26 Jan 2022
Cusp symmetry and coronary ostial eccentricity and its impact on coronary access following TAVR
Selected in JACC: Cardiovascular Interventions by M. Alasnag
Recently, coronary access has been recognized as an important consideration in the lifetime management of patients with severe aortic stenosis...
References
Authors
Xi Wang, Ole De Backer, Gintautas Bieliauskas, Ivan Wong, Vilhelmas Bajoras, Tian-Yuan Xiong, Yi Zhang, Klaus Fuglsang Kofoed, Mao Chen, and Lars Sondergaard
Reference
J Am Coll Cardiol Intv. 2022 Jan, 15 (2) 123–134
Published
January 2022
Link
Read the abstract
Reviewer
My Comment
Why this study – the rationale/objective?
Recently, coronary access has been recognized as an important consideration in the lifetime management of patients with severe aortic stenosis. Commissural alignment has been championed as the solution whereby the commissural posts of the transcatheter heart valves (THV) are aligned with the native commissures. 1Commissural alignment, however, is based on several assumptions including a standard angle between the center cusp and coronary ostia and the intercommissural angle.
Coronary access becomes even more critical in patients with bicuspid aortic valve (BAV) disease who present unique challenges. Firstly, they are younger hence access to the coronary tree may be necessary in the future. More importantly though, these patients suffer from an aortopathy in addition to the valvular degenerative process. Both the valvulopathy & aortopathy make the assumptions that form the basis of commissural alignment questionable. The angle between the commissures is not always 120° and the coronary arteries do not always originate from the center of the cusp. The cusp asymmetry & eccentricity of the coronary ostia necessitate alignment of the coronary arteries and not merely the post of the THV.
Furthermore, with valve-in-valve procedures, the position of the second THV commissural post must be carefully assessed. As such, several investigators have evaluated the role of cardiac computed tomography (CCT) in determining the best commissural projection and predicting coronary overlap. 2-3In the study by Wang et al, the main objective was to use a patient specific alignment technique determined by a CCT derived predictive model.
How was it executed? - the methodology
Four hundred patients from two centers were included in this study (200 patients with a trileaflet aortic valve (TAV) and 200 patients with type 1 bicuspid aortic valve). Baseline patient characteristics and preprocedural CCT measurements were collected from the local databases retrospectively. Cusp symmetry and coronary ostial eccentricity were assessed by CCT. In addition, the right and left coronary cusp and right coronary artery (RCA) and left coronary artery (LCA) ostia overlap views were defined using a centered-line that bisects the 2 commissures adjacent to the non-coronary cusp.
The fluoroscopic right and left cusp overlap views are generally determined by the hinge points of the Right and Left cusps at the annular level. The fluoroscopic Right and Left Coronary ostia overlap view was defined by overlapping the RCA and LCA ostia in the annular plane as well. The angular difference between the right and left cusp and coronary ostia overlap view was calculated by subtracting the coronary overlap fluoroscopic angle from the right and left anterior oblique projections as well as the caudal/cranial coordinates. The spatial distribution of the fluoroscopic views and the intra-patient angle difference were depicted in a scatterplot.
Student's t-test was used to compare continuous variables with normal distribution and expressed as mean ± SD. Chi-square test, Fisher exact test, or Cochran-Armitage trend tests were used for the categorical data.
What is the main result?
Sixty-one percent of the cohort were men. BAV patients were significantly younger with a mean age of 73 years (TAV patients were 78 years) and had fewer co-morbidities particularly Diabetes, hypertension, and coronary artery disease (21 % vs 30 %; p = 0.03).
Important differences in the CCT parameters include:
- Cusp Asymmetry: approximately 50 % of those with TAV had symmetrical cusps and only 2.5 % had severe asymmetry. While as, 52.5 % of those with BAV had severe asymmetry. Symmetric cusps were more commonly functional BAV. The NCC was the most common dominant cusp in both TAV (51 %) and BAV (85 %).
- Coronary Ostial Eccentricity: the RCA was more likely to have an eccentric origin compared with the LCA (P < 0.001). In BAV, LCA eccentricity was mild (94 %) vs 94.5 % in TAV. In those with more than mild RCA eccentricity, 95.5 % were located closer to the RCC-NCC commissure.
- Right & Left cusp/Right & Left coronary centered line: the RCC-LCC line overlapped and only mildly deviated from the commissure in 99.5 % of the TAV group and 97.0 % of the BAV group. A moderate deviation was reported in 1 patient with TAV and 6 with BAV. 97 % of patients with TAV and 93 % of those with BAV, had mild or less deviation (< 20°) between the RCC-LCC centered line and the RCA-LCA centered line.
- Cusp & Coronary Ostia overlap: the right and left cusp and coronary ostia overlap view differed by < 10° fluoroscopic angulation in 75 % of all patients with only 2.5 % having a difference of ≥ 20° in either an LAO/RAO or a cranial/caudal direction. Overall, the coronary ostia overlap view was calculated to be more RAO/caudal compared with the right/left cusp overlap view in 75.5 % of the TAV group and 64.0 % of the BAV group.
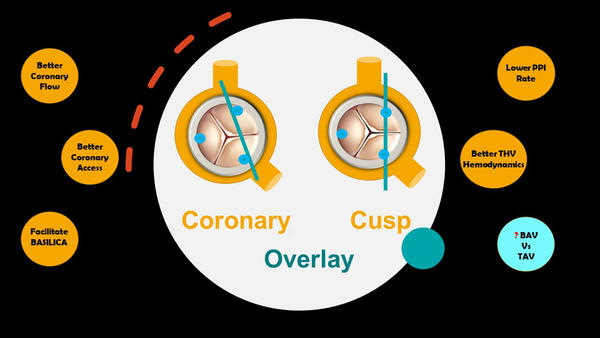
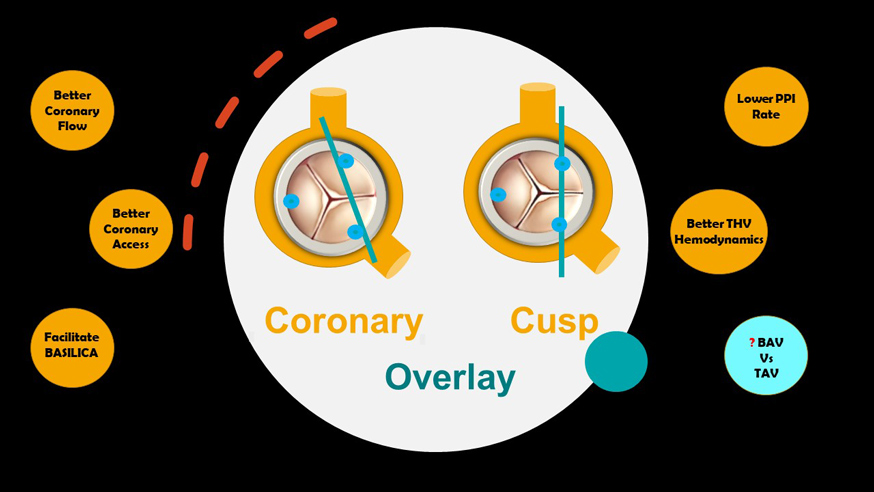
Commonly described overlay or alignment: cusp vs coronary
Source: with the courtesy of Mirvat Alasnag
Critical reading and the relevance for clinical practice
This study by Wang et al clearly demonstrated the higher frequency of severe cusp asymmetry in Type 1 BAV with the NCC being the most commonly dominant cusp. This suggests that the conventional commissural alignment may not adequately prevent coronary overlap. In another subset of patients, those undergoing valve-in-valve, Redondo et al also noted that one-third of these patients would have presented coronary overlap despite commissural alignment. Coronary eccentricity and the inter-coronary angle were the main predictors. This was reduced by 6-fold when coronary alignment was adopted3.
Appropriate alignment may facilitate, not only subsequent coronary access, but, theoretically, could also improve coronary flow, permit BASILICA for high-risk patients and improve hemodynamics after THV implantation. Already, there is similar propensity-matched data suggesting that cusp overlap could reduce permanent pacemaker implantation4.
Although the data is promising, it remains exploratory. The definitions of eccentricity and symmetry are not validated, not standardized, and arbitrary. How coronary alignment can be achieved with different THV technologies cannot be ascertained from this series, nor can inferences on other BAV types. 5Bieliauskas and colleagues evaluated neo-commissural alignment in different self-expanding valve designs (Evolut R/PRO, Medtronic; ACURATE neo2, Boston Scientific; and Portico, Abbott) with 20 patients in each arm. They concluded that patient-specific implantation techniques using neo-commissural alignment can prevent coronary overlap for all the studied THV iterations. However, they used fluoroscopy alone with its inherent limitations. From a technical perspective, achieving alignment of one coronary ostium may render the alignment of the other coronary ostium suboptimal. This is particularly true given the highly variable RCA origin in BAV and TAV.
Evaluating the collective data on coronary and commissural alignment, it is becoming abundantly clear that more sophisticated integrative imaging modalities are required and larger cohorts with different anatomies are necessary. Finally, in the future, it is anticipated that the role of fusion imaging to facilitate and achieve more accurate patient-specific alignment will grow significantly.
References
- Tang G.H.L., Zaid S., Fuchs A., et al. "Alignment of Transcatheter Aortic-Valve Neo-Commissures (ALIGN TAVR): impact on final valve orientation and coronary artery overlap". J Am Coll Cardiol Intv 2020;13:1030-1042.
- Wang X., Backer O.D., Bieliauskas G., et al. "Cusp symmetry and coronary ostial eccentricity and its impact on coronary access following TAVR". J Am Coll Cardiol Intv 2022;15:123-134.
- Redondo A., Baladrón Zorita C., Tchétché D., et al. "Commissural versus coronary optimized alignment during transcatheter aortic valve replacement". J Am Coll Cardiol Intv 2022;15:135-146.
- Pascual I., Hernández-Vaquero D., Alperi A., et al. "Permanent pacemaker reduction using cusp-overlapping projection in TAVR: a propensity score analysis". J Am Coll Cardiol Intv 2022;15:2: 150-161.
- Bieliauskas G., Wong I., Bajoras V., et al. "Patient-specific implantation technique to obtain neo-commissural alignment with self-expanding transcatheter aortic valves". J Am Coll Cardiol Intv 2021;14:19: 2097-2108.