23 Mar 2023
A novel breakthrough in wrist-worn transdermal Troponin-I-Sensor assessment for acute myocardial infarction
Selected in European Heart Journal - Digital Health by S. Brugaletta , G. Occhipinti
A transdermal-infrared spectrophotometric sensor (T-ISS) to assess troponins increase has been recently developed. This multicenter, observational study tested the feasibility of implementing this tool with machine learning analytics carried out in a cohort of patients presenting with acute coronary syndrome.
References
Authors
Shantanu Sengupta, Siddharth Biswal, Jitto Titus, Atandra Burman, Keshav Reddy, Mahesh C Fulwani, Aziz Khan, Niteen Deshpande, Smit Shrivastava, Naveena Yanamala, Partho P Sengupta
Reference
https://doi.org/10.1093/ehjdh/ztad015
Published
06 March 2023
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
The diagnosis of acute myocardial injury relies on laboratory findings of elevated levels of cardiac troponin (cTn), exceeding the 99th percentile upper reference limit (URL), and a pattern of rise and/or fall in the cTn levels (delta-troponin). Unfortunately, there are limited standardization protocols and significant variability between emergency departments for the turnover time of blood draws required to calculate the delta-troponin. These constraints may contribute to consistent delays and misinterpretations in diagnosis, which can lead to worse patient outcomes and increased healthcare costs.
Recently, a wrist-worn transdermal-infrared spectrophotometric sensor (T-ISS) has been developed (Figure 1). It measures the infrared absorption corresponding to the troponin-I concentration through the skin, resulting in swifter triage over point-of-care blood testing.
The objective of the study was to test the feasibility of implementing the diagnostic accuracy of the T-ISS with machine learning analytics.

Figure 1. The wrist-worn transdermal-infrared spectrophotometric sensor (T-ISS) prototype2
How was it executed? - the methodology
This is a prospective multicenter observational study, conducted at five different sites, and included 238 patients (150 in the development cohort and 88 in the validation cohort) presenting to the emergency department with acute chest pain suggestive of acute coronary syndrome (ACS), including unstable angina, non-ST-segment and ST-segment elevation myocardial infarction.
The T-ISS was applied to the participants' wrists, and blood samples were collected within 15 minutes for reference troponin-I levels. After unbiased cleaning, the data collected were incorporated into a hybrid convolutional neural network-recurrent neural network (CNN-RNN) model to develop a classifier to identify patients with and without elevated troponin-I levels. The performance and generalizability of the model were further tested using the validation cohorts.
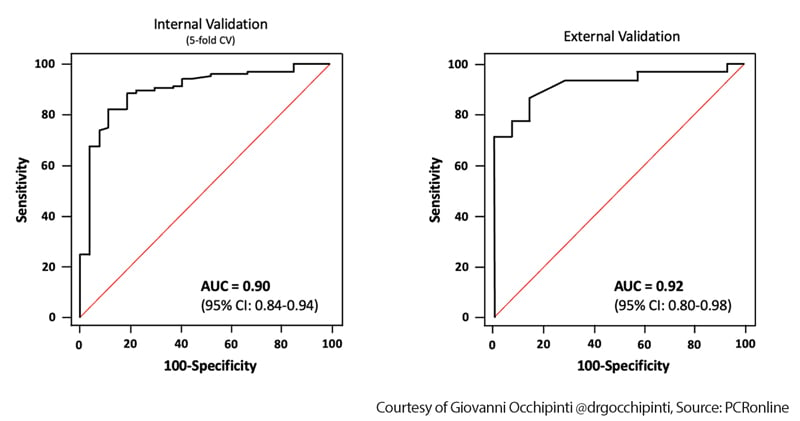
The primary endpoint of training the model was the presence of elevated troponin values, defined as a binary endpoint (elevated vs normal). The trained machine learning model was evaluated using the five-fold cross-validation technique, a powerful tool in machine learning for assessing the performance of a model on a dataset. To describe the algorithm's performance, the authors used visual inspection of a calibration curve, receiver operating characteristic (ROC) curve analysis, and area under the curve (AUC) calculations for statistical analysis.
What is the main result?
- There was an excellent performance on both the training and validation datasets, with an AUC of 0.90 (95 % CI, 0.84-0.94) and 0.92 (95 % CI, 0.80-0.98), respectively (Figure 2).
- The overall model’s performance was not affected by any of the following clinical covariates (age, sex, smoking history, coronary artery disease (CAD), hypertension, diabetes, body mass index, and dyslipidemia), included in the analysis as moderator variables (i.e., influence factors);
- Elevated levels of troponin-I on the T-ISS were significantly associated with an adjusted odds ratio (OR) of 4.69 for obstructive CAD, and also significantly associated with regional wall-motion abnormalities, before and after adjustment for the presence of underlying obstructive CAD (unadjusted OR 3.37; adjusted OR 3.75).
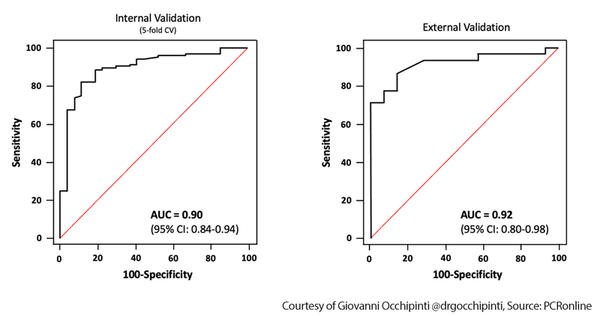
Figure 2. Model performance in the model training and external validation datasets. AUC = area under the curve; CV = cross-validation (Readapted from the original manuscript)
Critical reading and the relevance for clinical practice
The efficient assessment of patients with chest pain, built on evidence-based rapid risk-stratification protocols and standardized sample collection processes is an unmet clinical need1. In this context, the present study represents a preliminary landmark and could potentially lead to a paradigm shift in the way troponin measurements are conducted.
In particular, since the T-ISS device can be worn continuously, it may provide serial assessments, potentially postulating novel algorithms that may supersede the 0/1h and 0/2h rule out algorithms, resulting in a faster and accurate diagnostic assessment.
From the perspective of an interventional cardiologist, obtaining real-time troponin assessments may be beneficial in developing a biomarker-based treatment plan. By integrating specific trends in troponin values with clinical characteristics and a precise troponin curve, different intervention approaches and treatment settings can be set quicker to optimize patient care. This approach may specifically help to identify patients with non-ST segment elevation myocardial infarction who could benefit from early or very-early (less than 2 hours) revascularization, based on evidence of ongoing ischemia or specific short-term troponin trends, instead of relying solely on pain as a feature of “evolving ischemia”.
Continuous monitoring of troponin levels could also help identify potential issues with complex percutaneous coronary intervention techniques, and their relationship with the onset of periprocedural injury and re-infarction and their correlation with long-term prognosis. This could offer new avenues for evaluating the outcomes of certain complex techniques, beyond the endpoints that nowadays we usually consider, often resulting in inconclusive results. Overall, the ability to continuously monitor real-time troponin levels could greatly benefit interventional cardiologists in providing personalized care to their patients.
References
- Sandoval Y, Apple FS, Mahler SA, Body R, Collinson PO, Jaffe AS, International Federation of Clinical C, Laboratory Medicine Committee on the Clinical Application of Cardiac B. High-Sensitivity Cardiac Troponin and the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guidelines for the Evaluation and Diagnosis of Acute Chest Pain. Circulation. 2022;146:569-581. doi: 10.1161/CIRCULATIONAHA.122.059678
- Titus J, Wu AHB, Biswal S, Burman A, Sengupta SP, Sengupta PP. Development and preliminary validation of infrared spectroscopic device for transdermal assessment of elevated cardiac troponin. Commun Med (Lond). 2022;2:42. doi: 10.1038/s43856-022-00104-9