24 Mar 2020
How to use a Rotablator as single operator
A single operator technique simplifies the procedure and removes the dependence on having a trained assistant. Discover the tips and solutions proposed by Joshua Loh.
Frequency of the problem:
Expert level:
Summary
Rotational atherectomy for plaque modification can be technically challenging. Besides being familiar with the Rotablator equipment, the operator must be able to work well with an experienced assistant. The usual way of advancing a burr requires the operator and an assistant to work in perfect sync, otherwise, there is a risk of losing wire position.
A single operator technique simplifies the procedure and removes the dependence on the assistant. The operator is able to advance the burr over the wire with the left hand while the right hand simultaneously pulls the wire back the same distance. The operator monitors the wire position and burr movement constantly under fluoroscopy. This gives the operator full control. After plaque modification is completed, the burr can also be removed by a single operator technique.
The problem
The usual way of advancing a burr requires the operator and an assistant to work in perfect sync. The assistant fixes the wire in position at the end of the catheterization lab table while the operator advances the burr and driveshaft. As an over-the-wire system, the entire system has to be kept straight. Any accidental movements may risk losing wire position. However, an experienced assistant is not always available, and the operator may be performing rotablation in an unfamiliar catheterization lab either as a proctor or for live demonstration purposes. A single operator technique simplifies the procedure and removes the dependence on having a trained assistant.
Principal idea
A single operator technique for rotablation removes the dependence on the assistant. The operator is in full control. The burr is advanced over the wire with the left hand while the right hand simultaneously pulls the wire back the same distance. While performing this manoeuvre, the operator monitors the wire position and burr movement constantly under fluoroscopy. After plaque modification is completed, the burr can also be removed by a single operator technique by opening the Y-connector valve while pushing the wire forward on “Dynaglide” mode.
Material needed
The rotablator burr comes with its own advancer and a WireClip torquer. A 6 Fr guiding catheter can accommodate a 1.25 mm or 1.5 mm burr, while a 7 Fr or 8 Fr guiding catheter can accommodate up to 1.75 mm or 2 mm burr respectively. A Rotawire Floppy or Extra Support can be used. A Rotaflush system either with RotaglideTM lubricant or 10,000 units of heparin and vasodilator cocktail in a 1 L bag of normal saline reduces friction and heat generation. A Y-connector hemostasis valve is attached to the end of the guiding catheter.
Method step-by-step
Step 1: Preparing to advance the burr

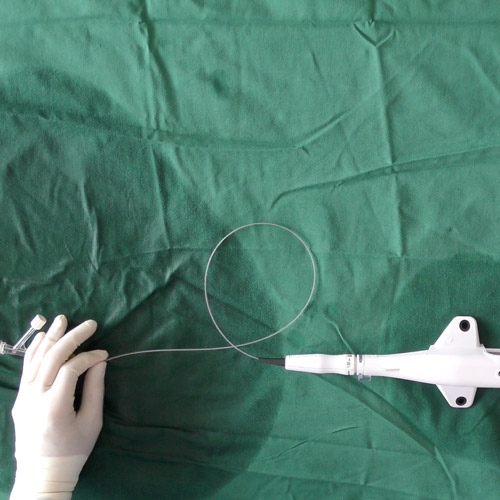
Figure 1. The burr is advanced over the wire until 2-3cm from the Y-connector. The burr is tested and primed at >150000rpm with the WireClip torquer clipped onto the wire.

Figure 2. The advancer is moved close to the Y-connector. The burr shaft forms a big loop.

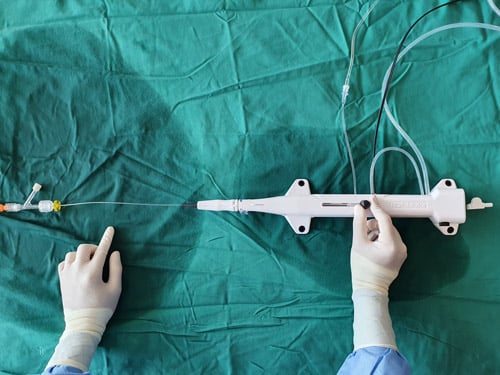
Figure 3. The brake defeat button is depressed, and the Wireclip torquer is slotted in correctly. This allows the wire to move freely.
Step 2: Advancing the burr within the guiding catheter
- The left hand advances the burr shaft, while the right hand simultaneously pulls the wire back the same distance.
- The loop of the burr shaft becomes smaller as the burr is advanced and the wire is pulled back. (Fig 4, Vid 1).

Figure 4.
- The operator monitors the wire position, burr movement and guiding catheter position constantly under fluoroscopy at low magnification. (Fig 5, Vid 2).

Figure 5.
- The burr is advanced beyond the guiding catheter and proximal to the lesion. The loop of the burr shaft is no longer present. The brake defeat button is released and the wire is locked. The WireClip torquer is clipped onto the wire (Fig 6). Plaque modification with rotablator can now be performed.

Figure 6.
Step 3: Removing the burr
- The brake defeat button is depressed, and the Wireclip torquer is slotted in correctly. This allows the wire to move freely.
- The Y-connector hemostasis valve is left open for the burr to exit.
- Activating constant ‘Dynaglide’ mode, a rapid pushing of the wire forward will propel the burr backwards until it exits the guiding catheter and Y-connector (Vid 3).
- The operator monitors the wire position, burr movement and guiding catheter position constantly under fluoroscopy at low magnification.
Points of specific attention
While advancing the burr within the guiding catheter, the operator should be monitoring the fluoroscopy screen closely, with particular attention on the wire position. The operator can adjust the left or right hand movements accordingly. If the wire advances too forward, more right hand pull of the wire is necessary. If the wire comes back, less right hand pull of the wire will correct the wire position.
In case the burr faces resistance at the guiding catheter curve, either of the following 2 manœuvres may be used:
- Simple ‘tug-and-pull’ movement (firm pushing of the shaft with the left hand and equally firm pulling of the wire with the right hand) while monitoring guiding catheter position.
- Activating a short burst of ‘dynaglide’ to bring the burr across the curve.







7 comments
Fantastic method! No coordination between two operators needed. We are currently trying to apply this within the entire team since it definitely reduces the threshold to use the rotablator when needed and thus simplifies PCI I calcified vessels. Takes a few attempts, but definitely worthwhile trying!
Great Congratulations
we are geting training this tecnique .thanks a lot
Thanks
Why brake defeat while advancing?
Thanks for making complicated procedural steps in to easysteps and building confidence to use Rota
Thankyou for this very vivid presentation ! I will implement this in my daily practice.