Evolution and prognostic impact of right ventricular–pulmonary artery coupling after transcatheter aortic valve replacement
Selected in JACC: Cardiovascular Interventions by A. Beneduce , L. Baldetti
The aim of this study was to comprehensively assess the prognostic impact of TAPSE/PASP and its longitudinal variation in AS patients undergoing TAVR.
References
Authors
Maria Chiara Meucci, Silvia Malara, Steele C. Butcher, Kensuke Hirasawa, Frank van der Kley, Antonella Lombardo, Cristina Aurigemma, Enrico Romagnoli, Carlo Trani, Massimo Massetti, Francesco Burzotta, Jeroen J. Bax, Filippo Crea, Nina Ajmone Marsan, and Francesca Graziani
Reference
J Am Coll Cardiol Intv. 2023 Jul, 16 (13) 1612–1621
Published
July 2023
Link
Read the abstract
Reviewers
Our Comment
Why this study? – the rationale/objective
In patients with severe aortic stenosis (AS) undergoing transcatheter aortic valve replacement (TAVR), extending the focus from the evaluation of the aortic valve itself to a broader assessment of extra-valvular involvement portends relevant information.
According to the 5-stage classification of AS-related cardiac damage proposed by Généreux et al. (stage 0, no extra-valvular cardiac damage; stage 1, left ventricular damage; stage 2, left atrial or mitral valve damage; stage 3, pulmonary vasculature or tricuspid valve damage; and stage 4, right ventricular damage), the extent of AS-related cardiac damage at baseline and its change after TAVR have important prognostic implications1.
Given the detrimental effects of the untreated AS disease upon the pulmonary circulation and the right ventricle (RV), the echocardiographic ratio of tricuspid annular plane systolic excursion (TAPSE) to pulmonary artery systolic pressure (PASP) has been proposed as a prognostic marker in this setting2.
The aim of the study by Meucci et al. was to comprehensively assess the prognostic impact of TAPSE/PASP and its longitudinal variation in AS patients undergoing TAVR3.
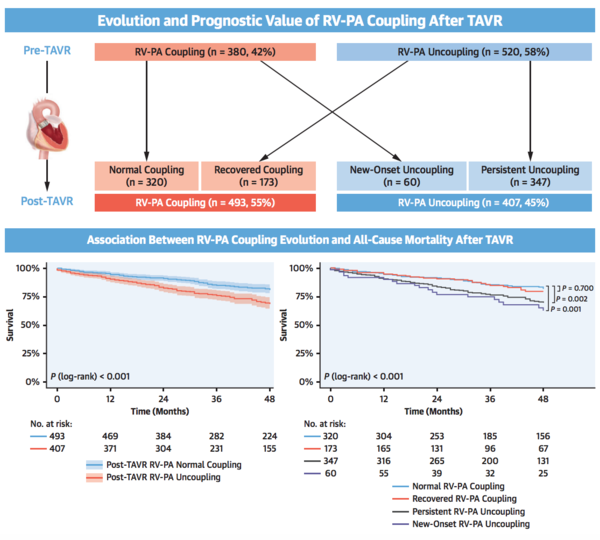
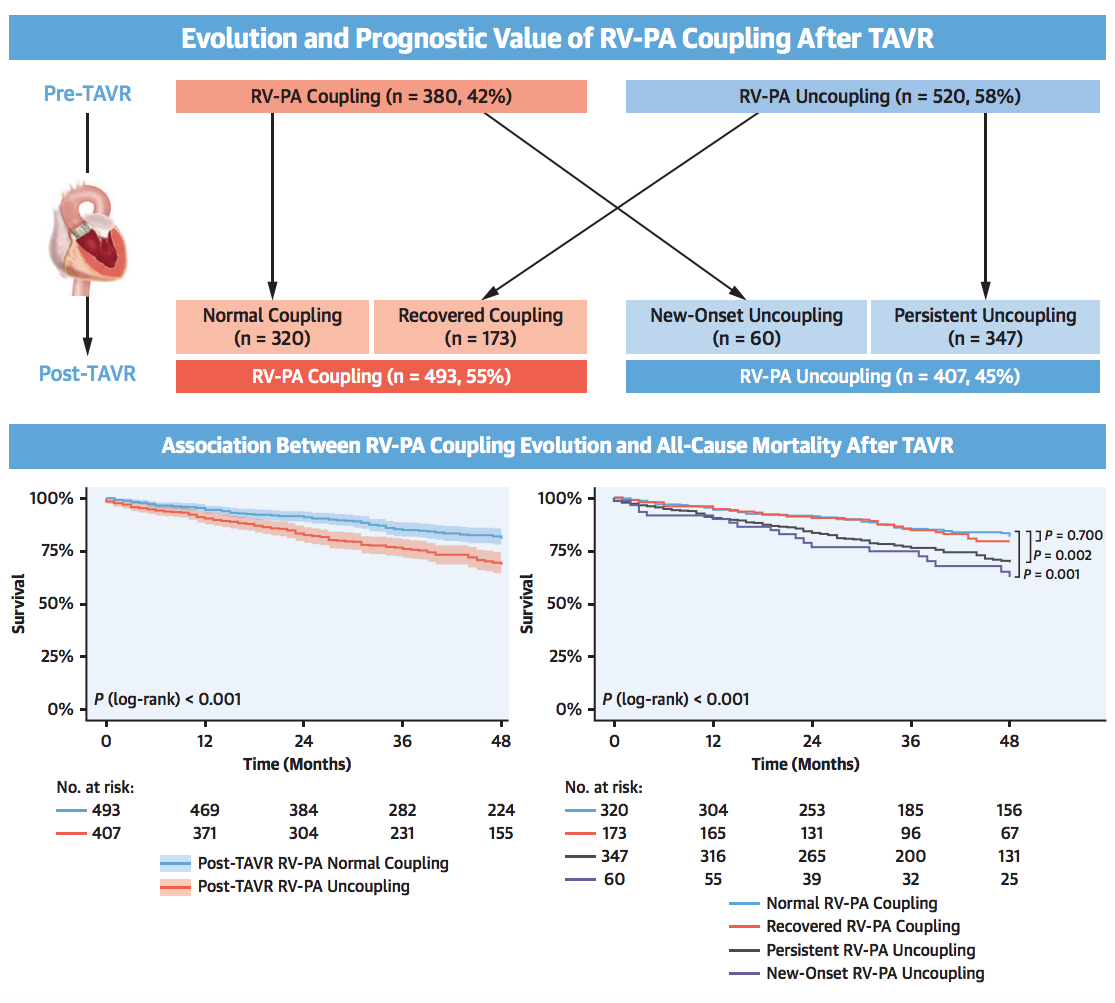
Central Illustration
Study findings and Summary. RV-PA = right ventricular-to-pulmonary artery; TAVR = transcatheter aortic valve replacement.
Source: JACC Cardiovascular Interventions
How was it executed? - the methodology
A total of 900 patients who underwent TAVR in 2 tertiary centers with adequate echocardiographic analysis performed within 3 months before and after the procedure were included.
RV to pulmonary artery (RV-PA) coupling was classified as follows:
- Normal RV-PA coupling: TAPSE/PASP≥0.55,
- RV-PA uncoupling: TAPSE/PASP 0.33-0.54,
- Severe RV-PA uncoupling: TAPSE/PASP <0.32.
The primary endpoint was all-cause mortality. Median follow-up was 40 (24-65) months. Clinical, procedural and echocardiographic characteristics were compared between patients with normal vs abnormal post-TAVR RV-PA coupling. The adjusted prognostic role of pre- and post-TAVR RV-PA coupling was explored by multivariable analysis.
What is the main result?
The study reported several interesting observations.
- At baseline, RV-PA uncoupling was present prior to TAVR in 58 % of AS patients, with severe uncoupling found in 15 % of the entire population and 26 % of the uncoupling group. After TAVR, RV-PA uncoupling was identified in 45 % of patients, with severe uncoupling found in 10 % of cases.
- Regarding the evolution of RV-PA uncoupling, only 19 % of uncoupled patients at baseline actually recovered to normal coupling following TAVR, while 39 % had persistent uncoupling and 7 % new-onset uncoupling.
- Baseline RV-PA uncoupling was not significantly associated with reduced survival. In contrast, post-TAVR RV-PA uncoupling (either persistent or new-onset) was significantly associated with increased mortality at follow-up (adjusted HR: 1.474; 95 % CI: 1.115-1.948; P = 0.006). New-onset RV-PA uncoupling presented the highest hazard ratio for long-term mortality.
- Stratifying the study population according to Généreux classification of AS-related cardiac damage revealed that in stages 0-2 (no overt right heart damage) post-TAVR RV-PA uncoupling was less common (33 % vs 68 %; P < 0.001) although portending an increased rate of mortality (HR: 1.709; 95 % CI: 1.221-2.392; P = 0.002), while in stages 3-4 (overt right heart damage) the association with mortality was observed only for severe RV-PA uncoupling (HR: 1.806; 95 % CI: 1.211-2.694; P = 0.004).
Critical reading and the relevance for clinical practice
The concept of ventricular-arterial coupling (VAC) of the right circulation is based on physiological and physical observations and summarizes:
- the amount of mechanical work transferred from the RV to the pulmonary artery (PA), i.e. mechanical efficiency;
- the amount of energy spent to generate flow across PA, i.e. energetic efficiency;
- the RV ejection fraction at any given loading and inotropic condition4.
VAC is calculated as the ratio of effective arterial elastance (Ea) to end-systolic elastance (Ees), measures attainable only from the pressure-volume plane domain. As a surrogate method, amenable to bedside clinical use, the ratio of TAPSE (index of RV contractility) and PASP (index of RV afterload) has been suggested and validated in several settings5. It is consequential that, in patients with lower TAPSE/PASP ratio, the RV works at an unfavorable hemodynamic and energetic condition, bearing high pressures despite reduced systolic function.
Several previous studies investigated the prognostic role of pre-TAVR TAPSE/PASP ratio with inconsistent findings6,7. In contrast, the present study offers an unique perspective on post-TAVR TAPSE/PASP ratio and affirms its role as a relevant prognostic marker in this setting. These results prompt us to consider systematic assessment of TAPSE/PAPS following TAVR, in order to identify normalization, persistent or new-onset impairment of RV-PA coupling.
The observation that post-TAVR RV-PA uncoupling might provide additional prognostic stratification in patients without overt right heart damage is particularly relevant, as those patients might benefit from tailored medical therapy optimization and close follow-up. Interestingly, the majority of uncoupled patients at baseline persisted with RV-PA uncoupling after TAVR, suggesting that in some cases TAVR may be insufficient to reverse pulmonary overload and RV dysfunction.
Despite some insights emerging from clinical and echocardiographic data (lower left ventricular function, higher prevalence of significant aortic regurgitation, persistent diastolic dysfunction, or moderate or severe mitral and tricuspid regurgitation after TAVR), the clinical phenotype of these patients remains unclear and might also be the consequence of concomitant myocardial or pulmonary disease. Particularly, further efforts should be carried out to understand why some patients experience new-onset RV-PA uncoupling after TAVR.
Finally, the study reminds how the RV is the weak link in the modern era of LV-focused therapies. This should prompt identification of contributing comorbidities (atrial fibrillation, residual valvular disease) and treatments focused on the RV and the pulmonary circulation in patients in whom AS has become advanced and has also involved right heart chambers, as a relevant proportion of these subjects will fail to normalize the VAC following TAVR being exposed to a dismal prognosis.
References
- Généreux P, Pibarot P, Redfors B, Bax JJ, Zhao Y, Makkar RR, Kapadia S, Thourani VH, Mack MJ, Nazif TM, Lindman BR, Babaliaros V, Vincent F, Russo M, McCabe JM, Gillam LD, Alu MC, Hahn RT, Webb JG, Leon MB, Cohen DJ. Evolution and Prognostic Impact of Cardiac Damage After Aortic Valve Replacement. J Am Coll Cardiol. 2022;80:783–800.
- Leurent G, Auffret V, Donal E. Right Ventricular-Pulmonary Artery Coupling: A Simple Marker to Guide Complex Clinical Decisions? JACC Cardiovasc Interv. 2022;15:1834–6.
- Meucci MC, Malara S, Butcher SC, Hirasawa K, van der Kley F, Lombardo A, Aurigemma C, Romagnoli E, Trani C, Massetti M, Burzotta F, Bax JJ, Crea F, Ajmone Marsan N, Graziani F. Evolution and Prognostic Impact of Right Ventricular-Pulmonary Artery Coupling After Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2023;16:1612–21.
- Asanoi H, Sasayama S, Kameyama T. Ventriculoarterial coupling in normal and failing heart in humans. Circ Res. 1989;65:483–93.
- Tello K, Wan J, Dalmer A, Vanderpool R, Ghofrani HA, Naeije R, Roller F, Mohajerani E, Seeger W, Herberg U, Sommer N, Gall H, Richter MJ. Validation of the Tricuspid Annular Plane Systolic Excursion/Systolic Pulmonary Artery Pressure Ratio for the Assessment of Right Ventricular-Arterial Coupling in Severe Pulmonary Hypertension. Circ Cardiovasc Imaging. 2019;12.
- Sultan I, Cardounel A, Abdelkarim I, Kilic A, Althouse AD, Sharbaugh MS, Gupta A, Xu J, Fukui M, Simon MA, Schindler JT, Lee JS, Gleason TG, Cavalcante JL. Right ventricle to pulmonary artery coupling in patients undergoing transcatheter aortic valve implantation. Heart. 2019;105:117–21.
- Cahill TJ, Pibarot P, Yu X, Babaliaros V, Blanke P, Clavel MA, Douglas PS, Khalique OK, Leipsic J, Makkar R, Alu MC, Kodali S, Mack MJ, Leon MB, Hahn RT. Impact of Right Ventricle-Pulmonary Artery Coupling on Clinical Outcomes in the PARTNER 3 Trial. JACC Cardiovasc Interv. 2022;15:1823–33.







No comments yet!