Identification of vulnerable plaques and patients by intracoronary near-infrared spectroscopy and ultrasound (PROSPECT II)
Selected in The Lancet by T. Jones , M. Alasnag
This is the first prospective natural history study to evaluate the utility of comprehensive intravascular imaging with both IVUS and NIRS in predicting future adverse events following acute myocardial infarction.
References
Authors
David Erlinge, Akiko Maehara, Ori Ben-Yehuda, Hans Erik Bøtker, Maeng, Lars Kjøller-Hansen, Thomas Engstrøm, Mitsuaki Matsumura, Aaron Crowley, Ovidiu Dressler, Gary S Mintz, Ole Fröbert, Jonas Persson, Rune Wiseth, Alf Inge Larsen, Lisette Okkels Jensen, Jan Erik Nordrehaug, Øyvind Bleie, Elmir Omerovic, Claes Held, Stefan K James, Ziad A Ali, James E Muller, Gregg W Stone for the PROSPECT II Investigators
Reference
Volume 397, Issue 10278, 13–19 March 2021, Pages 985-995
Published
March 2021
Link
Read the abstractReviewers
Our Comment
Why this study? – the rationale/objective
This study aims to evaluate the ability of intravascular ultrasound (IVUS) and near-infrared spectroscopy (NIRS) to detect vulnerable plaques within the coronary arteries.
Prior studies have suggested that these individual modalities can identify vulnerable plaque1-3; however, this is the first prospective study to evaluate the utility of comprehensive intravascular imaging with both IVUS and NIRS in predicting future adverse events following acute myocardial infarction (MI).
It is important to further understand the high-risk features of coronary atherosclerosis to aid in prognostication for patients with coronary artery disease and implementation of secondary prevention measures.
Furthermore, this may facilitate plaque evaluation in the context of complete revascularization which is currently recommended for those with an MI (except shock).
How was it executed? – the methodology
This is a multicentric prospective study that evaluated 898 patients who had suffered an MI within the prior 4 weeks at 16 centers in Denmark, Norway, and Sweden.
Following physiologic guided revascularization of all non-culprit lesions (> 40%), a combination of IVUS and NIRS was performed on the proximal 6-10 cm of all three coronary arteries.
Maximum lipid core burden index within a 4 mm segment (max LCBI 4 mm), % plaque burden, and minimal luminal area (MLA) were hypothesized to predict major cardiac adverse events (MACE), defined as cardiac death, MI, unstable angina, or progressive angina. MACE events were reported up to a median follow-up of 3.7 years.
Notably, all patients were placed on guideline-directed medical therapy for coronary artery disease following MI.
What is the main result?
A total of 3,629 untreated non-culprit lesions in 898 patients were identified by IVUS and included in the analysis. Of these 3,629, NIRS data was available for 3,500.
At 4-year follow-up, a total of 112 (13.2%) of all patients experienced composite adverse events. Within this group, 84 events attributed to 78 unique untreated non-culprit lesions occurred in 66 patients (8%).
Patients with at least one untreated lesion with max LCBI 4 mm > 324.7, > 70% plaque burden, or MLA < 4.0 mm2 were significantly more likely to suffer an untreated non-culprit lesion-related event compared to those without these features.
Additionally, these high-risk plaque characteristics were predictive of events arising from each specific lesion (p < 0.0001 for all 3). The relation between presence of > 1 lipid-rich lesion with max LCBI 4 mm > 324.7 and rates of non-culprit lesion-related MACE was consistent between men and women (pinteraction = 0.31). In a multivariable model using all 3 high-risk features, high lipid content (maxLCBI4mm) and a large plaque burden remained independent predictors of non-culprit lesion-related MACE. However, in the multivariable model small MLA was no longer a significant correlate.
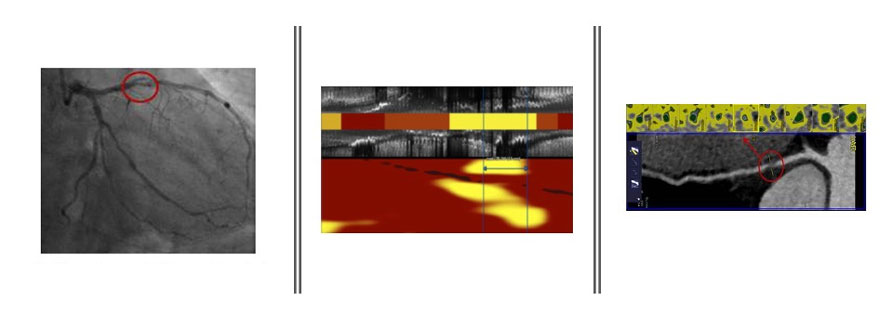
Cardiac CT and NIRS imaging illustrating plaque consistency in a culprit lesion
Critical reading and the relevance for clinical practice:
There were several important findings in this natural history study of non-culprit lesions following an MI.
First, most MACE events following MI within the 4-year follow-up period arose from mild lesions that were not hemodynamically significant at the time of the MI. This is in contrast to prior studies such as the original PROSPECT study and LRP study1-3 in which the proportion of MACE was similar in culprit and non-culprit lesions. The difference in observed event rates may be related to increasing use of intravascular imaging at the time of culprit vessel treatment, along with improving stent technology and medical therapy post-MI.
Nevertheless, a significant number of patients within this study experienced events related to a non-culprit lesion.
Next, a substantial number of patients presenting with an MI had intracoronary imaging findings consistent with high-risk features (24% of lesions exhibiting max LCBI 4 mm > 324.7, 22% of lesions exhibiting > 70% plaque burden, and 38% of lesions exhibiting MLA < 4.0 mm2).
This supports the theory that high-risk vulnerable plaques may be more often present in patients presenting with acute coronary syndromes as compared to chronic stable coronary artery disease, further confirming the concept of vulnerable patient and not just vulnerable plaque.
Finally, non-culprit lesion MACE rates were almost entirely related to lesions with high lipid content, large plaque burden, or small MLA despite most of these lesions being not hemodynamically or angiographically significant.
Notably, the relationship between high lipid content and the MACE rate was consistent among men and women in this study. This study confirms outcomes from prior studies suggesting that lipid content and plaque burden are valid prognostic tools for coronary events following an MI; however, MLA was not found to be predictive of future events in this study.
This has implications on secondary prevention whereby aggressive lipid modification with lifestyle and potentially PCSK9i may permit stabilization of the plaque. This also suggests that our focus should go beyond percent stenosis and MLA when determining which lesions to tackle during a complete revascularization strategy.
Overall, this study establishes the prognostic value of identifying high lipid content lesions with large plaque burden.
Equally important is the negative predictive value of low-risk plaques.
At present, clinical recommendations regarding guideline-directed medical therapy for coronary artery disease are unlikely to change as a result of these findings, as there is no evidence to suggest that intensified pharmacotherapy or focal intervention for vulnerable plaques changes outcomes.
Finally, it is unclear as to whether these findings could be extrapolated to patients with chronic stable coronary artery disease.
However, these results will aid in immediate prognostic value and may lay the foundation for future clinical trials to explore the remaining unanswered questions. One of these questions is the ability of other imaging modalities such as cardiac computed tomography to identify vulnerable plaque and its prognostic utility.
References:
- Stone GW, Maehara A, Lansky AL, de Bruyne B, et al. “A prospective natural-history study of coronary atherosclerosis.” N Engl J Med. 2011 Jan 20;364(3):226-35. Doi:10.1056/NEJMoa1002358. PMID: 21247313.
- Cheng JM, Garcia-Garcia HM, de Boer SPM, Kardys I, et al. “In vivo detection of high-risk coronary plaques by radiofrequency intravascular ultrasound and cardiovascular outcome: results of the ATHEROREMO-IVUS study.” Eur Heart J. 2014 Mar;35(10):639-47. doi: 10.1093/eurheartj/eht484. PMID:24255128.
- Waksman R, Di Mario C, Torguson R, Ali ZA, et al. “Identification of patients and plaques vulnerable to future coronary events with near-infrared spectroscopy intravascular ultrasound imaging: a prospective, cohort study.” Lancet. 2019 Nov 2;394(10209):1629-1637. doi: 10.1016/S0140-6736(19)31794-5. Epub 2019 Sep 27. PMID: 31570255.





No comments yet!