Outcomes of transcatheter aortic valve replacement in patients with cardiogenic shock
Selected in European Heart Journal by M. Alasnag , H. Lichaa
This is the largest real world observational data that confirms the safety and efficacy of TAVR for the treatment of patients with severe aortic stenosis presenting with cardiogenic shock.
References
Authors
Kashish Goel, Pinak Shah, Brandon M Jones, Ethan Korngold, Anju Bhardwaj, Biswajit Kar, Colin Barker, Molly Szerlip, Richard Smalling, Abhijeet Dhoble
Reference
European Heart Journal, ehad387, https://doi.org/10.1093/eurheartj/ehad387
Published
23 June 2023
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
One of the most challenging management decisions in the Cardiac Care Unit (CCU) is that for patients with severe Aortic Stenosis (AS) in the setting of another life-threatening hemodynamic condition which is Cardiogenic Shock (CS). There has been no clear consensus regarding the timing, safety and efficacy of Transcatheter Aortic Valve Replacement (TAVR) in this very ill patient population.
The use of temporizing balloon angioplasty as a bridge to recovery has not been shown to be a great strategy1,2. Taking these very ill patients to the operating room for Surgical Aortic Valve Replacement (SAVR), generally carries very poor outcomes attributed to poor myocardial recovery3. Moreover, the use of Mechanical Circulatory Support (MCS) devices is not only procedurally onerous, but also lacks consensus guidelines owing to insufficient outcome data and high inter-operator practice variability.
Previously published registry data prior to 20174 are not quite representative of today’s practice with regards to the substantial advancements in transcatheter heart valve technology and operator experience. Since this patient population represents 1-4 % of the TAVR patient population3, it is important to study the safety and efficacy of contemporary practice, based on a real-world observational registry.
How was it executed? - the methodology
This is an all-comer registry representing contemporary practice with SAPIEN 3 and SAPIEN 3 ULTRA (Edwards Life Sciences, Irvine, CA), between 2015 and 2022 in the USA. Eligibility for TAVR was left to the discretion of the clinical judgement of the respective Heart Teams.
CS definition included the following:
- Billing code of CS within 24 hours of the procedure
- Pre-procedural use of inotropes
- Pre-procedural use of MCS
The control group included patients without CS. The primary outcome was all-cause mortality at 1 year. Technical and procedural success definitions followed the standard VARC 3 criteria (Valve Academic Research Consortium). Major adverse procedural complications and objective quality of life measures (NYHA and KCCQ OS) were reported at 30 days and 1 year.
A landmark analysis was performed at 30 days. Statistical analysis included the two-sample t-test, Wilcoxon rank sum test, χ2 or Fisher’s exact tests and propensity score analysis to adjust for confounders.
What is the main result?
1.6 % of the studied TAVR patient population had CS. Complete follow-up was achieved in a high percentage of those enrolled (93.03 % at 30 days - 76.86 % at 1 year). Expectedly, in terms of baseline characteristics, the CS group was much sicker; however, after adjustment with propensity score matching, there were only minimal differences between the 2 groups. The most relevant are summarized in Table 1.
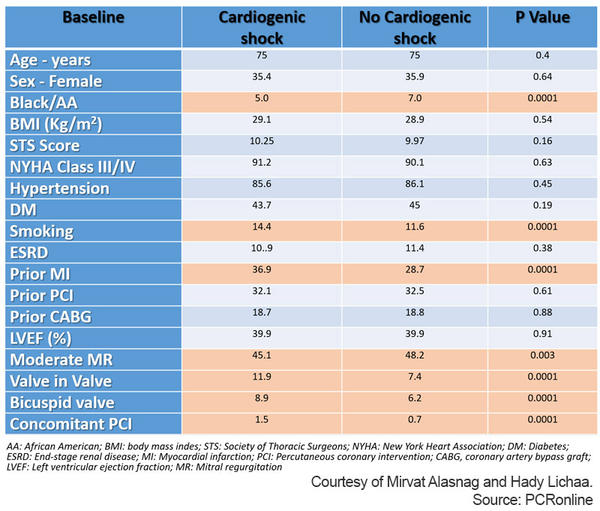
Table 1: Adjusted baseline characteristics of the study populations.
Courtesy of Mirvat Alasnag and Hady Lichaa.
Unsurprisingly, in-hospital mortality was significantly higher in patients with CS compared with no CS. Moreover, the CS group showed significantly higher cardiac death, cerebrovascular events, new dialysis, major vascular complication, life-threatening bleeding, new onset atrial fibrillation, and PCI.
Although procedural success rates were numerically similar between the 2 groups, some procedural outcomes were less optimal in the CS group including conversion to open cardiac surgery and coronary compression or obstruction rate. This may be partly related to the hemodynamic instability of these patients. However, other immediate cardiovascular complications were similar.
On the other hand, technical success (VARC-3 criteria) was 2.2 % lower (P < 0.0001) in the CS group. The rate of 30-day mortality (12.9 % vs. 4.9 %) and stroke (3.2 % vs. 1.9 %) was significantly higher in the CS group. Median length of stay post-TAVR was more than double in the CS group and 20 % less patients went home. Even though adjusted 1-year mortality was significantly higher in the CS group (Figure 1), the landmark analysis showed that this difference was only attributable to the worse CS group outcomes in the first 30 days.

Figure 1: Reported mortality rates in study popoulation.
Courtesy of Mirvat Alasnag and Hady Lichaa.
Critical reading and the relevance for clinical practice
This is the largest real world observational data that confirms the safety and efficacy of TAVR for the treatment of patients with severe aortic stenosis presenting with cardiogenic shock. It is also representative of contemporary practices. Reassuringly, the in-hospital and 30-day mortality after TAVR in patients with CS was lower than those managed conservatively; 9.9 % and 12.9 % and 35 %–70 % respectively5. Although balloon valvuloplasty has gained traction over the years for shocked patients, the in-hospital mortality remained disappointingly high5.
In this study, it is important to note that those who did survive hospital discharge and the first 30 days after the procedure had similar mortality rates to those without CS. The implication here is that co-morbidities are the likely contributors to mortality after 30 days and not the CS per se. It is difficult to understand how shock stage and procedural factors were not predictive of survival. This may in part be due to the observational nature of the study which depended on accurate coding for the data.
Moreover, evaluating the stage of shock and use of mechanical support devices was not expanded in the trial, which may have impact on outcomes, particularly associated vascular access complications. Drivers reported in this study were end stage renal disease, NYHA Class III/IV, presence of an implantable defibrillator, immunocompromised state and peripheral arterial disease. Although the CS group had a higher likelihood of having a recent myocardial infarction (MI) and recent percutaneous revascularization, that did not impact survival which is counterintuitive. A deeper dive into the types of MI and optimal or completeness of revascularization is worth exploring in a randomized dataset.
One must be cautious with the wider application of this study to centers with little expertise in the care of shocked patients and/or TAVR procedures. Moreover, the outcomes reported are limited to the balloon expandable valve, Edwards Sapien, and it would be difficult to assume similar outcomes with other valve self-expanding valves that have higher rates of paravalvular leaks and pacemakers post implantation (both which have been shown to contribute to overall outcomes).
Overall, this trial begs the question: what is the ideal timing for treating severe aortic stenosis and the risk of subsequent cardiogenic shock? What are there triggers for CS in this population that perhaps would prompt a more urgent replacement?
References
- Debry N, Kone P, Vincent F, Lemesle G, Delhaye C, Schurtz G, et al. Urgent balloon aortic valvuloplasty in patients with cardiogenic shock related to severe aortic stenosis: time matters. EuroIntervention 2018;14:e519–e525. https://doi.org/10.4244/EIJ-D-18- 00029.
- Eugene M, Urena M, Abtan J, Carrasco JL, Ghodbane W, Nataf P, et al. Effectiveness of rescue percutaneous balloon aortic valvuloplasty in patients with severe aortic stenosis and acute heart failure. Am J Cardiol 2018;121:746–750. https://doi.org/10.1016/j. amjcard.2017.11.048.
- Hutter AM Jr, De Sanctis RW, Nathan MJ, Buckley MJ, Mundth ED, Daggett WM, Austen WG. Aortic valve surgery as an emergency procedure. Circulation. 1970 Apr;41(4):623-7. doi: 10.1161/01.cir.41.4.623
- Masha L, Vemulapalli S, Manandhar P, Balan P, Shah P, Kosinski AS, et al. Demographics, procedural characteristics, and clinical outcomes when cardiogenic shock precedes TAVR in the United States. JACC Cardiovasc Interv 2020;13:1314–1325. https://doi. org/10.1016/j.jcin.2020.02.033
- Bongiovanni D, Kühl C, Bleiziffer S, Stecher L, Poch F, Greif M, Mehilli J, Massberg S, Frey N, Lange R, Laugwitz KL, Schymik G, Frank D, Kupatt C. Emergency treatment of decompensated aortic stenosis. Heart. 2018 Jan;104(1):23-29. doi: 10.1136/heartjnl-2016-311037. Epub 2017 May 31.









No comments yet!