The effectiveness and safety of a planned investment procedure in high-risk chronic total occlusions - The INVEST CTO single arm study
Reported from TCT 2025
Kalaivani Mahadevan and Sofia Papadopoulou provide their take on the INVEST CTO trial, presented by Anja Oksnes at TCT 2025, in San Francisco.
Study rationale
Despite major advances in techniques, algorithms and equipment, chronic total occlusions (CTO) remain the most challenging percutaneous coronary intervention (PCI) lesion subset with success dependent on patient and anatomical complexity, procedural strategy and operator skillsets.
All-comer CTO-PCI success is consistently high at 80–90 % across three contemporary registries from centres with dedicated CTO programmes (UK Hybrid, PROGRESS-CTO, OPEN-CTO)1–3. However, with increasing anatomical complexity, strategy escalation across the hybrid algorithm to more complex techniques is required, and first attempt technical success rates fall1,2. As J-CTO score rises, antegrade wire escalation (AWE) use declines sharply, with retrograde and antegrade dissection–re-entry (ADR) techniques increasingly utilised for crossing and procedural completion (Figure 1).
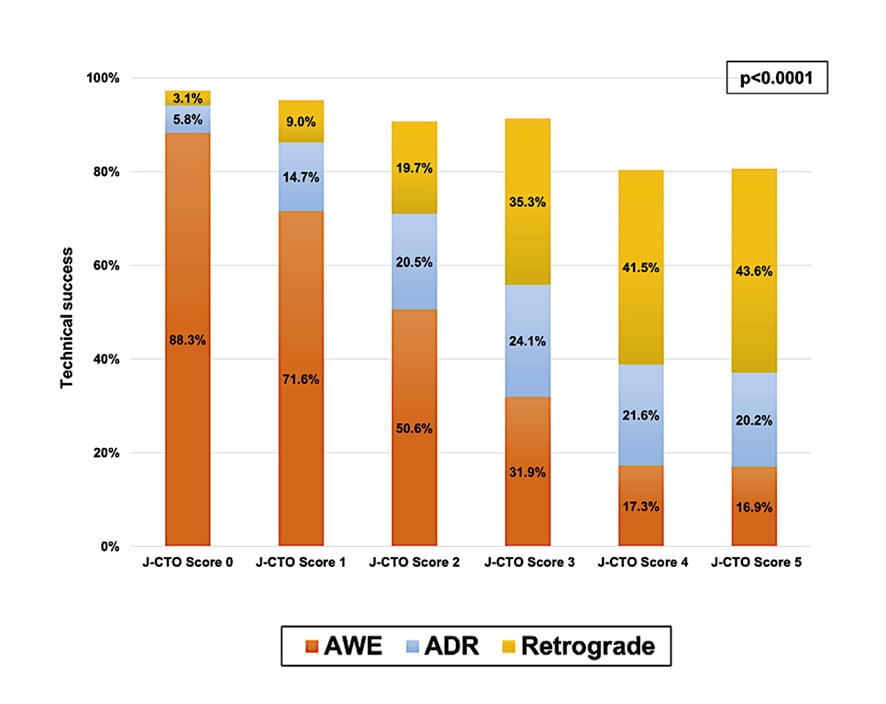
Figure 1. Technical success and crossing-strategy use according to J-CTO Score2.
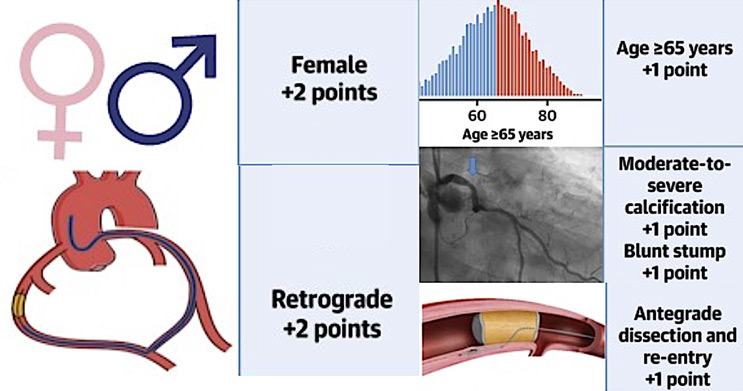
Complication frequency and severity also rises with CTO complexity. The PROGRESS-CTO complication prediction score demonstrates higher event risk with increasing lesion and procedural complexity with +1 and +2 points assigned for ADR and retrograde approaches respectively (Figure 2)4.
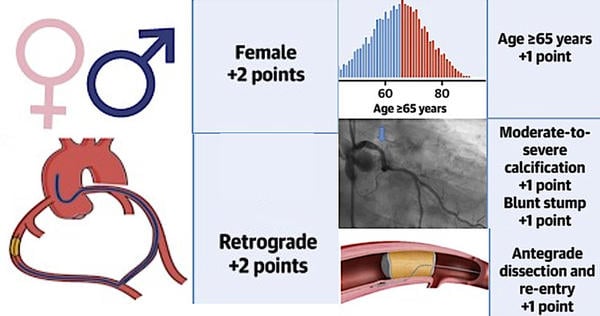
Figure 2: PROGRESS CTO complication risk score
Figure courtesy of Simsek B et al. JACC Cardiovasc Interv. 2022 Jul 25;15(14):1413-1422
In cases of failed re-entry into the distal true lumen, extraplaque ballooning for plaque modification can facilitate subsequent lesion recanalisation and improve likelihood of success at re-attempt (‘modification procedure’). Currently, ‘modification procedures’ are utilised in a bail-out manner which does not offset longer procedural duration, potential complications, contrast load, and x-ray dosage incurred during the unsuccessful index procedure5.
The above observations support the rationale for a planned, up-front ‘investment procedure’ with follow-on ‘staged completion’ to explore the feasibility, safety and success of an evolving stepwise strategy for high-risk CTO lesions6.This was the objective of the INVEST CTO study.
Study methodology
Design:
This was a prospective, single-arm, international, multicentre study (dedicated CTO PCI centres in Norway, USA and UK).
Population:
153 patients with symptomatic angina and anatomically high–risk CTO’s.
Key eligibility:
CTOs meeting the study’s high-risk criteria (Figure 3) were included6; flush aorto-ostial and in-stent occlusions alongside prior attempt on the target lesion CTO within 6 months were key exclusion criteria.
Intervention strategy:
Planned two-stage approach with an initial ‘investment procedure’ (lesion modification without full revascularisation) followed by completion CTO-PCI at 8–12 weeks.
Primary endpoint:
Procedural success (cumulative after completion stage, and defined as both technical success and the absence of in-hospital MACE)
Secondary endpoints:
Patient-reported outcomes (symptoms/QoL), treatment satisfaction, and clinical endpoints (30 days, 3 and 12 months).
Statistical plan:
Non-inferiority testing was performed against an external benchmark of 75 % procedural success (based on historical/ registry data) with a non-inferiority margin set at 10 %.
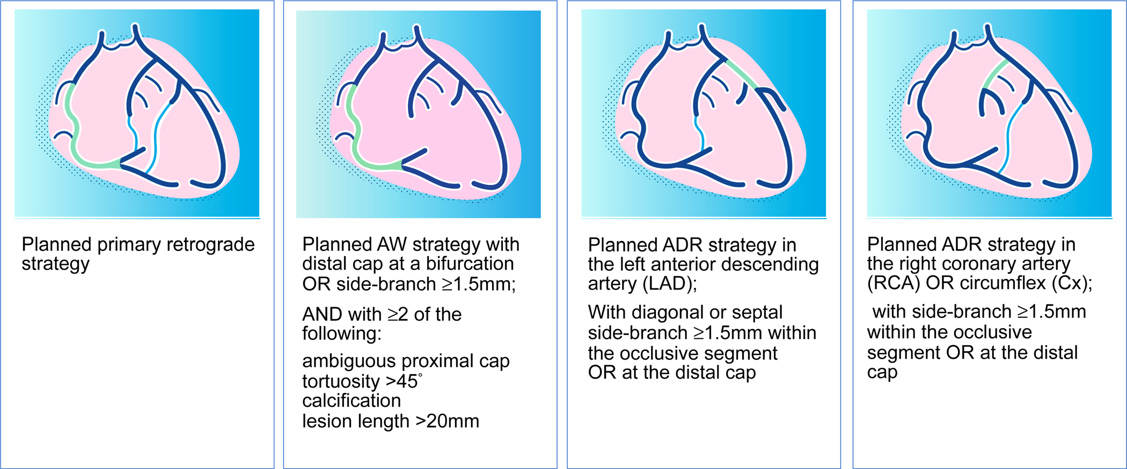
Figure 3: INVEST–CTO defined ‘High-Risk’ CTO Lesions
Courtesy of Anja Oksnes (slides presented at TCT 2025)
Results
Baseline characteristics revealed high prevalence of cardiovascular risk factors. Prior MI featured in the past history of 42 % and rates of hypertension, hypercholesterolaemia and diabetes were 69 %, 70 % and 28 % respectively. Prior PCI and prior CABG were present in 56 % and 27 % of patients respectively. Clinical presentation was stable CAD in approximately 93 %.
With respect to lesion characteristics, this was a truly ‘high-risk’ and complex cohort with median J-CTO Score 4 – angiographic and anatomical lesion characteristics are summarised in Figure 4.
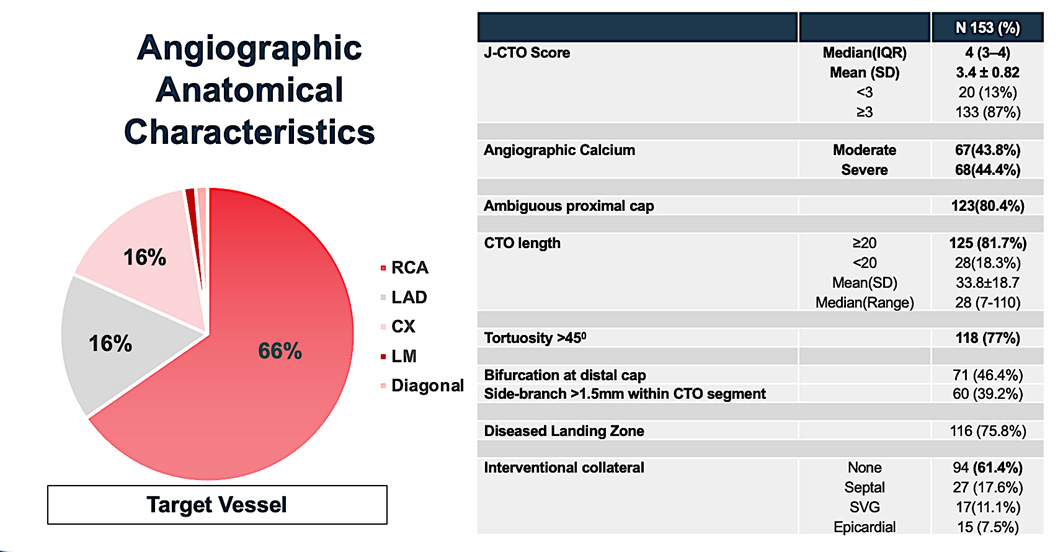
Figure 4: Angiographic and anatomical characteristics of high-risk CTO lesions
Courtesy of Anja Oksnes (slides presented at TCT 2025)
Both technical and procedural success was achieved in 86.7 % with no in-hospital MACE, meeting non-inferiority versus the 75 % benchmark. 30-day composite safety events (secondary endpoint) occurred in 7 patients (4.6 %). CCS angina ≥ 2 fell from 85 % at baseline to 60 % post-investment and 20 % post-completion (Figure 5).
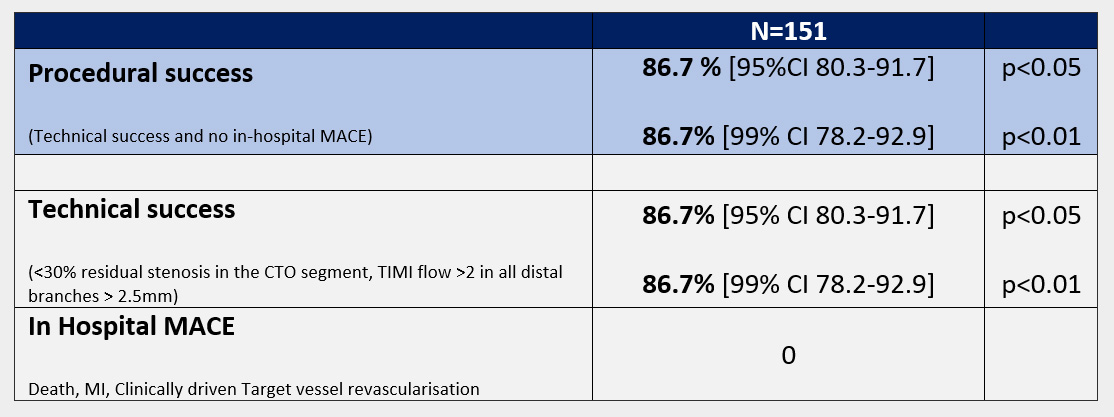
Figure 5: key results
Courtesy of Anja Oksnes (slides presented at TCT 2025)
Discussion
Study strengths, limitations and weaknesses are summarised in Table 1. Of note, this is the first study to assess the potential effects of a true up-front planned ‘investment’ procedure in CTO PCI. It is important to differentiate between the concept of ‘investment’ as described in the INVEST CTO study and that which is referred too following ‘STAR’ (sub-intimal tracking and re-entry).
In this study, the ‘investment’ procedure aimed to modify the CTO proximal and distal caps and lesion body from within the extraplaque space with balloon angioplasty. The purpose was to facilitate increased success of antegrade wiring as the primary crossing strategy and reduce procedural complexity at the completion stage procedure in a high-risk CTO cohort. There was no intent or attempt to re-enter the distal true lumen. A ‘STAR’ procedure, also a CTO modification technique and also traditionally referred to as an ‘investment’ is usually performed as a bailout following unsuccessful crossing and intentionally involves re-entry into the distal true lumen prior to extraplaque modification.
Recent data from the STAR study assessed utilisation of STAR for ‘bailout’ modification during index procedure to improve procedural success at staged completion7. An overall 6 % MACE rate was observed at the index, driven by perforation. In INVEST in-hospital MACE was 0 % at the index procedure despite higher mean JCTO score [3.4 versus 2.8]. These differences are perhaps likely to have been driven by the alternative strategies and intents for modification in the two studies. In the STAR Study, modification was utilised as bailout after attempt at procedural completion, whilst in the INVEST study the intent was upfront modification without an attempt to complete. This observation lends support to the safety of up-front modification, a primary objective of the study investigators.
That 13 % of cases wired successfully and went on to completion at the index procedure in INVEST, due to shorter than anticipated CTO length from the diagnostic angiogram [in the absence of dual injections] is reflective of both real-world practice and the skillset of the recruiting operators. The majority of CTO PCI procedures are undertaken electively following a standard set of diagnostic angiography views on which true CTO length cannot always be accurately assessed. Given that complication risk increases with complexity of procedural strategy, it is important to note the 50 % rate of final crossing/completion utilising AWE in INVEST, which is significantly higher than that seen in prior CTO registries (Figure 6).
Table 1 - Study strengths and limitations
Strengths | Limitations/Weaknesses |
First prospective study assessing feasibility, safety and potential outcome benefits of up-front ‘Investment’ procedure. | 55% of case recruitment from the Lead Centre undertaken by PI, and the remainder predominantly by highly experienced operators – limitation to external validity. |
Highly granular filtering for ‘high-risk’ lesions demonstrated by a median JCTO Score of 4 | Highly selectively defined ‘high-risk’ lesions anatomically – results cannot be directly extrapolated to lower risk/complexity lesions. |
90% IVUS use, with dedicated analysis of mechanistic effects of investment technique within Imaging Core lab – first of a kind for this method. | Modest overall sample size –but adequate given primarily a feasibility study. |
Independent adverse events adjudication by a dedicated CEC increasing credibility of outcome reporting. | 62% of procedures undertaken bi-radially – whilst this has a positive effect in reducing vascular complications and recovery time, it does not reflect standard practise for complex CTO PCI in North America [and other jurisdictions] – therefore not generalisable to these regions. |
Near 90% technical success rate in a highly complex lesion subset with NO in-hospital MACE and low [4.6%] 30-d MACE, supporting feasibility and safety. | Potential for bias in patient reported outcome measures given lack of comparator arm and no blinding to treatment strategy. However, reassuring to observe incremental improvement in angina symptom class was observed from pre-PCI to post – investment and from post – investment to post – completion procedure. |
![INVEST-CTO: Figure 6: Final crossing/completion strategy for JCTO 4 lesions subsets [approximate %]](https://www.pcronline.com/var/pcrov3/storage/images/media/pcr/news/2025/tct/invest-cto-fig-6-final-crossing-completion-strategy-fot-jcto-4-lesions-subsets/28021681-4-eng-GB/invest-cto-fig-6-final-crossing-completion-strategy-fot-jcto-4-lesions-subsets.jpg)
Figure 6: Final crossing/completion strategy for JCTO 4 lesions subsets [approximate %]
Designed by Papadopoulou S. and Mahadevan K.
Source: PCRonline.com
These preliminary results suggest that a strategy of a 2-staged approach in high-risk CTO’s has the potential to increase accessibility and safety of CTO PCI with the goal of reducing complication rates and improving patient experience. Whether, however, this translates to similar real-world outcomes, beyond the hands of expert CTO operators is both questionable and remains to be seen.
Without a head-to-head comparator, it is perhaps more challenging to appreciate the potential benefits pertaining to reduction in contrast load, procedural time, x-ray dose and procedural complication rates – a cohort matched analysis of a similarly high-risk CTO population from existing national/international registries would provide informative comparative insight.
The investigators should be congratulated on achieving the primary goal of demonstrating feasibility, safety and non-inferiority of a planned investment procedure, and setting the scene for a randomised trial assessing up-front ‘investment’ against ‘standard of care’ in the treatment of high-risk chronic occlusions.
Conclusion
A planned 2–stage investment and follow-on staged completion procedure was safe, effective and non-inferior to current techniques, and can be considered as an initial or early strategy in the treatment of high-risk CTO’s.
References
- Wilson WM, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016;102(18):1486–1493. doi: 10.1136/heartjnl-2015-308891.
- Tajti P, et al. The Hybrid Approach to Chronic Total Occlusion Percutaneous Coronary Intervention: Update From the PROGRESS CTO Registry. JACC Cardiovasc Interv. 2018;11(14):1325–1335. doi: 10.1016/j.jcin.2018.02.036.
- Sapontis J, et al. Early Procedural and Health Status Outcomes After Chronic Total Occlusion Angioplasty: A Report From the OPEN-CTO Registry. JACC Cardiovasc Interv. 2017;10(15):1523–1534. doi: 10.1016/j.jcin.2017.05.065.
- Simsek B, et al. Predicting Periprocedural Complications in Chronic Total Occlusion Percutaneous Coronary Intervention: The PROGRESS-CTO Complication Risk Scores. JACC Cardiovasc Interv. 2022;15(14):1413–1422. doi: 10.1016/j.jcin.2022.06.007.
- Xenogiannis I, et al. Outcomes of “Investment Procedures” in Chronic Total Occlusion Interventions. J Am Coll Cardiol. 2019;74(13 Suppl B):B228. doi: 10.1016/j.jacc.2019.08.293.
- Øksnes A, et al. Effectiveness, safety, and patient-reported outcomes of a planned investment procedure in higher-risk chronic total occlusion percutaneous coronary intervention: Rationale and design of the INVEST-CTO study. Catheter Cardiovasc Interv. 2023;102(1):71–79. doi: 10.1002/ccd.30692.
- Hirai T, Kearney K, Azzalini L et al. Optimal timing of staged percutaneous coronary intervention after subintimal tracking and re-entry: Rationale and design of the subintimal tracking and re-entry with deferred stenting study. Catheter Cardiovasc Interv. 2024 Sep;104(3):444-450
Authors





No comments yet!