15 Jun 2023
The 17th expert consensus document of the European Bifurcation Club – techniques to preserve access to the side branch during stepwise provisional stenting
Selected in EuroIntervention Journal by A. Cader , A. N. Calik
Provisional stenting (PS) is the default approach for treating most coronary bifurcation lesions (CBL). The side branch (SB) can be compromised after main vessel (MV) stenting in up to 6-18 % of cases. The 17th Expert consensus document of the European Bifurcation Club details strategies for SB preservation & restoring its patency1.
References
Authors
Manuel Pan, Jens Flensted Lassen, Francesco Burzotta, Soledad Ojeda, Remo Albiero, Thierry Lefèvre, David Hildick-Smith, Thomas W. Johnson, Alaide Chieffo, Adrian P Banning, Miroslaw Ferenc, Olivier Darremont, Yiannis S. Chatzizisis, Yves Louvard, Goran Stankovic
Reference
EuroIntervention 2023;19:26-36. DOI: 10.4244/EIJ-D-23-00124
Published
May 12, 2023
Link
Read the abstract
Reviewers
Our Comment
What are the key points?
A SB is “relevant” if:
- reference vessel diameter is ≥ 2.0 mm
- represents a significant territory (> 10 %) of the myocardium, impacting prognosis (an SB length ≥ 73 mm is assumed to supply ≥ 10% myocardial mass)
- a SB the operator is unwilling to lose in context of patient’s anatomy
Mechanism of SB occlusion is usually a combination of carina shift and longitudinal plaque shift. Most prevalent cause is over-dilatation of MV stent, and thus MV stent must be sized according to distal MV diameter, followed by proximal optimisation technique (POT) above the carina level.
Predictors of SB occlusion:
- On IVUS: Carina with spiky morphology (Eyebrow sign)
- On OCT: High lipid content of MV lesion and a contralateral location of lipid in the bifurcation area, narrower carina tip angle, shorter length between the proximal branching point to the carina tip, calcified plaque in the MV
- On angiography: severe diameter stenosis in both branches, lesion length, bifurcation angle ≥ 90 degrees, thrombus-containing lesion.
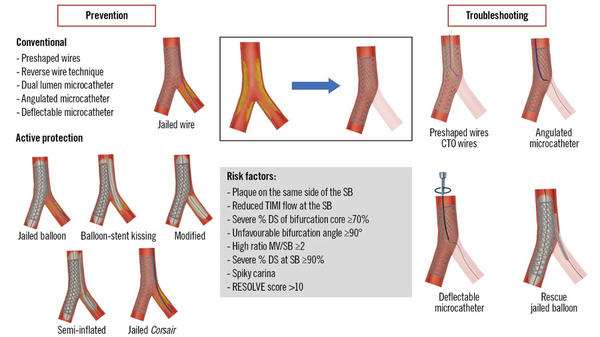
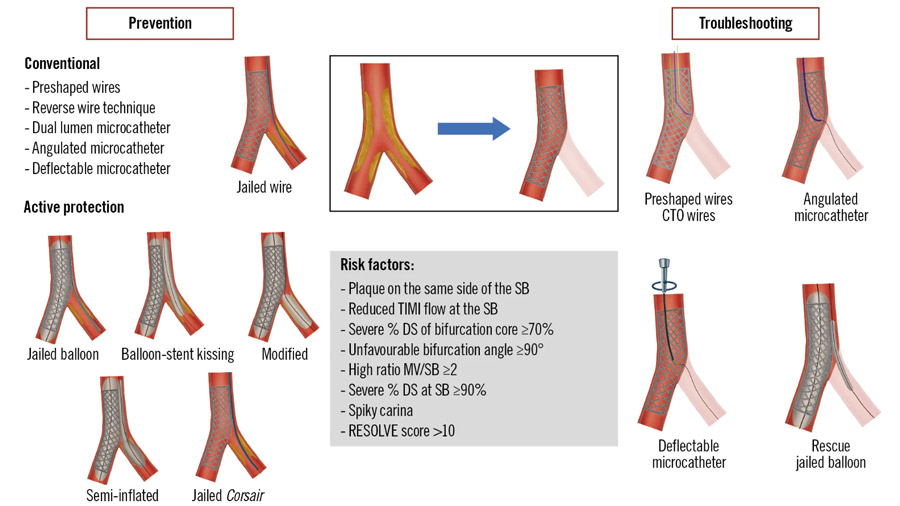
Central illustration: Preserving SB access during provisional stenting. CTO: chronic total occlusion; DS: diameter stenosis; MV: main vessel; RESOLVE: Risk prEdiction of Side branch OccLusion in coronary bifurcation intervention; SB: side branch; TIMI: Thrombolysis in Myocardial Infarction.
Source: EuroIntervention Journal
The RESOLVE [Risk prediction of Side branch OccLusion in coronary bifurcation interVEntion] score is a risk stratification score system of 6 variables [plaque distribution (on the opposing or same side of the SB), Thrombolysis in Myocardial Infarction (TIMI) flow grade of the MV before stenting, preprocedural diameter stenosis of the bifurcation core (%), bifurcation angle, diameter ratio between MV/SB and diameter stenosis of the SB before MV stenting (%)] to help predict SB occlusion2. RESOLVE score ≥ 10 points is considered high-risk, with SB occlusion probability ~ 20 %. A modified V-RESOLVE score is available3.
The jailed wire technique
Leaving a wire in the SB during MV stenting has been recommended by previous EBC consensus documents4,5, due to advantages of keeping the SB open, as a marker for SB ostium, facilitating SB access, anchoring guide catheter and bailout by passage of low-profile balloon. The risk of wire fracture is low, but best to avoid long jailed segments (> 15-20 mm) in calcified vessels.
New evidence supporting jailed wires:
In a bifurcation-CTO lesions series treated mainly by provisional stenting, SB non-protection was linked to procedural failure and periprocedural myocardial infarction6.
In the COBIS III Registry, SB wire jailing led to lower rates of final SB occlusion in those with MV and SB stenosis ≥ 60 %, but not other CBL. Therefore, this group recommended routine SB wire jailing only for complex CBL treated by PS, not all7.
In the EBC MAIN Study, failure to rewire SB was more common when jailed wires were not used8.
Current consensus:
While baseline SB wiring is recommended, but there is currently no definite consensus on which anatomies a jailed wire is considered essential. However, if SB is compromised after MV predilatation, the SB should always be wired1.
Baseline SB wiring in challenging anatomies
SB wiring is challenging in extreme vessel tortuosity, extreme angulation at SB origin or severe MV and SB stenosis. Selection of optimal view to visualise each ostium is vital.
Several techniques to wire challenging SBs are detailed in the consensus document1:
- Preshape wire tip according to bifurcation anatomy. 4 typical curves: 1) a single bend with a short (2-3 mm) tip, 2) a single bend with a long (4-6 mm) tip, 3) a single wide-angled bend and 4) a double-bend shape.
If this fails, more sophisticated techniques can be used:
- Reverse wire technique: two sharp curves at wire tip, a long proximal one, which creates a loop in the distal MV; an opposite short distal one, which engages SB ostium during the wire pullback. Dual lumen/ angulated microcatheters facilitate this technique.
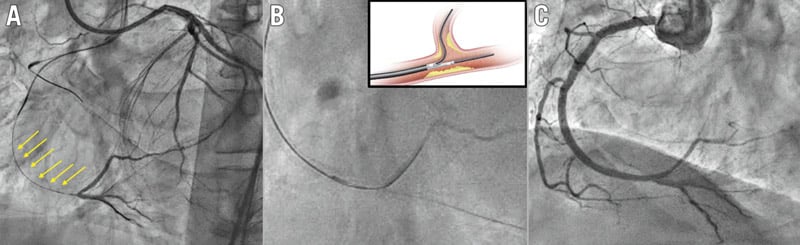
- Dual lumen microcatheters: especially useful for bifurcated CTO lesions, tortuous SB ostial lesions, and tricky bifurcation angles. The whole microcatheter is advanced up to the level of the SB ostium with MV wire within the monorail lumen. The OTW exit port is orientated facing the SB origin, facilitating passage of a second wire towards the SB. Caution: Dual-lumen microcatheters alter the guidewire properties by increasing the penetrative force through added support (Figure 1).
- Dedicated single lumen angulated microcatheters (SuperCross Angled Tip Microcatheter): These catheters tips can be torqued and are most useful for extreme SB angulations, especially Medina X,0,X bifurcation lesions. On the contrary, in Medina X,1,X bifurcation lesions, the orientation of the SuperCross in front of the SB origin can be more complicated because of a lack of space at the level of the SB ostium.
- Deflectable tip single lumen microcatheters (Venture (Teleflex) wire-control catheter): with a success rate ~ 85 % after conventional techniques fail, this microcatheter has radiopaque 8 mm distal tip that can be deflected up to 90º to the desired angle to access SB ostium.
- The balloon block and support technique. Only to be used in cases of significant MV/SB angulation, where microcatheters are unavailable, when the SB guidewire prolapses into the distal MV Once the SB wire reaches SB ostium, The MV balloon is inflated to block the distal MV, thus facilitating wire advancement into SB.
- MV balloon predilation. As the “last resort” strategy, to be used only in unfavourable anatomies, ie. large plaque burden in both the MV and SB, and a wide angle, preventing advancement of any wires/ devices. Gentle predilation of the proximal MV with a small balloon creates enough space to advance and manipulate shaped wires and microcatheters. In severely calcified lesions, MV rotational atherectomy is an alternative. Caution to be applied as this may cause plaque and carina shift, leading to SB occlusion.
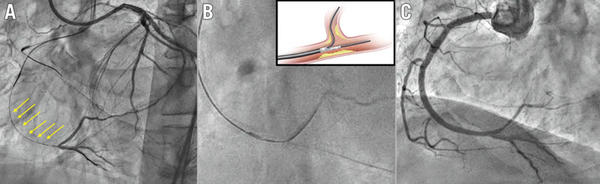
Figure 1. Dual lumen microcatheter in bifurcation lesions associated with CTO. Example of a right coronary artery CTO with a bifurcation at the distal cap and a long proximal dissected segment (arrows). A) Wire into the true lumen of the posterior descending artery. B) Dual lumen microcatheter to pass a new guidewire into the posterolateral branch. C) Final angiographic result after provisional stenting. CTO: coronary chronic total occlusion.
Source: EuroIntervention Journal
SB rewiring after MV stenting in challenging anatomies
SB rewiring can be technically challenging due to the baseline anatomy and/or severity of the stenosis at the SB origin following MV stenting. The most difficult scenario is the obstruction of a highly angulated SB.
The following manoeuvres may help in SB rewiring;
- Leaving a wire in the SB during MV stent implantation (jailed wire technique).
- POT should be performed before SB rewiring to prevent unintentional abluminal wiring outside the stent in the main vessel.
- When SB access is anticipated to be more problematic than MV access, inverted provisional stenting should be considered.
- Predilation of the SB balloon prior to MV stenting. This strategy is not typically recommended, although it may be effective in cases of significantly calcified or angulated side branch stenosis, restricted access to the side branch, or diminished side branch flow after wiring. However, side branch dissection is more prevalent with this method, which may inhibit rewiring and have negative consequences.
SB rewiring through the MV stent struts
With slight modifications, most of the strategies outlined above may be helpful in this scenario. (Central illustration)
- Guidewire tip configuration. For this reason, a single wide-angled bend or a double-bend form appears to be the most preferred options. Pulling the wire back from the distal MV and allowing it to traverse into the SB increases the success rate, and the possibility of distal strut crossing.
- Angulated and deflectable tip catheters maybe more effective than baseline. The large MV lumen produced by the stent allows these catheters to be rotated and manipulated to aim their tip toward the SB ostium. Dual-lumen microcatheters can also help to minimize abluminal wire crossing and ease SB wiring in this situation.
- If an important SB becomes occluded and side branch wiring attempts fail, an initial re-POT should be performed to achieve adequate stent strut expansion, followed by additional recrossing attempts. If these approaches are not successful, a "rescue" balloon can be introduced behind the stent along the jailed wire into the side vessel (Figure 2).
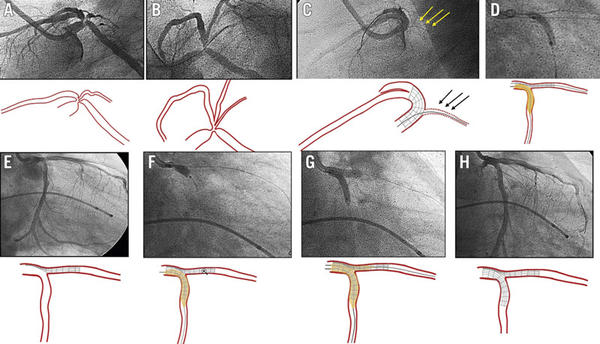
Figure 2. Inverted crush as a rescue technique for acute side branch occlusion. A, B) Baseline angiography, lateral (A) and spider (B) views, showing a severe bifurcation lesion at the distal LM (Medina 1,1,1). C) Acute LCx occlusion after LM-LAD stent implantation. Jailed guidewire at LCx (arrows). D) Abluminal inflation of a balloon at LCx advanced through the jailed wire (after previous low-profile balloon dilation). E) Patent LCx while the stent at the LAD remains crushed. F) DES implantation from LM to LCx artery (inverted crush technique). G) Rewiring of the LAD and final kissing balloon inflation. H) Final angiographic result. DES: drug-eluting stent; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main.
Source: EuroIntervention Journal
SB jailed balloon technique and active SB protection
Burzotta and al. initially described the jailed balloon technique9. During the MV stenting, an uninflated balloon is placed in the SB. After deployment, the uninflated balloon remains behind the MV stent, limiting carina and plaque shifts. If the SB flow is preserved following MV stenting, the uninflated jailed balloon is removed. If the SB is occluded following MV stenting, the SB jailed balloon is inflated to restore SB flow.
Following the original description, additional modifications have been reported, including 1) balloon- stent kissing technique; 2) modified jailed balloon technique; 3) semi-inflated balloon technique; 4) double-kissing inflation outside the stent; 5) jailed Corsair technique (Central illustration).
According to observational studies, all of these jailed SB balloon techniques for complex, true bifurcation lesions provide good, immediate procedural success, excellent SB protection that prevents SB occlusion during the procedure, and good immediate clinical outcome in patients treated with the provisional stenting approach.
The CIT-RESOLVE Trial10 included 335 patients at high risk of SB occlusion who were randomly assigned to either the conventional approach, using the jailed SB wire method, or the SB protection strategy, using the jailed SB balloon. The active SB protection with a jailed balloon technique outperformed the conventional strategy, with a significantly decreased incidence of SB occlusion and loss of SB flow immediately after full apposition of the MV stent.
A subgroup analysis found no significant difference in major adverse cardiac events (MACE) after one year of follow-up. A meta-analysis comparing the two techniques indicated no difference in procedural myocardial infarction or long-term prognosis improvement11.
Conclusion
Side branch occlusion can develop after main vessel stenting, and is not always easy to correct.
Following several EBC meetings, SB protection approaches were discussed and developed in this consensus document, which provides strategies to avoid SB closure or overcome compromise following MV stenting, while minimizing periprocedural injury and ensuring a durable outcome for patients with bifurcation coronary lesions.
To go further...
Join Nicola Ryan and Manuel Pan, one of the EBC members and co-authors of this Consensus, in the corridors of EuroPCR 2023 to discuss the 17th Consensus Statement from the European Bifurcation Club on techniques to preserve access to the side-branch using the stepwise provisional approach.
References
- Pan M, Lassen JF, Burzotta F, Ojeda S, Albiero R, Lefèvre T, Hildick-Smith D, Johnson TW, Chieffo A, Banning AP, Ferenc M, Darremont O, Chatzizisis YS, Louvard Y, Stankovic G. The 17th expert consensus document of the European Bifurcation Club - techniques to preserve access to the side branch during stepwise provisional stenting. EuroIntervention. 2023 15;19(1):26-36.
- Dou K, Zhang D, Xu B, Yang Y, Yin D, Qiao S, Wu Y, Yan H, You S, Wang Y, Wu Z, Gao R, Kirtane AJ. An angiographic tool for risk prediction of side branch occlusion in coronary bifurcation intervention: the RESOLVE score system (Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion). JACC Cardiovasc Interv. 2015;8:39-46.
- Dou K, Zhang D, Xu B, Yang Y, Yin D, Qiao S, Wu Y, You S, Wang Y, Yan R, Gao R, Kirtane AJ. An angiographic tool based on Visual estimation for Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion: the V-RESOLVE score system. EuroIntervention. 2016;11:e1604-11
- Lassen JF, Holm NR, Stankovic G, Lefèvre T, Chieffo A, Hildick-Smith D, Pan M, Darremont O, Albiero R, Ferenc M, Louvard Y. Percutaneous coronary intervention for coronary bifurcation disease: consensus from the first 10 years of the European Bifurcation Club meetings. EuroIntervention. 2014;10:545-60.
- Albiero R, Burzotta F, Lassen JF, Lefèvre T, Banning AP, Chatzizisis YS, Johnson TW, Ferenc M, Pan M, Daremont O, Hildick-Smith D, Chieffo A, Louvard Y, Stankovic G. Treatment of coronary bifurcation lesions, part I: implanting the first stent in the provisional pathway. The 16th expert consensus document of the European Bifurcation Club. EuroIntervention. 2022;18:e362-76.
- Ojeda S, Pan M, Gutiérrez A, Romero M, Chavarría J, de Lezo JS, Mazuelos F, Pardo L, Hidalgo F, Carrasco F, Segura J, Durán E, Ferreiro C, Sánchez JJ, Rodríguez S, Oneto J, de Lezo JS. Bifurcation lesions involved in the recanalization process of coronary chronic total occlusions: Incidence, treatment and clinical implications. Int J Cardiol. 2017;230:432-8.
- Choi YJ, Lee SJ, Kim BK, Hong SJ, Ahn CM, Kim JS, Gwon HC, Kim HS, Chun WJ, Hur SH, Nam CW, Han SH, Rha SW, Chae IH, Jeong JO, Heo JH, Yoon J, Lim DS, Park JS, Cha KS, Kim DI, Lee SY, Chang K, Hwang BH, Choi SY, Jeong MH, Choi KH, Song YB, Hong SJ, Doh JH, Koo BK, Hong MK, Jang Y. Effect of Wire Jailing at Side Branch in 1-Stent Strategy for Coronary Bifurcation Lesions. JACC Cardiovasc Interv. 2022;15:443-55.
- Arunothayaraj S, Lassen JF, Clesham GJ, Spence MS, Koning R, Banning AP, Lindsay M, Christiansen EH, Egred M, Cockburn J, Mylotte D, Brunel P, Ferenc M, Hovasse T, Wlodarczak A, Pan M, Silvestri M, Erglis A, Kretov E, Chieffo A, Lefèvre T, Burzotta F, Darremont O, Stankovic G, Morice MC, Louvard Y, Hildick-Smith D. Impact of technique on bifurcation stent outcomes in the European Bifurcation Club Left Main Coronary Trial. Catheter Cardiovasc Interv. 2023;101:553-62
- Burzotta F, Trani C, Sianos G. Jailed balloon protection: a new technique to avoid acute side-branch occlusion during provisional stenting of bifurcated lesions. Bench test report and first clinical experience. EuroIntervention. 2010;5:809-13.
- Dou K, Zhang D, Pan H, Guo N, Li L, Li Y, Zhang Q, Liu B, Shen Z, Zhang B, Liu J, Han W, Wang Y, Zhao Y, Yang Y, Chen S, Xie L, Guan C, Kirtane AJ, Xu B; CIT-RESOLVE Investigators. Active SB-P Versus Conventional Approach to the Protection of High-Risk Side Branches: The CIT-RESOLVE Trial. JACC Cardiovasc Interv. 2020;13:1112-22.
- Qin Q, Zheng B, Liu J, Zhang B, Chen M, Li J, Huo Y. Active Versus Conventional Side Branch Protection Strategy for Coronary Bifurcation Lesions. Int Heart J. 2021; 62:1241-8.