29 Oct 2021
Placebo-controlled efficacy of percutaneous coronary intervention for focal and diffuse patterns of stable coronary artery disease
Selected in Circulation Cardiovascular Interventions by M. Pighi , S. Fezzi
According to the updated international revascularization guidelines, fractional flow reserve (FFR) and instantaneous wave-free period ratio (iFR) are proposed to dichotomize decision-making for ischemia detection in guiding percutaneous coronary intervention (PCI) of intermediate coronary stenosis.
References
Authors
Christopher A. Rajkumar; Matthew Shun-Shin; Henry Seligman; Yousif Ahmad; Takayuki Warisawa; Christopher M. Cook; James P. Howard; Sashiananthan Ganesananthan; Laura Amarin; Caitlin Khan; Ayesha Ahmed; Alexandra Nowbar; Michael Foley; Ravi Assomull; Niall G. Keenan; Joban Sehmi; Thomas R. Keeble; John R. Davies; Kare H. Tang; Robert Gerber; Graham Cole; Peter O’Kane; Andrew S.P. Sharp; Ramzi Khamis; Gajen Kanaganayagam; Ricardo Petraco; Neil Ruparelia; Iqbal S. Malik; Sukhjinder Nijjer; Sayan Sen; Darrel P. Francis; Rasha Al-Lamee.
Reference
10.1161/CIRCINTERVENTIONS.120.009891
Published
August 2021
Link
Read the abstractReviewers
Our Comment
Why this study? – the rationale/objective
According to the updated international revascularization guidelines, fractional flow reserve (FFR) and instantaneous wave-free period ratio (iFR) are proposed to dichotomize decision-making for ischemia detection in guiding percutaneous coronary intervention (PCI) of intermediate coronary stenosis.
Retrospective studies have outlined how the physiological pattern of CAD impacts both the physiological assessment and indices discordance, as well as on the best management of CAD. Indeed, on the one side, PCI seems to be effective in improving myocardial ischemia and clinical outcomes in case of focal stenosis. Conversely, in the presence of a diffuse pattern, the benefit is less clear, leading to suboptimal results, higher number and length of stent used, with the risk for side branch occlusion.
The ORBITA trial (Objective Randomised Blinded Investigation With Optimal Medical Therapy of Angioplasty in Stable Angina) was the first placebo-controlled trial investigating PCI for stable CAD. It showed that PCI was effective in normalizing the anatomic and hemodynamic features of coronary stenoses, compared with placebo. However, the effect sizes on exercise time and symptoms were smaller than expected, regardless of FFR/iFR values.
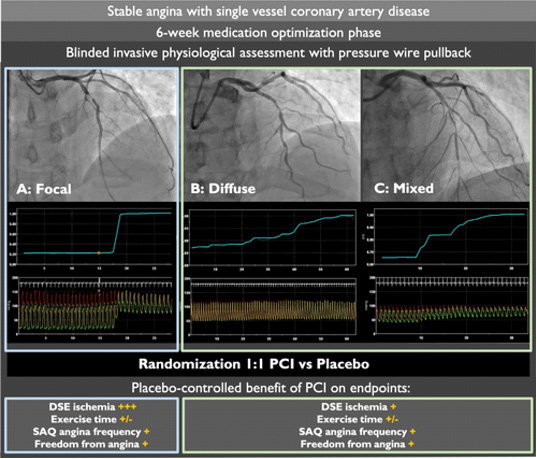
The objective of the current analysis was to assess whether the physiological pattern of CAD (focal vs. diffuse/combined) had an impact on the primary and secondary endpoints of the ORBITA trial, thus on the difference in exercise time increment from baseline to 6 weeks follow-up, on angina severity and on the improvement of stress echocardiography between PCI and placebo arms.
How was it executed? - the methodology
- This is a post-hoc analysis of the double-blind, multi-centre, 1:1 randomized, placebo-controlled ORBITA trial that included 230 patients with chronic ischaemic symptoms (200 randomized).
- Patients presented severe (≥ 70 %) single-vessel stenoses and, after enrolment, underwent six weeks of medical optimization. Patients then had pre-randomization assessments with cardiopulmonary exercise testing, symptom questionnaires, and dobutamine stress echocardiography.
- During the index procedure, patients were in deep conscious sedation and on auditory isolation.
- According to the study protocol, all the lesions were assessed with a pressure guide-wire detecting FFR, iFR, and iFR manual pullback values. The primary operator was blinded to their results, which definitely were not used to guide the intervention in the PCI arm.
- In the PCI arm, iFR and FFR were remeasured after revascularization with the operator that was blinded to the results.
- The physiological pattern of disease was defined as focal with ≥ 0.03 iFR unit drop within 15 mm and diffuse/mixed in the remaining cases. The analysis was conducted blindly by 6 experienced interventionalists.
- Among the overall population (200 patients), 164 patients were eligible for the current analysis as iFR pullback was not available at every site, and 4 patients were excluded due to technical procedural issues.
- In the PCI arm (n = 85), 48 patients (56 %) were classified as focal, 37 (44 %) as diffuse. In the placebo arm (n = 79), 35 patients (44 %) were focal and 44 (56 %) diffuse.
- Focal stenoses were associated with lower pre-randomization FFR (0.60 ± 0.15 vs 0.78 ± 0.10; p < 0.0001) and iFR (0.65 ± 0.24 vs 0.88 ± 0.08; p < 0.0001) values compared to diffuse disease.
Source: Circulation: Cardiovascular Interventions
What is the main result?
- In the overall population, PCI resulted in a larger improvement in stress echocardiography documented ischemia in comparison to a placebo procedure, OR 3.44 (95 % CI, 1.83–6.47, P < 0.0001). After adjustment, PCI for focal stenoses offered a significantly greater reduction in stress echo ischemia than PCI for diffuse disease. This effect was consistent when adjusted for baseline iFR (P = 0.020) or baseline FFR (P = 0.032) values.
- PCI did not significantly increase exercise time (9.32 seconds; 95 % CI, -17.1 to 35.7 seconds; P = 0.487) compared to placebo. For this relatively small effect, there was no detectable evidence of interaction between a focal disease pattern and the effect of PCI.
- PCI significantly improved SAQ angina frequency score (OR 1.88 [95 % CI, 1.05–3.37]; P = 0.034) and patient-reported freedom from angina (OR 2.90 [95 % CI, 1.42–5.92]; P = 0.0035) over a placebo procedure. However, there was no statistically significant evidence of interaction between a focal disease pattern and the effect of PCI.
- Using QCA-defined pattern of disease as a comparator, PCI did not even show a significant impact on stress echo score, as well as angina scores and exercise time.
Critical reading and the relevance for clinical practice
This report represents, besides with some limitations, the first placebo-controlled experience to assess the efficacy of PCI stratified by the iFR scout pullback defined physiological pattern of CAD. PCI showed to significantly improve stress echocardiography derived ischemia compared to placebo, in a greater way for focal stenoses compared to diffuse/combined pattern. No significant impact of the physiological pattern was reported on exercise time as well angina scores.
In the ORBITA trial, a significant interaction was detected between PCI-derived improvement of ischemia and pre-randomization higher stress echocardiography score, lower FFR/iFR values, and focal pattern of disease.
At a critical reading of the work, a potential limitation of the present analysis is related to the limited sample size (n = 164; 83 focal and 81 diffuse lesions). Furthermore, the operators were blinded to FFR/iFR and pullback values; PCI was not physiology-guided, and thus the current work must be read as a post-hoc analysis aiming to provide a potential interaction of the physiological pattern of disease on the results of the ORBITA trial and not as a pre-specified analysis investigating the impact of the physiological pattern of disease on operator decision before and after PCI and their impact on follow-up angina improvement.
Patients with diffuse stenoses had significantly higher values of FFR/iFR, with almost half of them showing non-ischaemic values. Furthermore, in the physiological defined diffuse pattern of disease were included also combined pattern of disease, which may have influenced the results of the analysis.
That being said, this study provides precious results, building up the evidence in favour of physiology-tailored PCI for stable CAD. In the iFR GRADIENT registry, iFRpred showed a strong linear relationship with iFRobs. Furthermore, the iFR pullback, compared to angiography-based strategy, led to the change of the revascularization strategy in one out of three cases, with the reduction of lesion number and length. Post-PCI assessment has shown residual ischemia in 20-30 % of the procedures with a significant impact on vessel-oriented adverse events. These findings suggest that physiology-guided procedural planning, combined with post-PCI assessment, may lead to a significant improvement of PCI outcomes and move the interventional practice towards a precision-medicine approach, having physiology-pullback as a guide.
References
- Al-Lamee R, Thompson D, Dehbi HM, et al (2018) Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomized controlled trial. Lancet 391:31–40.
- Al-Lamee R, Thompson D, Dehbi HM, Sen S, Tang K, Davies J, Keeble T, Mielewczik M, Kaprielian R, Malik IS, et al.; ORBITA Investigators. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomized controlled trial. Lancet. 2018; 391:31–40.
- Kikuta Y, Cook CM, Sharp ASP, et al (2018) Pre-Angioplasty Instantaneous Wave-Free Ratio Pullback Predicts Hemodynamic Outcome In Humans With Coronary Artery Disease: Primary Results of the International Multicenter iFR GRADIENT Registry. JACC Cardiovasc Interv 11:757–767.
- Ding D, Huang J, Westra J, et al (2021) Immediate post-procedural functional assessment of percutaneous coronary intervention: current evidence and future directions. Eur Heart J 353:1–16.
- Biscaglia S, Uretsky B, Barbato E, et al (2021) Invasive Coronary Physiology After Stent Implantation. JACC Cardiovasc Interv 14:237–246.
- Al-Lamee R, Howard JP, Shun-Shin MJ, et al (2018) Fractional flow reserve and instantaneous wave-free ratio as predictors of the placebo-controlled response to percutaneous coronary intervention in stable single-vessel coronary artery disease: Physiology-stratified analysis of ORBITA. Circulation 138:1780–1792.
- Warisawa T, Cook CM, Howard JP, et al (2019) Physiological Pattern of Disease Assessed by Pressure-Wire Pullback Has an Influence on Fractional Flow Reserve/Instantaneous Wave-Free Ratio Discordance. Circ Cardiovasc Interv 12:e007494.




