
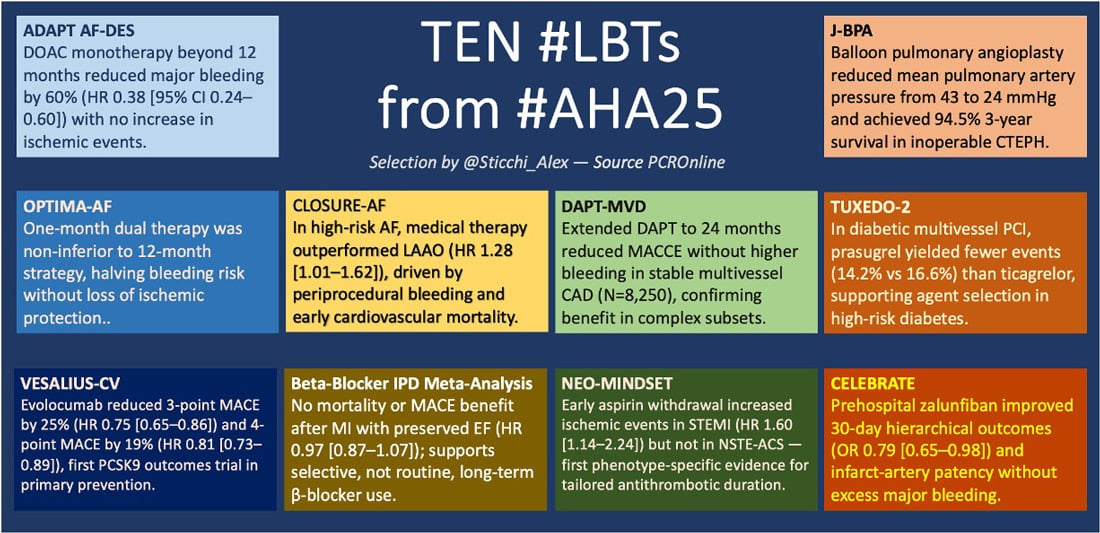
Ten trials from AHA 2025
Top 10 trials presented at the American Heart Association Scientific Sessions 2025
Alessandro Sticchi provides us with a curated overview of the late-breaking trials he found most relevant for interventional cardiologists from AHA 2025.
Why this study?
To determine whether DOAC monotherapy beyond 12 months after PCI is as effective and safer than continued combination therapy with clopidogrel in AF patients.
Methods
Multicenter, open-label, randomised, non-inferiority trial conducted in 32 Korean centers; N = 960 (mean age 71 years; 21 % women). AF and stable CAD ≥ 1 year post-DES. NOAC monotherapy vs NOAC + clopidogrel.
Key findings
The primary composite of death, MI, stent thrombosis, stroke, systemic embolism, or major/CRNM bleeding occurred in 9.6 % with DOAC monotherapy versus 17.2 % with dual therapy (absolute difference -7.6 %, P < 0.001). Major or clinically relevant bleeding was 5.2 % versus 13.2 % (HR 0.38 [95 % CI 0.24–0.60]), confirming both non-inferiority and superiority. There were no differences in ischemic events, though all-cause mortality was numerically higher with dual therapy (4.0 % vs 2.9 %).
Critical thinking
This trial reinforces a decade-long evolution from triple to dual and now single antithrombotic therapy in AF-PCI. Together with AUGUSTUS and ENTRUST-AF, it closes the loop on the safety of DOAC monotherapy beyond 1 year.
The findings align with European consensus for discontinuing antiplatelet agents in stable stents, confirming that ischemic benefit plateaus while bleeding risk persists. Future work should focus on defining which subgroups, complex PCI or high CHA₂DS₂-VASc, might still benefit from prolonged dual therapy.
Reference: Kim J-S et al. Therapy for atrial fibrillation in patients with drug-eluting stents. N Engl J Med. 2025; Epub ahead of print.
Why this study?
To test if 1 month of dual therapy (DOAC + P2Y12) followed by DOAC alone is as effective as 12 months dual therapy after PCI in AF.
Methods
Japanese RCT enrolling ≈ 1,000 AF-PCI patients. Randomised to 1-month vs 12-month dual therapy with follow-up at 12 months.
Key findings
Non-inferiority for ischemic events was achieved at 12 months with a hazard ratio close to unity; major bleeding was reduced by approximately 50 % with the shorter course.
Critical thinking
OPTIMA-AF complements prior studies such as STOPDAPT-2 and MASTER DAPT by extending the "minimalist" concept to AF-PCI. It validates that early aspirin discontinuation and short dual therapy can halve bleeding without compromising safety.
The results emphasise regional nuances — East Asian bleeding sensitivity and meticulous procedural technique — and should stimulate global validation across more heterogeneous cohorts. It advances the paradigm of precision-duration therapy rather than fixed-duration treatment.
Reference: Sotomi Y et al. presented at the American Heart Association Scientific Sessions 2025, New Orleans.
Why this study?
To evaluate whether early aspirin withdrawal with potent P2Y12 monotherapy differs in effect between STEMI and NSTE-ACS.
Methods
Pre-specified sub-study of the NEO-MINDSET trial. 3,410 ACS patients randomised to potent P2Y12 monotherapy (ticagrelor or prasugrel) or standard DAPT for 12 months.
Key findings
Among 2,119 STEMI and 1,291 NSTE-ACS patients, monotherapy increased ischemic events in STEMI (8.2 % vs 5.2 %, HR 1.60 [95 % CI 1.14–2.24]) but not in NSTE-ACS (5.1 % vs 6.0 %, HR 0.84 [0.39–2.02]; P interaction = 0.03). Bleeding decreased in both groups (STEMI HR 0.37 [0.22–0.61]; NSTE-ACS HR 0.45 [0.23–0.86]).
Critical thinking
The signal divergence between STEMI and NSTE-ACS challenges the universal adoption of aspirin-free strategies. It underlines that pathophysiology matters: higher thrombotic burden and microvascular obstruction in STEMI require more sustained platelet inhibition.
These data invite caution against blanket de-escalation policies and favor a tailored approach integrating clinical presentation, plaque morphology, and procedural complexity. NEO-MINDSET adds a new layer of phenotype-driven therapy to the ongoing de-escalation narrative.
Reference: Tavares CAM et al. J Am Coll Cardiol. 2025; Published online November 9, 2025. doi:10.1016/j.jacc.2025.10.058.
Why this study?
To compare LAAO with standard medical therapy in very high-risk AF patients.
Methods
German multicenter RCT, N = 912 (median age 79 years; CHA2DS2-VASc 5.2; HAS-BLED 3.0). LAAO (Amulet/Watchman FLX) vs standard care (mostly DOAC). Median follow-up 3 years.
Key findings
Primary endpoint (stroke/systemic embolism/CV or unexplained death/major bleeding): 16.8 vs 13.3 per 100 pt-years (HR 1.28 [95 % CI 1.01–1.62], P = 0.04), favoring medical therapy. Periprocedural bleeding contributed substantially to early events.
Critical thinking
CLOSURE-AF tempers enthusiasm for LAAO in very high-risk patients by revealing the limits of procedural benefit when frailty and comorbidities dominate prognosis. It also highlights the impact of operator learning curves and device evolution.
The results do not negate LAAO's value but reposition it as a solution for absolute anticoagulation intolerance, not for broad stroke prevention. Future generations of devices and lower-risk populations (as explored in CHAMPION-AF, CATALYST) may restore equipoise.
Reference: Landmesser U et al. Presented at AHA 2025; reported in TCTMD, Nov 9, 2025.
Why this study?
To determine if PCSK9 inhibition reduces events in high-risk patients without prior ischemic events.
Methods
Double-blind RCT, N = 12,257; median follow-up 4.6 years. Evolocumab 140 mg every 2 weeks vs placebo on optimised therapy.
Key findings
3-point MACE HR 0.75 [95 % CI 0.65–0.86]; 4-point MACE HR 0.81 [0.73–0.89]; LDL-C reduced by 55 % to 45 mg/dL. Benefit consistent across subgroups, with absolute risk reduction of 1.8 % and 2.8 % respectively.
Critical thinking
VESALIUS-CV moves PCSK9 inhibition upstream, from secondary prevention to high-risk primary prevention. It confirms that the biology of atherosclerosis progression is continuous, not binary. The trial substantiates the "lower is better" paradigm for LDL cholesterol, supporting guideline aspirations toward 40–50 mg/dL targets. It also exposes the challenge of translating statistical benefit into public health impact given drug cost and adherence barriers—issues that now define the next frontier of lipid management.
Reference: N Engl J Med. doi:10.1056/NEJMoa2514428.
Why this study?
To reassess the benefit of long-term β-blockade after MI in patients with LVEF ≥ 50 %.
Methods
Individual-patient meta-analysis pooling five RCTs (REBOOT, REDUCE-AMI, BETAMI, DANBLOCK, CAPITAL-RCT); N = 17,801; median follow-up 3.6 years.
Key findings
Primary endpoint (death/MI/HF): 8.1 % vs 8.3 % (HR 0.97 [95 % CI 0.87–1.07], P = 0.54). No benefit across age, sex, or index-MI type.
Critical thinking
This meta-analysis closes a 40-year debate originating from the pre-reperfusion era. In the context of early PCI, statins, and ACE inhibitors, β-blockers lose their prognostic edge when EF is preserved. The data advocate for selective use guided by symptoms, rhythm control, or ischemic burden rather than reflex prescription. The implications are broad: stewardship of therapy duration and de-prescription emerge as essential aspects of modern cardiology practice.
Reference: N Engl J Med. 2025; DOI:10.1056/NEJMoa2512686.
Why this study?
To evaluate the risk–benefit of extending DAPT for 12 additional months after DES in stable MVD.
Methods
Randomised, open-label multicenter study across 97 Chinese centers; N = 8,250 stable MVD patients event-free 12 months post-PCI.
Key findings
Extended DAPT reduced MACCE without increasing major bleeding.
Key takeaway: ischemic advantage maintained with no excess hemorrhage.
Critical thinking
The results revive discussion on the ischemic–bleeding trade-off in long-term secondary prevention. While DAPT-MVD shows net benefit in complex anatomy, it remains geographically limited to an East Asian population with distinct pharmacogenomics.
Integration with DAPT and PEGASUS-TIMI 54 frameworks suggests that optimal duration may depend more on plaque phenotype and systemic inflammation than on time alone. Precision extension, rather than blanket prolongation, should guide future strategies.
Reference: Tian J et al. Presented at AHA 2025, Late-Breaking Science LBS.06.
Why this study?
To assess if early subcutaneous GP IIb/IIIa inhibition improves reperfusion and outcomes in STEMI.
Methods
Phase 3 international double-blind RCT; N = 2,467 (58 sites). Zalunfiban 0.11 mg/kg or 0.13 mg/kg vs placebo at first medical contact.
Key findings
Hierarchical composite (death, stroke, MI, stent thrombosis, HF, large MI): OR 0.79 [95 % CI 0.65–0.98], P = 0.028. Severe bleeding 1.2 % vs 0.8 % (P = 0.40); mild/moderate bleeding 6.4 % vs 2.5 % (P < 0.001).
Critical thinking
CELEBRATE marks the return of prehospital pharmacology with a modern molecule designed for controllability and safety. By improving early microvascular reperfusion, it rekindles the concept once pioneered by glycoprotein IIb/IIIa inhibitors in the 1990s but abandoned for bleeding. Zalunfiban's short half-life and subcutaneous delivery redefine feasibility for early STEMI care, particularly in regions with long transfer delays. It positions pharmacologic reperfusion as a bridge to mechanical reperfusion, not a competitor.
Reference: van't Hof AWJ et al. NEJM Evidence. 2025; DOI:10.1056/EVIDoa2500268.
Why this study?
To compare prasugrel and ticagrelor in diabetic patients with MVD undergoing PCI.
Methods
Multicenter Indian RCT; N = 1,800; median age 60 years, 29 % women; 79 % ACS; 85 % triple-vessel disease.
Key findings
Composite death/MI/stroke/bleeding: 14.2 % prasugrel vs 16.6 % ticagrelor. Death 3.7 % vs 5.0 %; MI 5.2 % vs 6.0 %; major bleeding 7.1 % vs 8.4 %.
Critical thinking
TUXEDO-2 reopens the debate on agent selection in diabetes, the archetype of high-platelet-reactivity states. Contrary to expectations from ISAR-REACT 5, the signal favoring prasugrel suggests that ticagrelor's reversible binding and dyspnea-related discontinuation may compromise efficacy in diabetics.
These results advocate individualized P2Y₁₂ choice based on metabolic profile, adherence, and tolerance, advancing the concept of precision pharmacotherapy in coronary intervention.
Reference: Bangalore S et al. ACC.org, Nov 10, 2025.
Why this study?
To assess safety and efficacy of BPA as an alternative to pulmonary endarterectomy in inoperable CTEPH.
Methods
Multicenter Japanese registry; N = 308 patients; 1,408 BPA procedures.
Key findings
Mean PAP fell from 43 to 24 mmHg after BPA, maintained at 22.5 mmHg at follow-up. Complications 36 % (17.8 % pulmonary injury, 14 % hemoptysis). Three-year survival 94.5 %.
Critical thinking
J-BPA demonstrates that interventional treatment of pulmonary hypertension has matured from experimental to reproducible therapy. With procedural safety improving and outcomes approaching those of surgical endarterectomy, balloon pulmonary angioplasty is poised to redefine care for inoperable CTEPH.
The Japanese multicenter experience underscores the role of specialised centers and structured training, setting a benchmark for global adoption as expertise disseminates.
Reference: Ogawa A et al. Circ Cardiovasc Qual Outcomes. 2017;10:e004029.
Final thoughts
The ten late-breaking trials presented at AHA 2025 collectively illustrate a cardiology that is no longer guided by dogma but by refinement, a shift from "more treatment" to "smarter treatment."
In the antithrombotic arena, ADAPT AF-DES and OPTIMA-AF consolidate the final step of a 15-year journey from triple to monotherapy, cementing the safety of de-escalation strategies. NEO-MINDSET then adds nuance, proving that de-escalation cannot be universal: phenotype matters, and STEMI is not NSTE-ACS.
CLOSURE-AF challenges the overextension of device-based stroke prevention, reminding us that procedural sophistication cannot compensate for biologic frailty. About prevention, VESALIUS-CV extends the benefit of PCSK9 inhibition into the high-risk primary-prevention field, reinforcing the "lower is better" principle while raising legitimate questions on accessibility and cost-effectiveness. The Beta-Blocker IPD Meta-Analysis reframes cardiology's culture of inertia, showing that deprescription can be as evidence-based as prescription.
Within coronary intervention, DAPT-MVD and TUXEDO-2 emphasise that not all patients fit the same template. Precision in DAPT duration and agent selection is emerging as the natural evolution of a maturing discipline. CELEBRATE, meanwhile, revives the forgotten power of pharmacologic reperfusion in the prehospital STEMI phase, but with 21st-century safety and pharmacokinetics.Finally, J-BPA projects interventional expertise beyond the heart, exemplifying how procedural innovation can transform previously neglected fields like CTEPH into structured, evidence-based therapies.
AHA 2025, therefore, will not be remembered for a single disruptive trial, but for a collective narrative: cardiology moving toward precision without excess, innovation with restraint, and evidence with humanity.
References
- Kim J-S et al. Therapy for atrial fibrillation in patients with drug-eluting stents. N Engl J Med. 2025.
- Sotomi Y et al. OPTIMA-AF trial. Presented at AHA 2025, New Orleans.
- Tavares CAM et al. J Am Coll Cardiol. 2025; Published online Nov 9. doi:10.1016/j.jacc.2025.10.058
- Landmesser U et al. CLOSURE-AF trial. Presented at AHA 2025; reported in TCTMD, Nov 9, 2025.
- N Engl J Med. 2025; doi:10.1056/NEJMoa2514428.
- Beta-Blocker Therapy After MI with Preserved EF. N Engl J Med. 2025; DOI:10.1056/NEJMoa2512686.
- Tian J et al. DAPT-MVD. Presented at AHA 2025, Late-Breaking Science LBS.06.
- van't Hof AWJ et al. NEJM Evidence. 2025; DOI:10.1056/EVIDoa2500268.
- Bangalore S et al. TUXEDO-2. ACC.org, Nov 10, 2025.
- Ogawa A et al. Circ Cardiovasc Qual Outcomes. 2017;10:e004029.







No comments yet!