the arterial flow with ultrasound by locating the long-axis of the artery first, then acquiring a colour-Doppler image. Arterial flow should be pulsatile on both proximal and distal portions of the puncture site, with an acoustic shadow below the plug of Angio-Seal®.

Points of specific attention
- A purely plug-based vascular closure technique was associated with access-site related complications, whereas double ProGlide technique often required additional VCDs to achieve haemostasis. The combination of two different modes of closure provides the most effective and safe method of haemostasis.
- In Step 4, if the bleeding is significant even with the Angio-Seal® locator in place, do not directly go to Step 5. Instead, retreat Angio-Seal®, advance the second ProStyle™, repeat Steps 1-4, place the safety wire back in, and then proceed with 8F Angio-Seal® to Step 5. This approach allows you to place two ProStyles™ before placing the Angio-Seal® in case of significant bleeding.
- In case the residual bleeding after 2 ProStyles™ is still relevant, check for major complications before putting the Angio-Seal® and removing the wire: this will allow you to put a 6-10F sheath and inflate a balloon if necessary.
A word from the reviewer
Vascular closure strategies for large-bore femoral TAVI access remain of critical importance for the success of the entire procedure. Vascular access site complications and bleeding have been associated with adverse outcomes and significant morbidity and mortality in multiple studies. Hence, every effort should be made to provide a simple and yet safe and effective technique for percutaneous closure of large-bore femoral access.
The authors offer a concise step-by-step approach for a combined suture- and plug-based closure strategy that may offer efficient hemostasis and is yet simple, quick and reproducible. As they state, identification of an optimal puncture site is key for the success of the technique. Ultrasound is an effective tool to guide puncture and to avoid vessel segments with significant atheroma burden or calcific plaques. After suture-based closure following the TAVI procedure, residual oozing at the access site determines whether a plug-based device (6 French or 8 French) can be inserted or an additional suture-based closure device should be introduced first. Angiography via a 6 French sheath may additionally help to identify potential complications and guide the optimal next step, as suggested by the MultiCLOSE vascular algorithm1. As nicely illustrated in the My Toolkit article, final ultrasound is a further important step to allow for the immediate identification of closure-related complications and initiate early management, if required.
Following, a step-by-step algorithm, as beautifully illustrated by the authors in this article, will allow for safe and effective vascular closure in the majority of cases. TAVI operators should familiarise themselves with these techniques to achieve optimal procedural results for our patients.
- Rosseel L et al EuroIntervention DOI: 10.4244/EIJ-D-23-00725
Conflicts of interest
Dr. Seiffert reports receiving lecture fees from Abbott Vascular, Abiomed, AstraZeneca, Boston Scientific, Bristol-Myers Squibb, Edwards Lifesciences, Medtronic, Amgen, Shockwave Medical, Daiichi Sankyo, Pfizer, Inari Medical, and Bayer, all outside the submitted work.
Disclosures
The authors declare that they have no conflicts of interest.
Reference
- Rheude T, Ruge H, Altaner N, Pellegrini C, Alvarez Covarrubias H, Mayr P, Cassese S, Kufner S, Taniguchi Y, Thilo C, Klos M, Erlebach M, Schneider S, Jurisic M, Laugwitz KL, Lange R, Schunkert H, Kastrati A, Krane M, Xhepa E, Joner M. Comparison of strategies for vascular ACCESS closure after Transcatheter Aortic Valve Implantation: the ACCESS-TAVI randomized trial. Eur Heart J. 2025 Feb 14;46(7):635-645. doi: 10.1093/eurheartj/ehae784. PMID: 39474906.
Authors









2 comments
We do uae the same Technique but we tigthen the ProStyle suture over a 6 Fr sheath, if there is no bleeding, we deploy the AngioSeal, if it stille bleeds we remove the sheath, insert another ProStyle then the 8 Fr AngioSeql
If the Proglide sutures are already tightened, how can the Angiseal sheath be guaranteed to be pushed in through the retained guidewire?