17 Jun 2022
Prognostic impact of extra–mitral valve cardiac involvement in patients with primary mitral regurgitation
Selected in JACC: Cardiovascular Imaging by S. Fezzi , M. Pighi
This report builds up the evidence on the relevance of extra-valvular cardiac damage staging / involvement as a main predictor of adverse events in patients with VHD undergoing intervention, either surgical or percutaneous.
References
Authors
Aniek L. van Wijngaarden, Valentina Mantegazza, Yasmine L. Hiemstra, Valentina Volpato, Pieter van der Bijl, Mauro Pepi, Meindert Palmen, Victoria Delgado, Nina Ajmone Marsan, Gloria Tamborini, and Jeroen J. Bax
Reference
J Am Coll Cardiol Img. 2022 Jun, 15 (6) 961–970
Published
June 2022
Link
Read the abstractReviewers
Our Comment
Why this study – the rationale/objective?:
According to the current recommendations, the indication to treat primary mitral regurgitation (MR) is based on the severity of MR and on the presence of symptoms, left ventricular (LV) dilatation and dysfunction, atrial fibrillation, and pulmonary hypertension.
Extra-valvular cardiac damage staging system, firstly proposed by Généreux, was shown to be a strong predictor of adverse events at follow-up in patients with severe aortic stenosis (AS) undergoing aortic valve replacement (AVR), both surgical and transcatheter1,2,3.
However, this classification has not been previously assessed in patients with primary MR.
How was it executed? - the methodology:
- Patients with moderate-to-severe or severe primary MR (i.e., degeneration or prolapse) who underwent MV surgery at Leiden University Medical Center (Leiden, the Netherlands) or at Centro Cardiologico Monzino (Milan, Italy) were included. Patients with infective endocarditis, rheumatic heart disease, and previous valvular intervention were excluded.
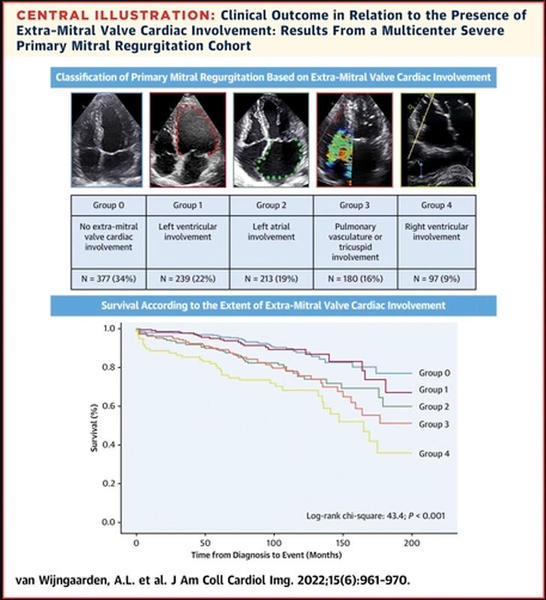
- Among the overall population (n = 1,106), the extent of cardiac damage was assessed and classified according to echocardiography prior to surgery in 5 groups:
- group 0 (34 %), with no signs of extra-MV cardiac involvement;
- group 1 (22 %), LV involvement (LV end-systolic diameter ≥ 40 mm, LV end-systolic volume index ≥ 30 mL/m2, or LV ejection fraction ≤ 60 %);
- group 2 (19 %), LA involvement (LA maximum diameter ≥ 55 mm or history of atrial fibrillation);
- group 3 (16 %), pulmonary artery vasculature or tricuspid valve involvement (systolic pulmonary artery pressure > 50 mm Hg or TR grade > 2);
- or group 4 (9 %), RV involvement (TAPSE ≤17 mm).
- The interaction of extravalvular cardiac damage with all-cause mortality at the very long-term follow-up (median time 88 months) was assessed.
What is the main result?
- In this large cohort of primary MR patients, a high proportion had some degree of extra-valvular cardiac damage. Patients in the higher extra-MV cardiac involvement groups were older and presented more frequently with diabetes mellitus and coronary artery disease. Moreover, had more severe symptoms, worse renal function, and more frequently used diuretic medications.
- The extent of cardiac damage was confirmed to be strongly associated with increased mortality at the very long-term follow-up (log-rank chi-square = 43.4; P < 0.001), with a significant increase in mortality for each worsening of the staging, excluding stage 1.
- After multivariate Cox regression, the group of extra-MV cardiac involvement was an independent predictor of all-cause mortality, together with age, male sex, chronic obstructive pulmonary disease, and renal function. For each increasing group, a 17 % higher risk for all-cause mortality was observed (95 % CI: 1.051-1.313; P = 0.005).
Source = JACC: Cardiovascular Imaging
Critical reading and the relevance for clinical practice:
This report builds up the evidence on the relevance of extra-valvular cardiac damage staging / involvement as a main predictor of adverse events in patients with valvular heart disease undergoing intervention, either surgical or percutaneous, as previously reported in the setting of AS.
To date, the indication to treat primary MR relies on the severity of the disease and on the presence of symptoms, left ventricular (LV) dilatation and dysfunction, atrial fibrillation, and pulmonary hypertension.
Nevertheless, in this original analysis, LV involvement, namely LV dilatation or disfunction, was not associated with worse outcomes, whilst both left atrium dilatation and right ventricle dysfunction were strictly related to mortality.
For many years, the tricuspid valve and right heart have been regarded as the “forgotten valve” with a presumed limited impact on hemodynamics and outcomes and a frequent consequent conservative management.
However, the combined presence of tricuspid regurgitation and left-side valvular disease is common and clinically relevant, as severe TR has been shown to be related to worse outcomes during follow-up4,5. To date, it is not still clear whether TR is directly linked to the increased mortality or is a marker of a more advanced underlying left-side disease and comorbidities6.
In the setting of MitraClip repair, a similar staging system has been described stratifying patients according to the presence of severe MR without right heart damage (stage 0), moderate-to-severe TR (stage 1), and right ventricular dysfunction (stage 2).
Rates of one-year all-cause mortality increased with more advanced stages of right heart remodeling (stage 0: 8.0 % vs stage 1: 9.7 % vs stage 2: 18.1 %; p < 0.001)7.
In the setting of transcatheter aortic valve implantation (TAVI), cardiac damage was shown to be one of the main predictors of renal function following AVR. Interestingly, acute kidney injury following TAVI was associated with a higher incidence of all-cause mortality, with a significant impact only in advanced cardiac damage stages but not in the early ones. Thus, interventions at an earlier stage, when the cardiac damage is not already established, may reduce mortality and clinical adverse events and preserve renal function3,8.
The use of this new staging system may improve patient care, risk stratification, assessment of the prognosis, and guide towards the heart-team decision-making process in patients with moderate-to-severe MR. Indeed, an intervention before the natural history of the valvular disease reaches a severe and symptomatic state could potentially limit the extent of cardiac damage, thus leading to improved long-term outcomes.
On the other side, cardiac damage staging classification could be particularly helpful by preventing futile treatments in advanced phases, when the worse prognosis may mitigate the advantage of valve replacement.
References
- Généreux P, Pibarot P, Redfors B, Mack MJ, Makkar RR, Jaber WA, Svensson LG, Kapadia S, Tuzcu EM, Thourani VH, Babaliaros V, Herrmann HC, Szeto WY, Cohen DJ, Lindman BR, McAndrew T, Alu MC, Douglas PS, Hahn RT, Kodali SK, Smith CR, Miller DC, Webb JG, Leon MB. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur Heart J. 2017;38:3351–8.
- Vollema EM, Amanullah MR, Arnold CT, van der Bijl P, Prevedello F, Sin YK, Prihadi EA, Marsan NA, Ding ZP, Généreux P, Pibarot P, Leon MB, Narula J, Ewe SH, Delgado V, Bax JJ. Staging Cardiac Damage in Patients With Symptomatic Aortic Valve Stenosis. J Am Coll Cardiol. 2019;74:538–49.
- Pighi M, Fezzi S, Pesarini G, Venturi G, Giovannini D, Castaldi G, Lunardi M, Ferrero V, Scarsini R, Ribichini F. Extravalvular Cardiac Damage and Renal Function Following Transcatheter Aortic Valve Implantation for Severe Aortic Stenosis. Can J Cardiol. 2021;37:904–12.
- Khan F, Okuno T, Malebranche D, Lanz J, Praz F, Stortecky S, Windecker S, Pilgrim T. Transcatheter Aortic Valve Replacement in Patients With Multivalvular Heart Disease. JACC Cardiovasc Interv. 2020;13:1503–14.
- Mantovani F, Fanti D, Tafciu E, Fezzi S, Setti M, Rossi A, Ribichini F, Benfari G. When Aortic Stenosis Is Not Alone: Epidemiology, Physiopathology, Diagnosis, and Management in Mixed and Combined Valvular Disease. Front Cardiovasc Med. 2021;8:1–10.
- McCarthy FH, Vemulapalli S, Li Z, Thourani V, Matsouaka RA, Desai ND, Kirtane A, Anwaruddin S, Williams ML, Giri J, Vallabhajosyula P, Li RH, Herrmann HC, Bavaria JE, Szeto WY. Association of Tricuspid Regurgitation With Transcatheter Aortic Valve Replacement Outcomes: A Report From The Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. Ann Thorac Surg. 2018;105:1121–8.
- Shamekhi J, Sugiura A, Spieker M, Iliadis C, Weber M, Öztürk C, Becher MU, Tiyerili V, Zimmer S, Horn P, Westenfeld R, Pfister R, Mauri V, Sinning J, Kelm M, Baldus S, Nickenig G. A staging classification of right heart remodelling for patients undergoing transcatheter edge-to-edge mitral valve repair. EuroIntervention. 2021;17:1–8.
- Fezzi S, Pighi M, Ribichini F. Acute Kidney Recovery Following Transcatheter Aortic Valve Implantation: A Matter of Definition? Am J Cardiol. 2022:6–8.






