Initial findings from the North American COVID-19 Myocardial Infarction Registry
Selected in JACC by L. Biasco
This study aimed at assessing in-hospital outcomes of patients with confirmed COVID-19 and concomitant STEMI in a large dataset obtained from the Midwest STEMI Consortium.
References
Authors
Garcia S, Dehghani P, Grines C, Davidson L, Nayak KR, Saw J, Waksman R, Blair J, Akshay B, Garberich R, Schmidt C, Ly HQ, Sharkey S, Mercado N, Alfonso CE, Misumida N, Acharya D, Madan M, Hafiz AM, Javed N, Shavadia J, Stone J, Alraies MC, Htun W, Downey W, Bergmark BA, Ebinger J, Alyousef T, Khalili H, Hwang CW, Purow J, Llanos A, McGrath B, Tannenbaum M, Resar J, Bagur R, Cox-Alomar P, Stefanescu Schmidt AC, Cilia LA, Jaffer FA, Gharacholou M, Salinger M, Case B, Kabour A, Dai X, Elkhateeb O, Kobayashi T, Kim HH, Roumia M, Aguirre FV, Rade J, Chong AY, Hall HM, Amlani S, Bagherli A, Patel RAG, Wood DA, Welt FG, Giri J, Mahmud E, Henry TD; Society for Cardiac Angiography and Interventions, the Canadian Association of Interventional Cardiology, and the American College of Cardiology Interventional Council.
Reference
10.1016/j.jacc.2021.02.055
Published
April 2021
Link
Read the abstractReviewer
Latest contributions
TAVI complications - Part 5 Unusual structural interventions: infective endocarditis, ventricular septal rupture & hypertrophic obstructive cardiomyopathy Tendyne transcatheter mitral valve system in patients with severe mitral annular calcification: one-year outcomes from the SUMMIT Severe MAC cohortMy Comment
Why this study? – the rationale/objective
The aim of this study was to assess in-hospital outcomes of patients with confirmed COVID-19 and concomitant STEMI in a large dataset obtained from the Midwest STEMI Consortium, a large, multicentre, North American collaborative initiative including data derived from regional STEMI programmes (Iowa, Minnesota, Illinois and Ohio).
How was it executed? – the methodology
Prospective, investigator-initiated, observational registry with ongoing enrollment at more than 60 sites.
Analysis included patients enrolled between April and December 2020.
- Three categories of patients included:
- Confirmed COVID+: adults with clinical features compatible with STEMI (ECG and symptoms) and a positive COVID-19 test within 4 weeks prior to the index STEMI hospitalization.
- Suspected COVID+ (aka Person Under Investigation, PUI): adults with clinical features compatible with STEMI and suspected COVID-19 infection according to the treating physician (e.g. with symptoms compatible with COVID-19 infection or known exposure to a confirmed case), but with negative COVID-19 test.
- Controls: non COVID-19 age and sex matched historical controls (2:1 ratio) obtained from the Midwest STEMI Consortium. Controls selected among patients treated in a pre-pandemic period (between 2015 and 2019).
- Comparisons of clinical characteristics, treatments, and in-hospital outcomes among confirmed, suspected COVID-19 patients and controls.
- Primary endpoint set as the composite of in-hospital death, stroke, recurrent myocardial infarction, or unplanned revascularization.
What is the main result?
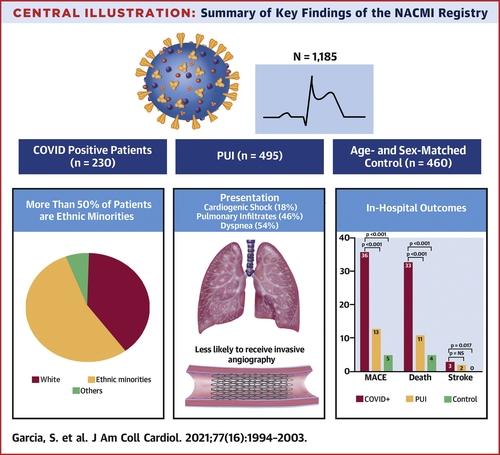
- Registry included 230 confirmed, 495 suspected COVID patients, and 460 controls.
- Sex and age were comparable among the three groups, while COVID+ patients were more likely to have minority ethnicity as compared to suspected cases (no data available for controls).
- Coronary angiography performed only in 78 % of confirmed COVID+ as compared to 96 % of suspected COVID and 100 % of matched controls.
- After angiography, 20 % of confirmed COVID-19 patients received medical management without reperfusion (probably due to the absence of occlusive coronary lesions) as compared to 11 % in suspected cases and 2 % in controls. When reperfusion was indicated, door-to-balloon time was longer in COVID+ patients as compared to non-COVID patients.
- A significant difference in the occurrence of the primary outcome was observed in COVID+ confirmed patients (36 %) as compared to suspected (13 %) and controls (5 %), driven by high rates of in-hospital mortality (33 %, 11 %, and 4 %, respectively).
- Stroke rate was 3 % in COVID confirmed cases vs 2 % in suspected cases and 0 % in controls.
Source: JACC
Critical reading and the relevance for clinical practice:
ST-elevation myocardial infarction in association with COVID-19 is an intriguing combination, as evidenced by the almost simultaneous publication of the present paper by Garcia et al. along with data collected from the Working Group of the Spanish Society of Cardiology in this issue of Eurointervention (Rodriguez Leor et al. EuroIntervention 2021;16:1426-1433. DOI: 10.4244/EIJ-D-20-00935). Both publications were correlated by an accompanying editorial, highlighting the topic relevance.
Both reports extend initial pieces of evidence derived from early reports published by Stefanini et al. in Circulation and Sharma et al. in the New England Journal of Medicine, describing small collectives of retrospectively enrolled case series from Northern Italy and New York City collected during the first pandemic wave.
What is clear so far is the deleterious prognostic impact of the concomitant presentation of STEMI and COVID-19 infection, with high in-hospital mortality rates (23 % in the Spanish registry, 33 % in the North American registry, 39 % in the early Italian data, and 72 % in NYC series) with a four- to fivefold increase in mortality, as compared to non-COVID-19 patients.
What still remains unclear is of what kind of disease we are talking about when referring to STEMI in COVID-19.
According to clinical practice, three different scenarios can be manifest in this setting:
- STEMI in a COVID-19 patient (but with no or mild symptoms),
- STEMI complicating a clinically relevant COVID infection,
- Clinical conditions mimicking STEMI with non-occlusive coronary lesions as a manifestation of COVID.
In the first two scenarios, the typical Type I myocardial infarction with evidence of an occlusive culprit coronary lesion might occur or complicate any form of SARS-CoV2 infection, with a clear adjunctive prognostic impact. The management of these patients is challenging due to the logistical issues related to patients’ and health care professionals' protection (that might result in delayed treatment times), along with optimal pharmacological measures needed to manage the boosted thrombogenicity observed in COVID-19 patients with acute coronary syndromes.
On the other hand, clearly different mechanisms are involved for patients with STEMI and non-occlusive coronary lesions, a frequently encountered condition that deserves focused research.
While we are far from a complete understanding of the cardiovascular implications of SARS-CoV2 infection, clinical practice and initial reports demonstrated that the latter group of patients, presenting with ST-segment elevation at ECG consistent with myocardial infarction with unobstructed coronary arteries at coronary angiography, are at an even higher risk of in-hospital mortality (as high as 90 % in NYC case series). Unfortunately, the present paper does not provide enough data regarding this intriguing and clinically relevant subgroup, while this category of patients seems to be under-represented in the paper by Rodriguez Leor et al., with only 2.6 % of their population with no coronary lesions evident at angiography.
Diffuse of endothelial activation causing microvascular thrombi, capillary vascular occlusion and ischemic damage has been demonstrated in the pulmonary vasculature of patients with COVID-19 by Ackermann et al. in an elegant autopsy study published in the New England Journal of Medicine. An analogous mechanism could be responsible for the “STEMI-like” presentation in COVID-19 patients. As demonstrated by Guagliumi et al. in a 43-year-old COVID-19 patient with typical inferior STEMI but without obstructive coronary disease. The only apparent abnormality evident at angiography were a TIMI 2 flow in the left anterior descending artery and persistent myocardial blush in distal right coronary artery. Diffuse microvascular thrombosis in the absence of epicardial coronary obstruction at post-mortem examination was observed.
Diagnosis of STEMI is one of the first learning points of every cardiology resident and its treatment relies on evidence-based and standardized protocols. These new pieces of evidence, while deserving additional focused research, show us how well-known clinical entities can conceal complex and yet unknown pathophysiological mechanisms.




No comments yet!