Sex-related characteristics and short-term outcomes of patients undergoing transcatheter tricuspid valve intervention for tricuspid regurgitation
Selected in European Heart Journal by J. Curio , A. Sticchi
Population-based studies show a higher prevalence of significant TR in women and following that in published and ongoing trials on TTVI more women than men were enrolled. However, so far it has not been investigated whether such differences in epidemiology also would affect TTVI outcomes...
References
Authors
Andrea Scotti, Augustin Coisne, Maurizio Taramasso, Juan F Granada, Sebastian Ludwig, Josep Rodés-Cabau, Philipp Lurz, Jörg Hausleiter, Neil Fam, Susheel K Kodali, Joel Rosiene, Ari Feinberg, Alberto Pozzoli, Hannes Alessandrini, Luigi Biasco, Eric Brochet, Paolo Denti, Rodrigo Estevez-Loureiro, Christian Frerker, Edwin C Ho, Vanessa Monivas, Georg Nickenig, Fabien Praz, Rishi Puri, Horst Sievert, Gilbert H L Tang, Martin Andreas, Ralph Stephan Von Bardeleben, Karl-Philipp Rommel, Guillem Muntané-Carol, Mara Gavazzoni, Daniel Braun, Benedikt Koell, Daniel Kalbacher, Kim A Connelly, Jean-Michel Juliard, Claudia Harr, Giovanni Pedrazzini, Giulio Russo, François Philippon, Joachim Schofer, Holger Thiele, Matthias Unterhuber, Dominique Himbert, Marina Ureña Alcázar, Mirjam G Wild, Stephan Windecker, Ulrich Jorde, Francesco Maisano, Martin B Leon, Rebecca T Hahn, Azeem Latib
Reference
Eur Heart J . 2022 Nov 29;ehac735
Published
November 2022
Link
Read the abstract
Reviewers
Our Comment
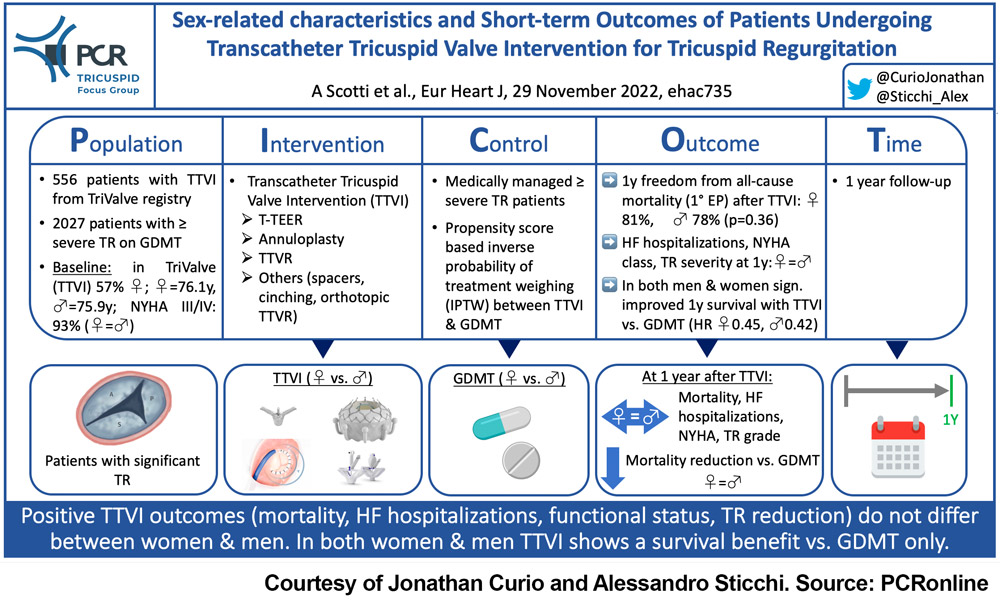
Figure 1: Picot scheme highlighting key aspects of the study. Source: courtesy of Jonathan Curio and Alessandro Sticchi
Why this study – the rationale/objective?
Symptomatic severe tricuspid regurgitation (TR) is associated with a significantly increased rate of mortality (1). However, isolated surgical treatment of TR remains associated with high peri-procedural mortality, which leads to the development of less invasive transcatheter tricuspid valve intervention (TTVI) approaches (2). A broad range of devices has emerged, aiming to either repair (edge-to-edge repair [TEER], annuloplasty, spacers) or replace the tricuspid valve. The so far largest experience with these devices has been reported based on the TriValve registry (NCT03416166), which included patients treated with all different available approaches and did report up to 1.5-year mid-term results (3).
Thus, the present study investigated sex-related differences regarding clinical presentation and TTVI outcomes as well as TTVI treatment effects in comparison to optimal medical therapy (OMT).
How was it executed? - the methodology
The TTVI cohort consisted of patients from the TriValve registry (patients from 24 European and North American centers mainly treated with TEER, replacement or annuloplasty). The OMT control group was formed by consecutive patients with the echocardiographic diagnosis of ≥ severe TR during a time when no TTVI was available (2015-2018). TTVI outcomes were evaluated for women vs. men and were compared to outcomes with OMT only using propensity score-based inverse probability of treatment weighting (IPTW).
- Primary endpoint: freedom from all-cause mortality at 1 year
- Secondary endpoints: HF hospitalizations, NYHA functional class, TR severity at 1 year
What is the main result?
The study assessed clinical outcomes in 556 patients (56.8% women) from the TriValve registry receiving TTVI in addition to OMT, and in 2072 patients (64.4% women) receiving OMT alone.
Mean age in TTVI patients was 76 years, EuroSCORE II was 6.3%, and 93% of patients were in NYHA class III/IV at baseline (each without any differences between women and men).
- Women receiving TTVI were less likely to have ascites (20.3% vs. 31.1% in men, p<0.01), had fewer previous hospitalizations for RV failure (65.1% vs. 75.7% in men, p=0.02), and men had more pacemaker or ICD leads across the tricuspid valve (31.2% vs. 21.6% in women, p=0.02); LVEF was higher in women (54% vs. 46% in men, p<0.01)
- Freedom from all-cause mortality at 1 year was without differences between women and men (80.9% vs. 77.9%, p=0.56)
- The rates of HF hospitalizations, patients in NYHA functional class III/IV and patients with TR >2+ at 1 year likewise were without differences between women and men
- Cox-regression, weighted using IPTW, comparing TTVI with OMT alone showed a significantly improved 1-year survival in both women (HRadj 0.45, p=0.01) and men (HRadj 0.42, p=0.03).
Critical reading and the relevance for clinical practice
Understanding the pathophysiological differences between women and men has been a topic of growing interest in recent years. Given known outcome differences for other interventions and given the difference between women and men seen in epidemiological studies, it is of high relevance to assess potential sex differences regarding outcomes of TTVI.
Therefore, the result of this study is highly relevant, showing beneficial outcomes after TTVI without any larger sex disparities.
However, it is important to refer this mortality data, especially in such elderly cohorts, to the general population’s life expectancy, which usually differs between women and men. For example, in the US, the probability of dying within 1 year for women 76 years of age (mean age of study population) is 2.7%, and for men it is 3.8% (4). 1-year mortality rates seen in this study are markedly higher, likely due to the underlying disease and comorbidities, while the statistically non-significant numerical difference between sexes reported seems similar to that of the general population.
For clinical practice and patient care pathways, the reported differences in the baseline presentation between women and men are of great importance and a more granular analysis might be needed to understand whether these baseline differences impact during follow-up. This could be especially important when looking at outcomes after different devices and treatment approaches. Potentially, device selection algorithms could be influenced by such baseline differences.
It is encouraging to see that, irrespective of sex, the IPTW weighting-based analysis comparing TTVI to GDMT alone shows a significant treatment effect with a reduction in mortality. This is in line with a previous propensity-matched analysis of TriValve data, that compared TTVI with GDMT-managed patients from two large European and North American registries (5).
Nonetheless, randomized controlled trials are needed to definitely prove the beneficial effects of adding TTVI to GDMT. These studies randomizing versus GDMT are currently ongoing, testing either T-TEER (CLASP II TR, NCT04097145; TRILUMINATE, NCT03904147) or orthotopic replacement (TRISCEND II, NCT04482062).
Finally, this study gives us the encouraging message that, based on currently available non-randomized data, regarding 1-year mortality TTVI, without any sex-related compromise, seems to provide a beneficial treatment for patients with significant TR and bears the potential to reduce mortality in comparison to GDMT alone, similarly for both women and men.
References
- Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol 2004;43:405-9.
- Praz F, Muraru D, Kreidel F et al. Transcatheter treatment for tricuspid valve disease. EuroIntervention 2021;17:791-808.
- Taramasso M, Alessandrini H, Latib A et al. Outcomes After Current Transcatheter Tricuspid Valve Intervention: Mid-Term Results From the International TriValve Registry. JACC Cardiovasc Interv 2019;12:155-165.
- Social Security Administration U. Actuarial Period Life Table. 2019. Available at: https://wwwssagov/oact/STATS/table4c6html.
- Taramasso M, Benfari G, van der Bijl P et al. Transcatheter Versus Medical Treatment of Patients With Symptomatic Severe Tricuspid Regurgitation. J Am Coll Cardiol 2019;74:2998-3008.







No comments yet!