Femoral or radial approach in treatment of coronary chronic total occlusion: A randomized clinical trial
Selected in JACC: Cardiovascular Interventions by A. Cader , S. R. Khan
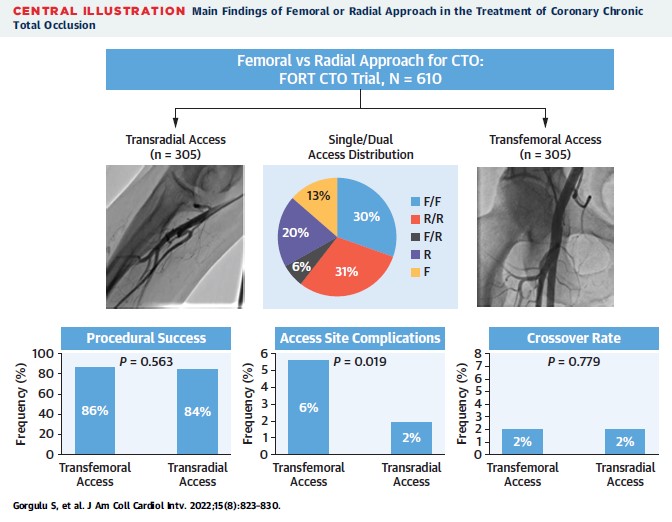
Access remains an increasingly discussed issue in the interventional community globally. In this FORT CTO trial, the authors reported no difference in procedural success in TRA vs TFA, among CTO patients.
References
Authors
Sevket Gorgulu, Nihat Kalay, Tugrul Norgaz, Cuneyt Kocas, Omer Goktekin, and Emmanouil S. Brilakis
Reference
J Am Coll Cardiol Intv. 2022 Apr, 15 (8) 823–830
Published
15 April 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
A “Radial First” approach is being increasingly undertaken for complex percutaneous coronary interventions (PCI) procedures including chronic total occlusions (CTO), predominantly owing to fewer vascular access complications, less bleeding and better outcomes.1 CTO PCI has been traditionally performed via transfemoral access (TFA), mainly to allow for larger guide catheters necessary to navigate devices for complex PCI.2 Registry and observational data exist for Transradial access (TRA) in CTO PCI,1,3 however, there is no randomised evidence of TRA vs TFA in CTO PCI.
The FORT CTO trial was the first randomised controlled trial (RCT) to examine the feasibility and impact of TRA vs TFA on outcomes of CTO PCI.4
How was it executed? - the methodology
Design: FORT CTO was a multi-centre, parallel-arm, non-inferiority design RCT.
Population: All consecutive patients referred for CTO PCI at 4 centres in Turkey were screened and enrolled.
Exclusion criteria were as follows:
- Any acute coronary syndrome within 3 months
- Severe heart failure
- Severe renal failure, defined as eGFR <15 mL/min/1.73 m2 and unresponsive to medical treatment (except for dialysis patients, who were eligible)
Intervention & Comparator: Patients were randomised 1:1 to TRA or TFA. For TRA, a radial access ONLY approach was mandated by protocol (i.e. single TRA or bi-radial TRA if dual injection required). For TFA arm, in addition to the main access being transfemoral, a radial access was allowed for donor vessel injection.
Access, sheath removal and haemostasis:
TRA: 20-gauge open-bore needles were used for puncture, only via proximal radial access, with no ultrasound guidance. 6-F short hydrophilic or 7-F Glidesheath Slender sheaths were used. Upon sheath removal, a patent haemostasis technique was applied. Radial artery patency was assessed by reverse Barbeau test. Suspected radial artery occlusion was confirmed by Doppler ultrasound.
TFA: Access was achieved by Seldinger technique by 18-gauge needle without fluoroscopic or ultrasound guidance. 6-, 7-, or 8-F artery sheaths were used. Sheaths were removed 6 hours after CTO PCI. Haemostasis was achieved by manual compression, followed by application of pressure by a sandbag for 6 hours. Arterial closure devices were not used.
Operators: All procedures were performed by 4 interventional cardiologists, who were experienced in both CTO PCI (>100 cases/year) and radial access.
Outcomes: The primary outcome was procedural success, defined as technical success without any in-hospital major adverse cardiovascular events (MACE). In-hospital MACE were death, myocardial infarction, repeat target vessel revascularization with PCI or coronary artery bypass graft (CABG) surgery, tamponade requiring either pericardiocentesis or surgery, and stroke.
The secondary endpoint was a safety endpoint, comprising of major access-site complications. This included major bleeding (BARC≥3).
Statistical analysis: The noninferiority margin was set at 7%, selected on the basis of the variation of technical success in several large CTO PCI registries. Assuming 90% procedural success in the TFA group, at a 1-sided alpha level of 0.025, the sample size required for 80% power using 1-sided Student’s t-test was 578 patients. This was increased to 610 patients to account for potential losses between enrolment and performance of the procedure.
What is the main result?
Over 4 years, 610 patients were randomized to TRA (n =305) or TFA (n =305). The mean age was 61±10 years, 83% were men.
The target vessel was the right coronary artery in 48%, left anterior descending coronary artery, in 35% and left circumflex in 17% of patients.
The mean J-CTO (2.1 ± 0.1 vs 2.2 ± 0.1; P = 0.279), PROGRESS CTO (1.3 ± 0.9 vs 1.1 ± 1.0; P = 0.058) and PROGRESS CTO complication (2.4 ± 1.8 vs 2.3 ± 1.8; P =0.561) scores were not significantly different between TRA vs TFA respectively.
As for the primary endpoint, there were no differences in procedural success between TRA vs TFA (84% vs 86%; P =0.563), reported to reflect that TRA was non-inferior to TFA in the manuscript. There were no differences in the individual components of MACE in each arm. In terms of secondary endpoint, fewer access-site complications (2.0% vs 5.6%; P = 0.019) were seen with TRA than with TFA.
No differences were seen between TFA and TRA in procedural duration, contrast volume, or radiation dose. A notable caveat is the extremely low usage of IVUS (0.5% in both arms).
Sheath size of target vessel access: A 7 F was the predominant sheath size used in both arms, with significantly more frequent use in TFA than TRA (95% vs 76%; p=0.001). 6 F sheaths were used more frequently in the TRA arm, as compared with TFA (24% vs 4%; p=0.001).
Guide size for target vessel: Overall, the predominant guide size was also 7F. However, for the target vessel, TFA patients were more likely to receive 7-F guide catheters, as compared with TRA patients (95% vs 76%; P= 0.001); 23% of TRA patients received a 6 F guide, as compared with just 4% in the TFA arm (p=0.001).
CTO crossing technique: Overall, the predominant strategy was antegrade (antegrade wiring and antegrade dissection & re-entry), with no differences between both arms (94% vs 96% for TRA vs TFA; p=0.429). Retrograde techniques were used in 11% of TFA and 14% of TRA (p=0.342).
Dual access was less common in the TRA group (61% vs 73%; P=0.002). All those who received dual access in the TRA arm had bi-radial access. Additionally, in the TFA arm, 12% had a radial approach for donor vessel access.
Similar crossover rates were seen in both arms (P = 0.779). Notably, the majority of crossovers were related to issues pertaining to their relative access sites and the arteries involved, and not owing to the CTO PCI itself.
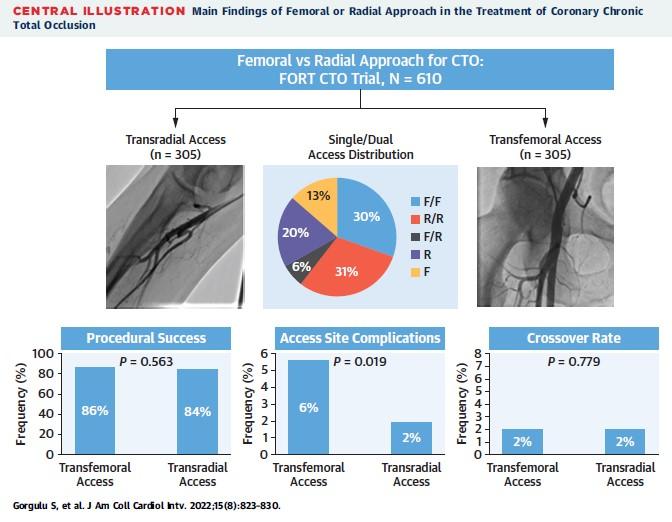
Access distribution, primary and secondary endpoints in TRA vs TFA for CTO PCI
Source: JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice
In this FORT CTO trial, the authors reported no difference in procedural success in TRA vs TFA, among CTO patients.4 The trial was designed as non-inferiority; however, the primary outcomes of procedural success were reported as similar with TRA and TFA, with non-significant p value (i.e. p values for inferiority per se, were not mentioned). Fewer access-site complications were reported in the TFA arm.
Access remains an increasingly discussed issue in the interventional community globally. While complex PCI is being increasingly performed via TRA, lesser uptake may have been observed in case of CTO PCI. TFA was preferred owing to the need for larger bore access, to pass bulkier equipment for CTO PCI, and also the need for better support.
However, high technical and procedural success was noted in FORT CTO, despite the very low uptake of IVUS in both arms. This may be explained by the fact that cases were only performed by experienced CTO operators, and that the lesions were not of complexity as high as contemporary registries: Indeed, in FORT CTO, relatively lower J-CTO and PROGRESS CTO scores were observed, which could potentially be the reason for successful crossing by a predominantly antegrade approach. These factors may limit the generalizability of the study’s findings to a wider, more complex CTO subset and less operator experience.
Support has been a key issue in complex PCI, and a frequent reason to opt for TFA. While lesion complexity, and therefore strategy (antegrade vs retrograde) are certainly factors determining need for better support, given the procedural success observed in this trial, it is reasonable to accept that adequate support can be achieved via both routes in CTOs of intermediate grade complexity.
Indeed, in the slender PCI approach propagated by Japanese colleagues, mechanisms to enhance active support have been described, such as the formation of alpha, gamma and epsilon loops, deep intubation of the guide, and use of guide extension catheters etc. Particularly for CTO PCI by antegrade approach, the “SATAI” (Stiff And Tapered guide wire penetration technique on Antegrade Intervention) technique has been described.5
The Global CTO Crossing Algorithm advocates for good visualisation of the CTO segment by dual injection as a preliminary step.6 In FORT CTO, over a quarter of patients did not receive dual access, with it being significantly lesser in the TRA arm. The proportions of patients in each arm that had ipsilateral collaterals only, therefore obviating the need for dual access, is not clear.
Furthermore, recently an alternative Minimalistic Hybrid Algorithm (MHA) has been proposed and validated, which aims to limit the use of dual injection, and enhance the uptake of TRA and smaller size guides for CTO PCI.7 Indeed, large bore guides have the greatest utility in ADR techniques, and less so in antegrade wiring, a fact that has also been noted by proponents of the MHA.7
As for access, while TRA demonstrated significantly fewer access site complications, this needs to be interpreted in the light of some limitations: While TRA was also not achieved with ultrasound guidance, in case of TFA, none of the contemporary best practices for puncture (ultrasound/ fluoroscopy guidance, micropuncture needles) were applied, which may have led to more access-related complications in this arm. Furthermore, manual haemostasis was applied in TFA, without the use of closure devices.
Alternatively, in the TRA arm, patent haemostasis was applied, which was reflected by low incidence of radial artery occlusion (RAO), even though this was an exploratory endpoint and RAO assessment was not done routinely for all patients via duplex ultrasound. Nevertheless, given that RAO is the bane of TRA, this low incidence observed is encouraging, especially in case of bi-radial access, which was the case in all dual access seen in the TRA arm.
The protocol mandated that TRA would be allowed for donor vessel access in the TFA arm, but not vice versa. As such, there were 491 transradial access sheaths applied in the trial. Thus, the fact that the TRA arm experienced fewer access-site complications, despite their being more TRA access overall in the trial, further validates a Radial First approach for at least one of the CTO access sites. Having said that, in those with narrow radial arteries unable to accommodate larger sheaths (6 F or greater), a TRA approach may not be possible.
In light of FORT CTO, what would be your default approach for access in CTO PCI?
References:
- Burzotta F, De Vita M, Lefevre T, et al. Radial approach for percutaneous coronary interventions on chronic total occlusions: technical issues and data review. Catheter Cardiovasc Interv. 2014 Jan 1;83(1):47-57.
- Brilakis ES, Grantham JA, Rinfret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. J Am Coll Cardiol Intv. 2012;5:367–379.
- Wu CJ, Fang HY, Cheng CI, et al. The safety and feasibility of bilateral radial approach in chronic total occlusion percutaneous coronary intervention. Int Heart J. 2011;52:131–138.
- Gorgulu S, Kalay N, Norgaz T, et al. Femoral or Radial Approach in Treatment of Coronary Chronic Total Occlusion: A Randomized Clinical Trial. JACC Cardiovasc Interv. 2022 Apr 25;15(8):823-830
- Kiemeneij F, Yoshimachi F, Matsukage T, et al. Focus on maximal miniaturisation of transradial coronary access materials and techniques by the Slender Club Japan and Europe: an overview and classification. EuroIntervention. 2015;10(10):1178-86.
- Wu EB, Brilakis ES, Mashayekhi K, et al. Global Chronic Total Occlusion Crossing Algorithm: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021;78(8):840-853.
- Agostoni P, Scott B, Budassi S, et al. A prospective evaluation of a redefined version of the "minimalistic hybrid approach" algorithm for percutaneous coronary chronic total occlusion revascularization. Catheter Cardiovasc Interv. 2021;98(4):617-625.





No comments yet!