Uninterrupted oral anticoagulant therapy in patients undergoing unplanned percutaneous coronary intervention
Selected in JACC: Cardiovascular Interventions by D. Giacoppo
This large-scale analysis sought to compare interrupted and uninterrupted OAC therapy in patients taking OAC undergoing unplanned coronary angiography or PCI for suspected acute coronary syndrome.
References
Authors
Dimitrios Venetsanos, Mikolaj Skibniewski, Magnus Janzon, Sofia S. Lawesson, Emmanouil Charitakis, Felix Böhm, Loghman Henareh, Pontus Andell, Lars O. Karlson, Moa Simonsson, Sebastian Völz, David Erlinge, Elmir Omerovic, Joakim Alfredsson
Reference
10.1016/j.jcin.2021.01.022
Published
April 2021
Link
Read the abstractReviewer
My Comment
Why this study? – the rationale/objective
Approximately 10 % of patients undergoing percutaneous coronary intervention (PCI) are on oral anticoagulant (OAC), mainly due to atrial fibrillation, venous thromboembolism, or a mechanical prosthetic heart valve. There is limited evidence regarding the optimal peri-periprocedural anticoagulation strategy in patients taking OAC therapy undergoing coronary angiography or PCI.
Although recent European guidelines and consensus documents have endorsed uninterrupted vitamin-K antagonist therapy without bridging anticoagulation and 12-48 hours direct oral anticoagulants (DOAC) discontinuation in patients undergoing PCI, current practice remains heterogeneous for several reasons.
This large-scale analysis by Venetsanos and colleagues sought to compare interrupted and uninterrupted OAC therapy in patients taking OAC undergoing unplanned coronary angiography or PCI for suspected acute coronary syndrome.
How was it executed? – the methodology
The study is a retrospective analysis from the nationwide SWEDEHEART registry including patients taking OAC admitted in Sweden from 2005 to 2017 for suspected acute coronary syndrome.
The primary endpoint was a composite of major adverse cardiac and cerebrovascular events (MACCE) including all-cause death, myocardial infarction, or stroke at 3-month follow-up.
Secondary endpoints included individual safety and efficacy outcomes and a net composite endpoint of cardiac and cerebrovascular events (NACCE), including MACCE or major bleeding at 3-month follow-up. In-hospital bleeding and length of stay were also assessed by secondary analyses. Major non-coronary artery bypass grafting-related bleeding was defined as fatal or cerebral bleeding, bleeding requiring surgical intervention or blood transfusion, haemoglobin decrease > 3.0 g/dL with overt bleeding or ≥ 3.0 g/dL without overt bleeding during hospitalization or any rehospitalization for a cerebral, gastrointestinal, urogenital, or respiratory tract bleeding at 3-month follow-up.
Three different statistical methods were employed to account for the relevant risk of bias due to nonrandomized strategy assignment:
- multivariable mixed-effects Cox regression model, including variables with significant difference between groups at univariate analysis (fixed component) and accounting for participating centre clustering (random component);
- propensity score adjustment by inverse probability of treatment weights (IPTW) based on non-parsimonious inclusion of baseline characteristics and subsequent Cox regression model accounting for the centre of origin;
- nearest-neighbour propensity score 1:1 matching followed by Cox regression model accounting for the centre of origin.
Missing values were overcome by multiple imputations. In-hospital bleeding and length of stay were assessed by multivariable logistic regression and linear regression adjusted for calendar year, respectively.
What is the main result?
A total of 6,485 patients were included in the study, of whom 3,163 underwent procedure on uninterrupted oral anticoagulation and 3,322 on interrupted oral anticoagulation. The annual incidence increase of uninterrupted OAC therapy was 13 %. Since their introduction, DOAC have gradually replaced warfarin, with a proportion of 53 % in 2017.
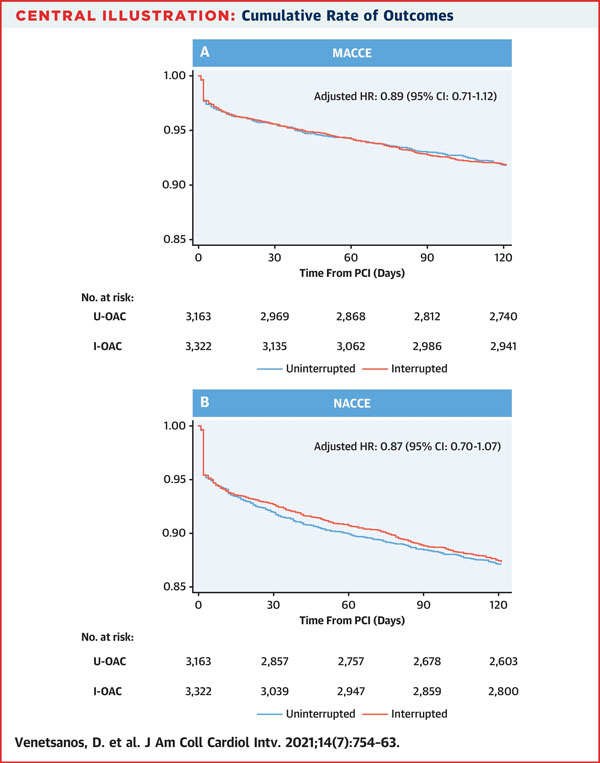
At 3 months, MACCE did not significantly differ between interrupted and uninterrupted OAC, regardless of the method used for adjustment (8.2 % vs. 8.2 %; crude: HR 1.00, 95 % CI 0.84-1.19; multivariable-adjusted: HR 0.94, 95 % CI 0.79-1.12; IPTW-adjusted: HR 0.89, 95 % CI 0.71-1.12; propensity score matching: HR 0.88, 95 % CI 0.70-1.09).
At 3 months, consistent results were observed in terms of NACCE (12.6 % vs. 12.9 %; crude: HR 0.98, 95 % CI 0.85-1.12; multivariable-adjusted: HR 0.90, 95 % CI 0.76-1.07; IPTW-adjusted: HR 0.87, 95 % CI 0.70-1.07; propensity score matching: HR 0.92, 95 % CI 0.76-1.12). Each of the individual endpoints of all-cause death, myocardial infarction, and stroke did not significantly differ between strategies at 3-month follow-up. No significant difference in major bleeding was observed between interrupted and uninterrupted OAC (5.6 % vs. 6.0 %; crude: HR 0.93, 95 % CI 0.76-1.15; multivariable-adjusted: HR 0.84, 95 % CI 0.66-1.06; IPTW-adjusted: HR 0.83, 95 % CI 0.65-1.05; propensity score matching: HR 0.92, 95 % CI 0.73-1.16).
Major or minor (4.1 % vs. 4.0 %; crude: HR 1.03, 95 % CI 0.81-1.33; multivariable-adjusted: HR 0.89, 95 % CI 0.68-1.18; IPTW-adjusted: HR 0.87, 95 % CI 0.67-1.13; propensity score matching: HR 0.91, 95 % CI 0.68-1.21) and major in-hospital bleeding events were not significantly different between groups.
Similar results were also found when in-hospital administration of low molecular weight heparin, fondaparinux, and glycoprotein IIb/IIIa inhibitors was not included in the multivariable analyses. There was no significant interaction between the type of OAC on arrival (warfarin vs. DOAC) and the strategy adopted in terms of MACCE (p = 0.98) or NACCE (p = 0.85). The length of in-hospital stay was significantly longer in patients in the interrupted OAC group than in patients in the uninterrupted OAC group (median 5 days, IQR 3-8 days vs. median 4 days, IQR 3-7 days; p < 0.01).
Source: JACC Cardiovascular Interventions
Critical reading and the relevance for clinical practice:
The rationale for OAC discontinuation in patients undergoing PCI relies on the assumptions that uninterrupted OAC can be responsible for a significant increase in the risk of peri-procedural bleeding compared with interrupted OAC and the management of possible major or life-threatening vascular complications during uninterrupted OAC is more challenging compared with peri-procedural conventional parenteral anticoagulation after interrupted OAC therapy.
The study by Venetsanos and colleagues showed that no significant difference between interrupted and uninterrupted OAC therapy strategies is observed in terms of MACCE, NACCE, all-cause death, myocardial infarction, stroke, and major bleeding at 3 months. Similar results were observed in terms of major or minor and major in-hospital bleeding events.
On the one hand, these results support the conclusion that interrupted OAC therapy in patients taking OAC before coronary angiography or PCI is not associated with increased rates of bleeding compared with interrupted OAC. In addition, safety of uninterrupted OAC therapy is further supported by the observation of quite comparable incidences between strategies for all major endpoints, including all-cause death and stroke.
On the other hand, the opposite view is that no significant clinical and prognostic benefit from uninterrupted over interrupted OAC was detected. Indeed, interruption of OAC before coronary angiography or PCI and use of bridging anticoagulation was not associated with any signal of harm in terms of bleeding and stroke. The only possible advantage of uninterrupted OAC therapy was a significantly reduced in-hospital length of stay, though the absolute effect was modest (i.e. approximately 1 day less).
A novel and interesting finding of the analysis by Venetsanos and colleagues is that uninterrupted anticoagulation with DOAC – strategy not clearly endorsed by current recommendations – seems to be effective and safe.
The results of the study by Venetsanos and colleagues need to be interpreted bearing in mind the following considerations:
- First, the design of the study was observational and selection bias in the choice of the strategy cannot be excluded despite adjustment. Indeed, the powerful methods of adjustment applied in the study rely on collected information and possible unmeasured confounders cannot be taken into account. However, no signal of inconsistency was detected across analyses and endpoints.
- Second, some important variables, including INR at the time of intervention, peri-procedural dose of unfractionated heparin, and duration of antiplatelet therapy after discharge were not available. Strong recommendations on daily clinical practice can be provided only by high-quality randomized clinical trials properly addressing all these crucial aspects of the matter.
- Finally, it was not clearly explored the relationships between strategy of peri-procedural anticoagulation and type of access and coronary artery disease complexity in patients undergoing PCI. Whether uninterrupted peri-procedural anticoagulation can be safely applied to large femoral sheaths interventions and high-risk interventions requires further analysis.




No comments yet!