30 May 2023
Infarct‐related artery as a donor of collaterals in ST‐segment–elevation myocardial infarction with concomitant chronic total occlusion: challenge of the double‐jeopardy thesis
Selected in Journal of the American Heart Association by A. Cader , S. R. Khan
This study challenges the double-jeopardy assumption as the main cause of adverse outcome in STEMI with non-IRA CTO, as a collateral origin distal from the acute IRA occlusion was associated with a significantly better prognosis than with a proximal origin.
References
Authors
Matthias Scholz, Thomas Meyer, Lars S. Maier and Karl Heinrich Scholz
Reference
Journal of the American Heart Association. 2023;12:e028115
Published
21 March 2023
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
A concomitant chronic total occlusion (CTO) in a non–infarct-related artery (NIRA) is associated with adverse outcomes in ST-segment–elevation myocardial infarction (STEMI).
Double jeopardy effect: the double-jeopardy effect related to poor outcome in STEMI with CTO in a NIRA has been described where the infarct-related artery (IRA) acts as a donor vessel for collaterals to the CTO, and when this acute IRA occlusion occurs proximal to the collateral branching1.
It is postulated that a sudden interruption of these previously developed collaterals to the CTO pose an acute threat to both the immediate IRA area and the collaterally supplied CTO areas, leading to a larger infarct size.
Aims:
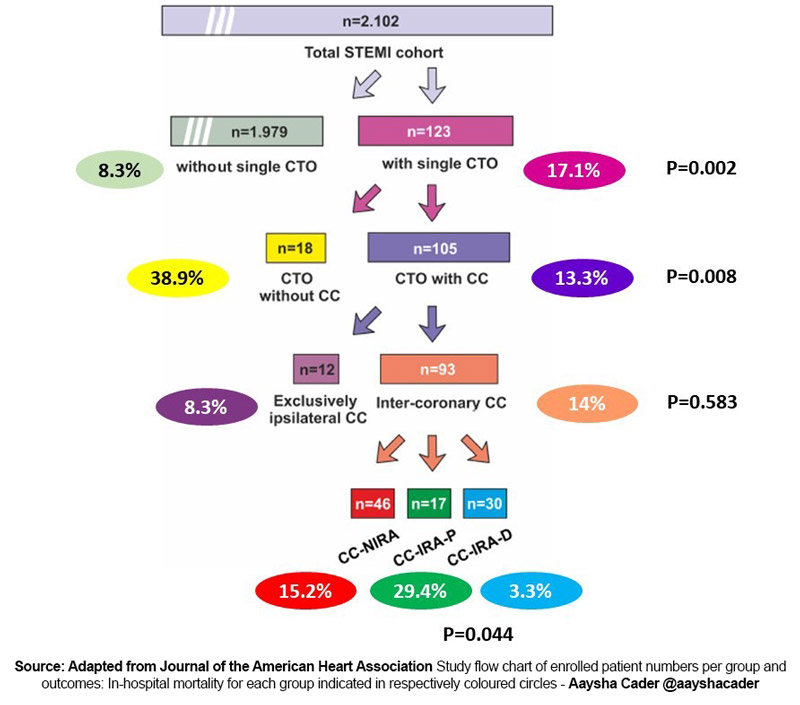
This study2 aimed to analyse the in-hospital mortality rates among STEMI patients with non-IRA CTO comparing outcomes between:
- those with (n = 105) versus without (n = 18) angiographically visible collaterals to the CTO
- those with exclusively ipsilateral collaterals (n = 12) versus intercoronary (n = 93) collaterals
- those with collaterals originating from the IRA (n = 47) versus non-IRA (n = 46) as donor vessels
- among those with collaterals originating from the IRA, collateral origin distal (n = 30) versus proximal (n = 17) to the occlusion
How was it executed? - the methodology
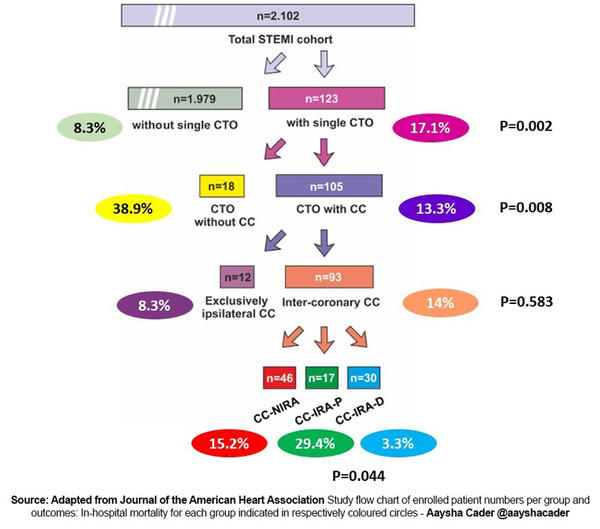
Source: Adapted from Journal of the American Heart Association Study flow chart of enrolled patient numbers per group and outcomes: In-hospital mortality for each group indicated in respectively coloured circles
Design:
This was an observational study with data from 2 hospitals participating in the prospective FITT-STEMI (Feedback Intervention and Treatment Times in ST-Segment Elevation Myocardial Infarction) study.
Population & inclusion criteria:
Among 2,102 STEMI patients undergoing primary PCI, 93 had a single non-IRA CTO with well-developed intercoronary collaterals, which formed the study cohort. Patients with at least a partial collateral filling exceeding a Rentrop grade of 1 were included.
Exclusion criteria:
- Patients with left-main coronary artery occlusion
- Pre-existing coronary artery bypass grafts
- Multiple CTOs due to the additional altered hemodynamics and extremely high early mortality risk
Endpoints:
The main outcome was in-hospital morality. Odds ratios (ORs) and their 95 % CIs for in-hospital mortality were calculated in patients with a collateral to the CTO.
What is the main result?
In-hospital mortality among STEMI patients with a single non-IRA CTO was significantly more than those without a non-IRA CTO (17.1 % vs 8.3 %, p = 0.002).
Mortality was significantly less among non-IRA CTO patients with collaterals to the CTO as compared to those without collaterals (13.3 % versus 38.9 %; p = 0.008).
Among those with intercoronary collaterals, mortality differed significantly with respect to the origin of the collaterals: 15.2 % with collaterals originating from the non-IRA, 29.4 % with a collateral origin from the IRA proximal to the acute STEMI occlusion, and 3.3 % with a collateral origin from the IRA distal to the acute occlusion (P = 0.044).
On multivariate regression analysis a proximal collateral origin had a significantly higher mortality, compared with a collateral origin distal to the acute STEMI occlusion (P = 0.027; odds ratio = 20.8 [95 % CI, 1.4–304.1]).
Previous PCI (OR 31.5) or cardiogenic shock (OR 16.7) were other independent predictors of mortality.
Critical reading and the relevance for clinical practice
This study challenges the double-jeopardy assumption as the main cause of adverse outcome in STEMI with non-IRA CTO, as a collateral origin distal from the acute IRA occlusion was associated with a significantly better prognosis than with a proximal origin2.
The authors hypothesize explanations to this, based on pressure gradients and changes to hypothetical flow patterns following IRA occlusion:
a) in distally arising collaterals, a flow reversal in the pre-existing CTO-IRA collaterals lead to a protective residual perfusion of the acutely infracted area;
b)in proximal origin collaterals, the acute IRA occlusion could lead to an increased blood outflow via the collaterals proximal to the occlusion, thus further depriving the acute infarct area of a blood supply.
These findings also have implications for studies on which subset of patients might benefit from additional CTO PCI, with future studies potentially focusing on collateral status and origin.
This study is limited in that it is a retrospective analysis of a registry, small sample size, challenges in precise visualization of collaterals and main endpoint duration of follow-up limited to in-hospital period.
References
- Claessen BEPM, Dangas GD, Weisz G, Witzenbichler B, Guagliumi G, Möckel M, Brener SJ, Xu K, Henriques JPS, Mehran R, et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur Heart J. 2012;33:768–775. doi:10.1093/eurheartj/ehr471
- Scholz M, Meyer T, Maier LS, Scholz KH. Infarct-Related Artery as a Donor of Collaterals in ST-Segment-Elevation Myocardial Infarction With Concomitant Chronic Total Occlusion: Challenge of the Double-Jeopardy Thesis. J Am Heart Assoc. 2023;12(7):e028115. doi: 10.1161/JAHA.122.028115