Mechanical thrombectomy with retrievable stents and aspiration catheters for acute ischaemic stroke: a meta-analysis of randomised controlled trials
Selected in EuroIntervention by A. N. Calik , L. Pay
The current meta-analysis highlights that mechanical thrombectomy with retrievable stents or aspiration catheters reduced disability and all-cause mortality at 90 days in acute anterior circulation ischaemic stroke.
References
Authors
Christopher A. Rajkumar, Sashiananthan Ganesananthan, Yousif Ahmad, Henry Seligman, George D. Thornton, Michael Foley, Alexandra N. Nowbar, James P. Howard, Darrel P. Francis, Thomas R. Keeble, Iris Q. Grunwald, Rasha K. Al-Lamee, Iqbal S. Malik, Matthew J. Shun-Shin
Reference
10.4244/EIJ-D-21-00343
Published
September 2021
Link
Read the abstractReviewers
Our Comment
Why this study? – the rationale/objective
The main purpose of treating patients with acute ischemic stroke is to maintain blood flow in the cerebral artery and reduce irreversible brain damage.
Even though intravenous tissue plasminogen activator (IV-tPA) within 4.5 hours of symptom onset is the first-line medical treatment of acute ischemic stroke, it may not provide complete revascularization in the majority of patients.
Today, removing the blockage with stent retrievers or aspiration catheters, in adjunct with IV-tPA where possible, has been the treatment of choice among patients having an acute ischemic stroke caused by a large-vessel occlusion.
The present meta-analysis aimed to compare the effect of mechanical thrombectomy with conventional medical therapy in patients with acute anterior ischemic stroke.
How was it executed? - the methodology
A search of PubMed was performed to evaluate all RCTs consisting of patients randomly assigned to thrombectomy (performed by either a retrievable stent or aspiration catheter) or control groups on a background of medical therapy, including intravenous thrombolysis when appropriate.
The primary efficacy endpoint was disability at 90 days which was evaluated by modified Rankin scale (mRS), where a score of 0 means no symptoms at all, and 6 means death. Besides, a dichotomised outcome from the mRS, which categorised an independent functional outcome (mRS ≤2) or a dependent outcome (mRS >2), was provided.
All-cause mortality at 90-day follow-up was defined as the secondary efficacy endpoint, whereas the safety endpoint was symptomatic intracranial haemorrhage. Analysis was performed with a Bayesian mixed-effects model.
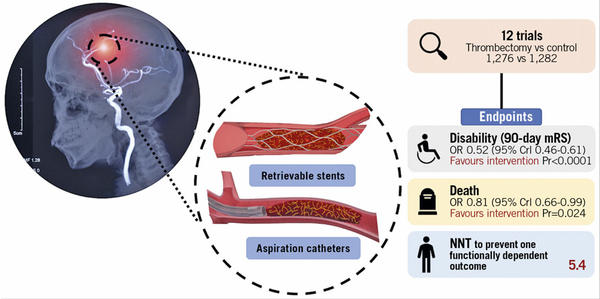
Source: EuroIntervention - Central illustration. Mechanical thrombectomy with retrievable stents and aspiration catheters for acute ischaemic stroke: a meta-analysis of randomised controlled trials.
What is the main result?
Overall, twelve trials published between 1 January 2010 to 2 July 2020 were included in the analysis. A total of 2,558 patients were randomized to thrombectomy (n = 1,276) and to control arm (n = 1,282). Intravenous thrombolysis was administered in both arms if indicated. In most studies, except DAWN and DEFUSE3, thrombectomy was performed in the first eight hours after symptom onset, with a median duration of 224-259 minutes.
The level of disability at 90 days, the primary efficacy endpoint, was reduced with thrombectomy compared to medical therapy alone (OR 0.52; 95 % credible interval [CrI] 0.46-0.61). The median mRS at follow-up was 3 in the thrombectomy group and 4 in the control group. Thrombectomy reduced the odds of patients being functionally dependent (mRS >2) at 90 days (OR 0.44, CrI 0.37 to 0.52, pr < 0.0001). For every 5.4 patients treated with thrombectomy, one fewer patient will be dependent at 90 days.
The rate of all-cause mortality, a secondary endpoint, was 16.1 % in patients randomized to thrombectomy and 19.2 % in those randomized to control (OR 0.81; 95 % credible interval [CrI] 0.66-0.99), a difference works out to a number needed to treat (NNT) of 32.
The frequency of symptomatic intracranial haemorrhage was similar in both groups (4.2 % vs 4.0 %).
Critical reading and the relevance for clinical practice
The current meta-analysis highlights that mechanical thrombectomy with retrievable stents or aspiration catheters reduced disability and all-cause mortality at 90 days in acute anterior circulation ischemic stroke.
Besides showing an improvement in the degree of disability assessed by mRS, this is the first meta-analysis demonstrating mortality benefit using modern mechanical thrombectomy. Of note, the benefit of mechanical thrombectomy was not mitigated even in the DAWN and DEFUSE3 trials, which included late-presenters compared to trials restricted to patients with an earlier presentation.
The current evidence suggests that this life-saving treatment needs to be expanded with more straightforward and more rapid access to 24/7 teams of proceduralists, CT vascular imaging and interpretation, catheter laboratory staff, and anaesthetists on-call for this intervention. Also, coordination between ambulance services, emergency departments, thrombectomy centres, and rehabilitation services should be optimized to save time while managing such critically ill patients.
References
- Frøbert O, Götberg M, Erlinge D, et al. Influenza Vaccination after Myocardial Infarction: A Randomized, Double-Blind, Placebo-Controlled, Multicenter Trial: IAMI trial. Circulation. 2021; Aug 30
- Collins SD. Excess mortality from causes other than influenza and pneumonia during influenza epidemic. Public Health Rep. 1932;47:2159–2179
- Ciszewski A, Bilinska ZT, Brydak LB, et al. Influenza vaccination in secondary prevention from coronary ischaemic events in coronary artery disease: FLUCAD study. Eur Heart J. 2008;29:1350–1358.
- Phrommintikul A, Kuanprasert S, Wongcharoen W, et al. Influenza vaccination reduces cardiovascular events in patients with acute coronary syndrome. Eur Heart J. 2011;32:1730–1735.
- Gurfinkel EP, de la Fuente RL, Mendiz O, Mautner B. Influenza vaccine pilot study in acute coronary syndromes and planned percutaneous coronary interventions: the FLU Vaccination Acute Coronary Syndromes (FLUVACS) Study. Circulation. 2002 May 7;105(18):2143-7.
- Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–477.
- Davis MM, Taubert K, Benin AL, et al. Influenza vaccination as secondary prevention for cardiovascular disease: a science advisory from the American Heart Association/American College of Cardiology. J Am Coll Cardiol.2006;48:1498–1502.
- Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, Katz K, Ko DT, McGeer AJ, McNally D, et al. Acute Myocardial Infarction after Laboratory-Confirmed Influenza Vaccination. N Engl J Med. 2018; 378: 345-353.
- Atoui R, F FE, Sroka K, Mireau J, McElhaney JE, Hare G. Influenza Vaccination Blunts the Inflammatory Response in Patients Undergoing Cardiopulmonary Bypass. Ann Thorac Surg. 2020
- Bermudez-Fajardo A, Oviedo-Orta E. Influenza vaccination promotes stable atherosclerotic plaques in apoE knockout mice. Atherosclerosis. 2011; 217: 97-105






No comments yet!