18 Nov 2024
The DCB kissing technique as a durable solution in treatment of recurring left main in-stent restenosis
A 73-year-old male with complex recurrent in-stent restenosis of the left main underwent an innovative treatment approach. Six-month follow-up revealed remarkable recovery and positive remodelling. Discover how Piotr Buszman and Mateusz Kachel tackled this challenging case.
Authors
Clinical presentation
A 73-year-old male patient with insulin dependent diabetes mellitus, heart failure with preserved ejection fraction hyperlipidemia and hypertension, presenting with a chest pain, was admitted to our Clinic with a non-ST-elevation myocardial infarction (NSTEMI).
The patient had a history of multiple coronary interventions (prior PCI RCA and LM/LAD), most recently (three months ago) with an NSTEMI and a restenosis in the left main treated with 2 EES.
He was previously disqualified from CABG due to the unfavorable anatomy of diffusely disease medial and distal LAD. The echocardiography on admission showed regional wall motion abnormalities in the form of interventricular septum (mid and distal portion) and apex hypokinesis with systolic dysfunction (mildly reduced ejection fraction; EF=40%).
Following these findings, the patient was immediately transferred to the cath lab. The invasive coronary angiography was performed and critical in-stent restenosis in distal left main, as well as in ostial part of LAD and LCX was seen (Video 1).
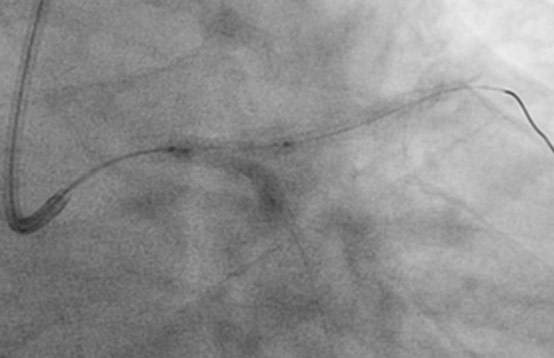
Following vessel wiring an initial lesion preparation and stent postdilation with a kissing NC 2.5x15 mm (LCx) and NC 3.0x15 mm (LM) was performed (Figure 1), after which IVUS did not reveal malaposition. An optimal revascularization was achieved with residual stenosis of 30% (Video 2).

Figure 1. Pre-dilatation with kissing NC 2.5x15 mm and NC 3.0x15 mm.
Considering the recurrent character of in-stent restenosis in a two-stent bifurcation, implantation of another stent would not be feasible and most likely risk the permanent occlusion of LCx. Wishing to avoid further stent placement and given the currently favorable evidence for drug-coated balloons (DCBs) in in-stent restenosis, we decided to proceed with postdilation kissing DCB technique for thirty seconds – twice to provide sufficient drug release and avoidance of significant ischemia.
Kissing balloon inflation (KBI) consists of the simultaneous inflation of two balloons in both the main vessel (MV) and the side branch (SB). Also, simultaneous balloon deflation is crucial to reduce the bifurcation carina shift and to maintain the centrality of present metallic stent struts.
SeQuent® Please NEO is a paclitaxel-coated DCB with proprietary polymer-free paclitaxel / iopromide drug coating technology that ensures a predictable drug delivery, long-term drug retention in target site and largest scientific portfolio providing its safety and efficacy.
A PTCA utilizing 2 SeQuent® Please NEO DEB - 3,0 x 20 mm and 2,0 x 20 mm was performed. Each balloon was inflated for 30 seconds twice (Figure 2). An optimal angiographic, TIMI 3, with full stent expansion in LM and ostial LAD was achieved. A slight (30%) residual restenosis was present in LCX (Video 3).

Figure 2. Inflation and kissing of 2 SeQuent® Please NEO DEB - 3,0 x 20 mm and 2,0 x 20 mm.
The following was confirmed in IVUS imaging that showed a full expansion of stent in LM and satisfactory MLA numbers in ostial LAD 4.2mm2 and ostial LCX 4.1mm2. Knowing the positive remodelling capabilities of paclitaxel-coated balloon, this result was considered satisfactory. The patient was discharged home in good clinical standing.
Final outcomes
The patient was admitted to the Clinic six months after baseline procedure for a control angiography. Echocardiography on admission showed no wall motion abnormalities and significantly improved systolic function (EF 63%).
The invasive coronary angiography confirmed an improved effect of previous intervention with no in-stent restenosis and no residual stenosis in LM/LAD/LCX present (Video 4).
Clearly, a positive remodelling effect with no residual stenosis was reported. After an optimization of pharmacotherapy, the patient was discharged home in good standing.
This case of a multiply recurring in-stent restenosis in particularly challenging territory of the left main highlights the need to search for stent-free techniques in selected clinical scenarios and enhances their value.
Paclitaxel-coated balloons provide an excellent alternative to stents, especially when positive remodelling is desired, in lesions and patient subsets where stents are not desirable, such as in-stent restenosis, two stent bifurcations, diffuse disease especially in small vessels, important ostial side branch, patients unable to take DAPT either due to bleeding issues or awaiting important surgery. Treatment of in-stent restenosis (DES and BMS) with DCB should be a first line approach whenever good angiographic outcome with lesion preparation is achieved.
It is also a promising treatment option for de-novo coronary lesions. However, more data supporting this technology and technique are warranted. New generation technology will focus on further coating optimization, as well as more predictable local delivery and drug retention.





4 comments
May I ask what was the LM stent size from the initial PCI?
Kissing balloon with DCB is not recommended. Also is better to use 1:1 balloon /artery ratio so use 2.0 balloon seems to be small for Cx
Good job, gay's!!!) What you think about Diag 1 and OM2 branches? For me, it's needs in 2 DCB also, Thanks
Nice case, thank you. Please consider that delivery time until balloon inflation is crucial to avoid drug loss. Also a second inflation might not add a lot of drug. Nevertheless a very nice success and certainly worthwhile to communicate