Mortality 10 years after percutaneous or surgical revascularization in patients with total coronary artery occlusions
Selected in JACC by A. Candreva , S. Brugaletta
The proposed manuscript is an intriguing sub-analysis from the recent SYNTAX Extended Survival (SYNTAXES) study, where the Synergy Between PCI With Taxus and Cardiac Surgery (SYNTAX) was investigated.
References
Authors
Hideyuki Kawashima, Kuniaki Takahashi, Masafumi Ono, Hironori Hara, Rutao Wang, Chao Gao, Faisal Sharif, Michael J Mack, David R Holmes, Marie-Claude Morice, Stuart J Head, Arie Pieter Kappetein, Daniel J F M Thuijs, Milan Milojevic, Thilo Noack, Friedrich-Wilhelm Mohr, Piroze M Davierwala, Patrick W Serruys, Yoshinobu Onuma, SYNTAX Extended Survival Investigators
Reference
J Am Coll Cardiol. 2021 Feb 9;77(5):529-540
Published
February 2021
Link
Read the abstractReviewers
Our Comment
Why this study? – the rationale/objective
Intervention in coronary chronic total occlusions (CTOs) has increased in frequency as well in success rate worldwide. However, long-term clinical outcomes of patients with 3-vessel disease (3VD) and/or left main disease (LM) undergoing surgical revascularization or interventional recanalization of a CTO (i.e. CTO-PCI) is still uncertain. Similarly, the role played by the different CTO vessels targeted during the intervention has not yet been clarified.
How was it executed? – the methodology
The proposed manuscript is an intriguing sub-analysis from the recent SYNTAX Extended Survival (SYNTAXES) study, where the Synergy Between PCI With Taxus and Cardiac Surgery (SYNTAX) was investigated in a 1:1 randomized, two-arm fashion (PCI vs CABG) in terms of all-cause mortality at 10 years in 1’800 patients with 3VD and/or LM-disease. It included only the 460 recruited patients presenting at least one “total occlusion”, defined angiographically by the absolute absence of post-stenotic flow (TIMI flow grade 0), independently from the presence of collaterals or the age of the occlusion (≤ or > 3 months).
What is the main result?
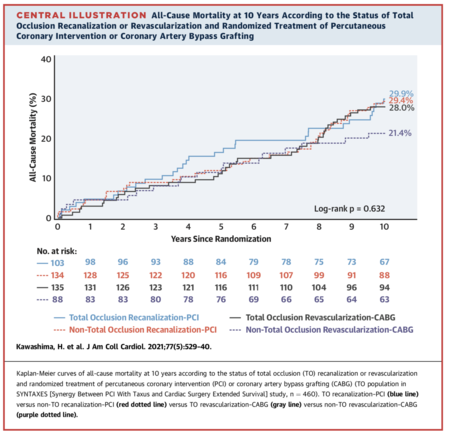
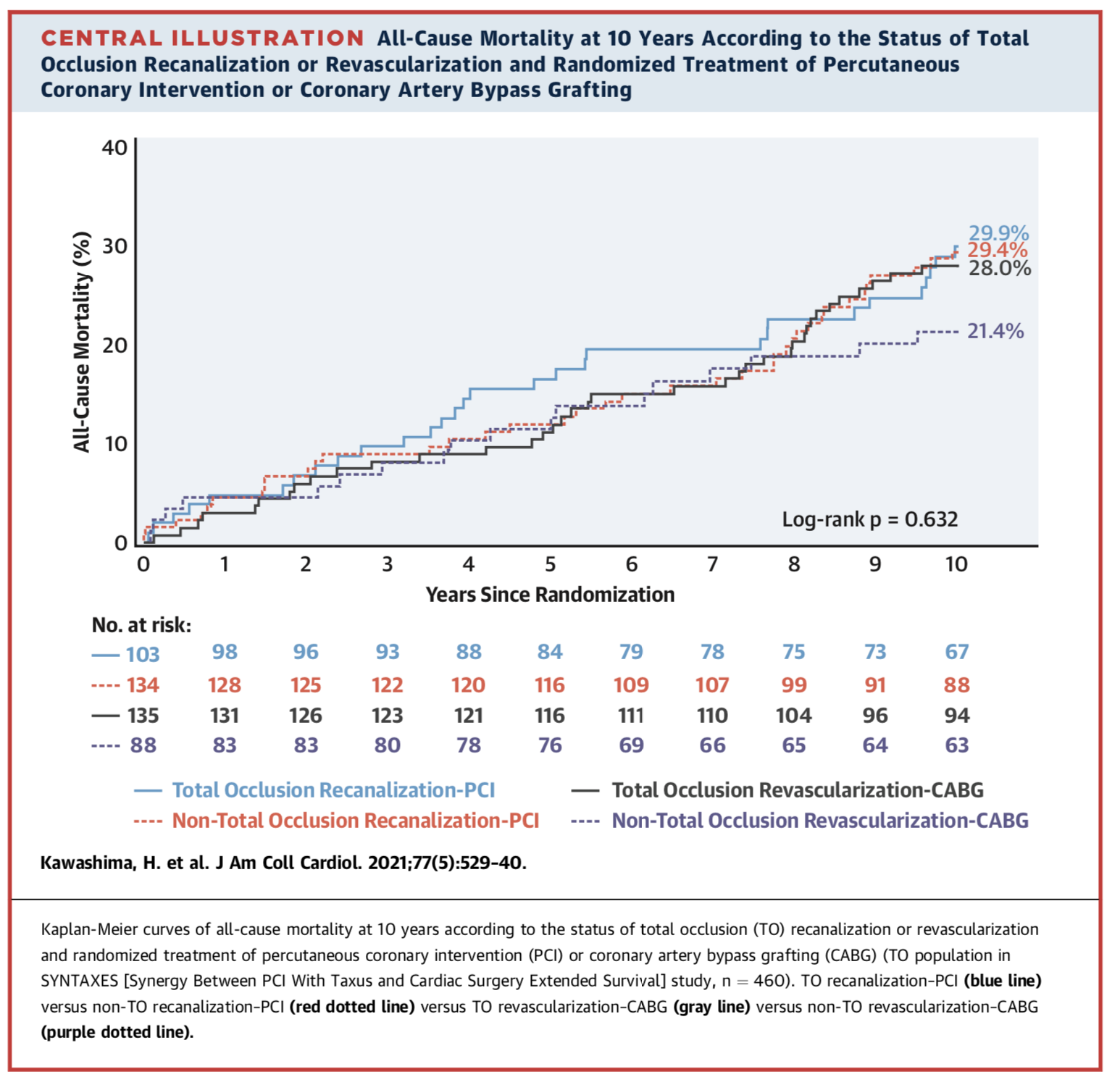
This study proposed many interesting results. Firstly, considering the whole recruited study population, the presence of an occluded vessel did not significantly impact on the 10-year mortality, which was 27.6% for patients with CTO vs. 26.1% in patients without CTO (adjusted HR: 1.018; 95% CI: 0.810 to 1.280; p = 0.877). Secondly, while complete successful revascularization was more often achieved with surgery (PCI: 43.5% vs. ACBP: 60.5%, p < 0.001), no significant survival benefit at 10 years was seen when comparing successful versus non-successful treatment (PCI arm: 29.9% vs. 29.4%; adjusted HR: 0.992; 95% CI: 0.474 to 2.075; p = 0.982; and CABG arm: 28.0% vs. 21.4%; adjusted HR: 0.656; 95% CI: 0.281 to 1.533; p = 0.330).
This was also true at the vessel-level analysis, where the success of an intervention on LM-CTO and/or left anterior descending artery (LAD)-CTO failed to impact on the 10-year all-cause mortality (adjusted HR: 0.896; 95% CI: 0.314 to 2.555; p = 0.837). On the contrary, treated CTO patients showed improved anginal control – quantified by the Seattle Angina Questionnaire (SAQ) – independently from treatment option, jumping from 18.6% freedom from angina rate at the baseline to 70.3% at 5 years.
Finally, a residual SYNTAX score above 8 (CTO: 45.5%; and non-CTO: 54.7%) predicted mortality independently of the CTO-status (CTO adjusted HR: 1.683; 95% CI: 1.01-2.8, p = 0.045; and non-CTO adjusted HR: 4.1; 95% CI: 2.5-6.6, p < 0.001).
Source: Journal of the American College of Cardiology (JACC)
Critical reading and the relevance for clinical practice:
This post hoc analysis from the SYNTAXES showed how CTOs are frequently encountered in an “all-comers” CAD population with 3VD or LM-disease (ca. one fourth of the enrolled trial population) and how treatment options - irrespectively of their success – failed to significantly impact survival at 10 years.
Patients treated with surgery of CTO-PCI showed improved anginal control both in the short and in the long terms. However, this does not translate into an improvement in survival: in this regard, the authors pointed at the “indiscriminate” CTO selection (i.e. not taking information on myocardial viability into account) as a study limitation which could have hampered the (expected) survival benefit of a CTO intervention.
Indeed, possibly in some contrast with the main analysis of this study, the sub-analysis on the residual SYNTAX score suggested that any intervention leading to a residual SYNTAX score below 8 could be associated with a survival benefit.
Finally, the authors reflect on the current practice of high-volume CTO-PCI centers to prioritize interventional solutions before surgical ones, which would be justified by current data showing no survival benefit from either treatment option. Moreover, the study results referred to CTO intervention performed between 2005 and 2007, thus possibly diverging from the long-term outcomes of contemporary CTO-PCI procedures, whose recanalization technique is somehow different and probably more effective.
In conclusion, this study, while offering real-world, long-term clinical results of differential CTO treatments (PCI, CABG or non-intervention) in a large population, triggers further reflections on the actual clinical outcomes of modern, viability-guided CTO interventions.






No comments yet!