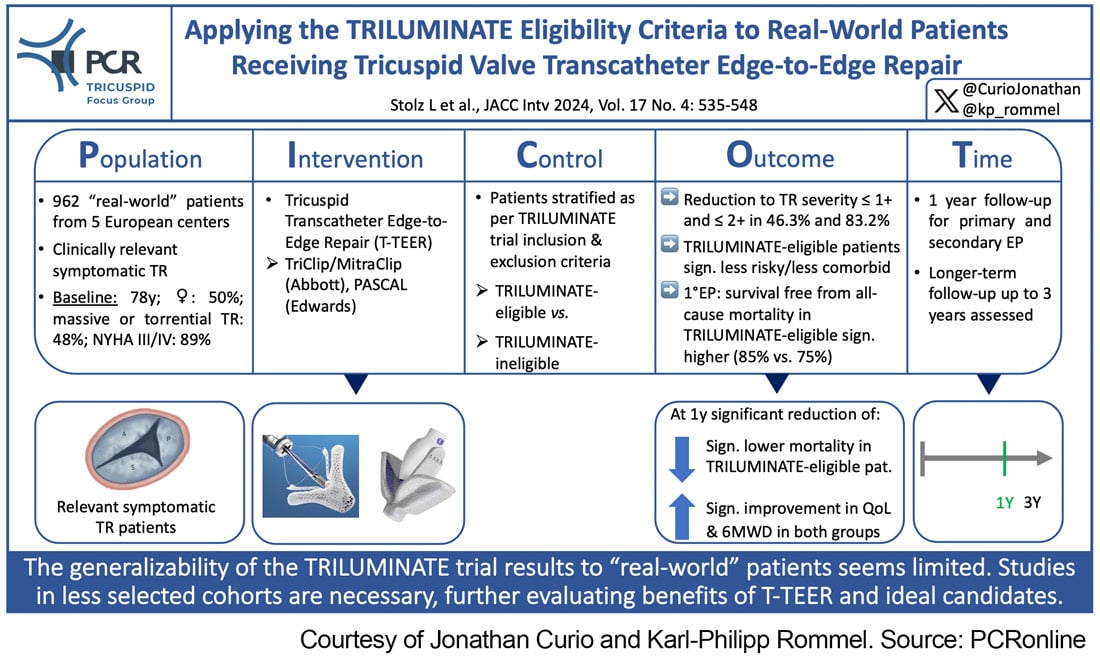
Applying the TRILUMINATE eligibility criteria to real-world patients receiving tricuspid valve transcatheter edge-to-edge repair
Selected in JACC: Cardiovascular Interventions by J. Curio , K. P. Rommel
This study, based on the trial inclusion and exclusion criteria, aimed to compare outcomes in a contemporary “real-world” T-TEER cohort stratified by TRILUMINATE eligibility or ineligibility.
References
Authors
Lukas Stolz, Philipp M. Doldi, Karl-Patrik Kresoja, Sara Bombace, Benedikt Koell, Mohammad Kassar, Johannes Kirchner, Ludwig T. Weckbach, Sebastian Ludwig, Thomas J. Stocker, Hannah Glaser, Anne R. Schöber, Steffen Massberg, Michael Näbauer, Volker Rudolph, Daniel Kalbacher, Fabien Praz, Philipp Lurz, and Jörg Hausleiter
Reference
J Am Coll Cardiol Intv. 2024 Feb, 17 (4) 535–548
Published
February 2024
Link
Read the abstractReviewers
Our Comment
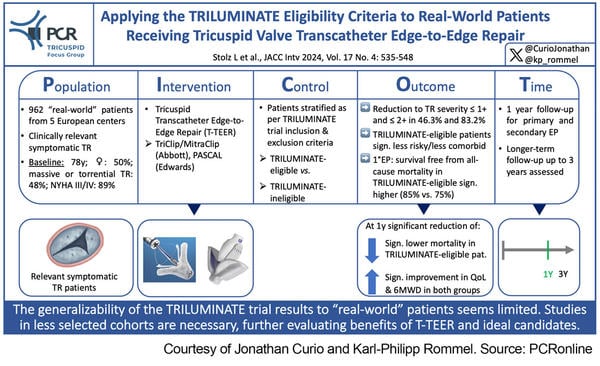
Figure 1: Picot scheme highlighting key aspects of the study.
Courtesy of Jonathan Curio and Karl-Philipp Rommel. Source: PCRonline
Why this study – the rationale/objective?
Transcatheter tricuspid edge-to-edge repair (T-TEER) plays an increasingly important role in the treatment of patients with symptomatic severe tricuspid regurgitation (TR). A first randomized controlled trial comparing T-TEER with medical therapy alone, the TRILUMINATE Pivotal Trial (Clinical Trial to Evaluate Cardiovascular Outcomes In Patients Treated With the Tricuspid Valve Repair System Pivotal, NCT03904147), has reported 1-year outcomes. (1) The trial met its combined hierarchical primary endpoint, with superiority of T-TEER driven by a significant improvement in quality of life as assessed by the Kansas City Cardiomyopathy Questionnaire (KCCQ) score. However, the neutral findings regarding mortality and heart failure hospitalizations have sparked multiple lines of reasoning.
One argument brought forward is that patient cohorts enrolled in randomized trials and patients treated in the actual “real-world” setting often differ significantly, potentially resulting in differing outcomes in these diverging populations. Thus, the present study, based on the trial inclusion and exclusion criteria, aimed to compare outcomes in a contemporary “real-world” T-TEER cohort stratified by TRILUMINATE eligibility or ineligibility.
How was it executed? - the methodology
This observational study assessed 962 consecutive patients treated with T-TEER at 5 experienced European centres, either using the PASCAL (Edwards Lifesciences) or the TriClip/MitraClip (Abbott) system. Inclusion and exclusion criteria of the TRILUMINATE trial were applied to these patients to identify TRILUMINATE-eligible and TRILUMINATE-ineligible subgroups.
Assessed endpoints were:
- Primary endpoint: 1-year survival
- Secondary endpoints: 1-year freedom from heart failure hospitalization (HFH)/TV intervention; change in NYHA class; quality of life; 6-minute walking distance (6MWD)
What is the main result?
Fifty per cent of patients were women, and mean age was 78.3 ± 7.3 years. Most patients suffered from severe TR (50%; 33% massive TR, 15% torrential TR; 2% moderate TR). 89% were in NYHA functional class III/IV.
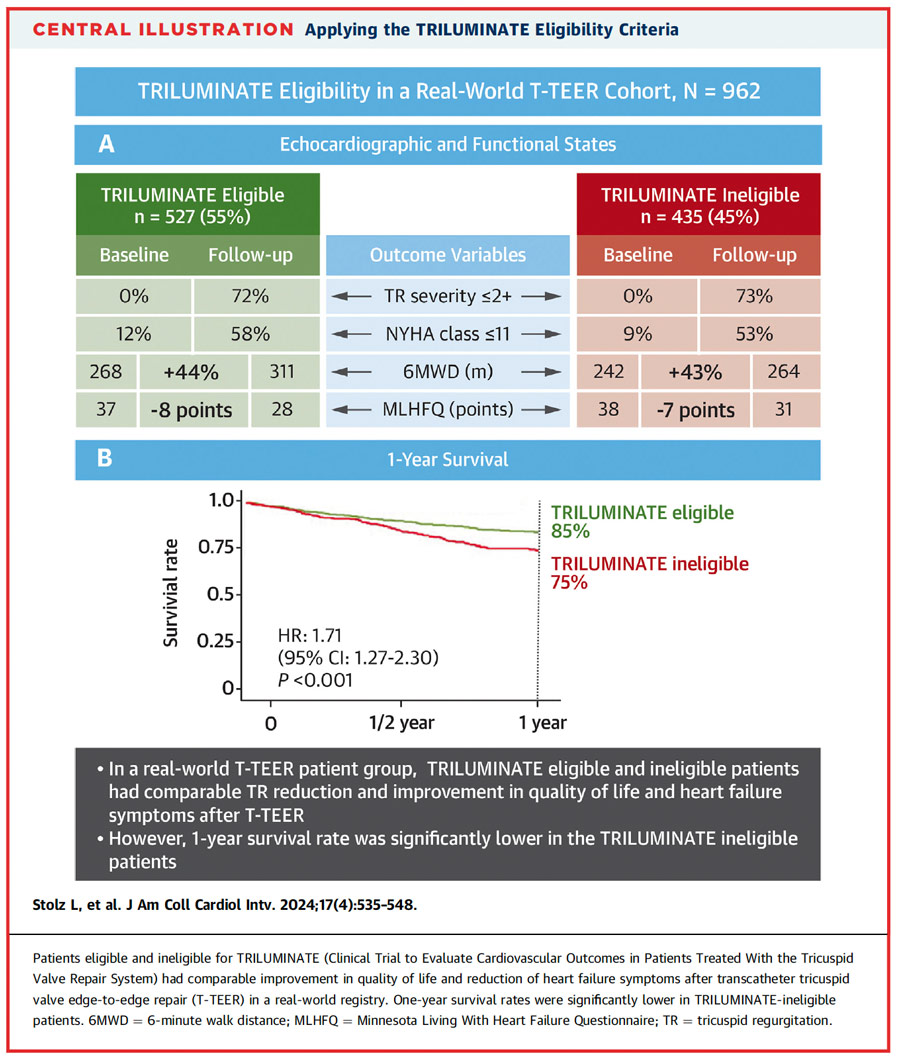
55% of patients were identified as TRILUMINATE-eligible and 45% as TRILUMINATE-ineligible.
- TriClip/MitraClip was used in 60% and PASCAL was used in 40% of patients, mean number of implanted devices was 1.9 ± 0.7, achieving a reduction to TR severity ≤ 1+ and ≤ 2+ in 46.3% and 83.2% of patients, respectively
- TRILUMINATE criteria identified patients with significantly lower surgical risk, less HFH in the year before T-TEER, better exercise capacity, and more preserved liver and kidney function
- Concerning the primary endpoint over-all survival at 1-year was 80.1%, with a significantly higher rate in the TRILUMINATE-eligible patients (84.7% vs. 74.9%. p < 0.001)
- Similarly, survival free from TV surgery, repeat intervention, and HFH was significantly lower in TRILUMINATE-eligible than in -ineligible patients (72.9% vs. 58.0%, p < 0.001)
- Quality of life (as assessed per MLHFQ) was similar at baseline and improved significantly in both groups; 6MWD was higher in TRILUMINATE-eligible patients at baseline, but significantly improved in both groups
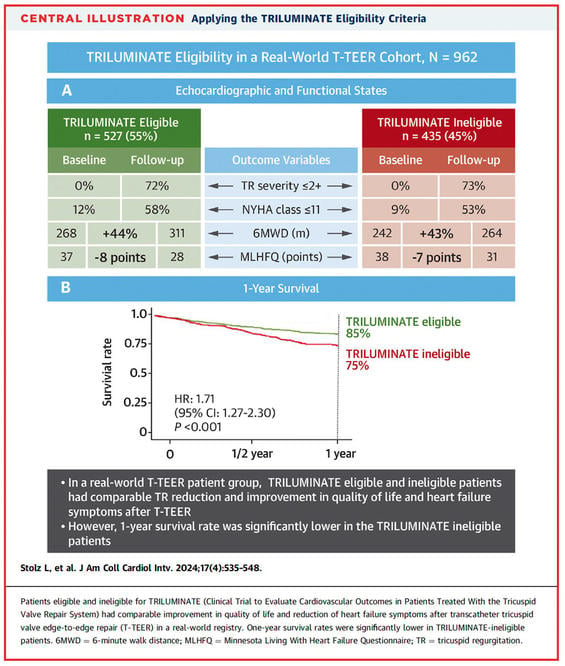
Figure 2
Source: JACC: Cardiovascular Interventions
Critical reading and relevance for clinical practice
This study elegantly demonstrates that patients undergoing T-TEER in clinical practice were at a higher risk compared to those included in the randomized TRILUMINATE trial. They exhibited worse outcomes, thus corroborating the notion a lower-risk cohort had been included in the TRILUMINATE trial. In fact, only roughly half of the real-world patients would have fulfilled TRILUMINATE inclusion criteria. While they tended to have better survival and lower hospitalization rates than patients not fulfilling the inclusion criteria, it is worth noting that they still had almost double the mortality rate and 2.5 times the rate of the mortality/reintervention endpoint compared to the patients in TRILUMINATE. Several reasons might account for this observation:
- TRILUMINATE-eligible patients presented with more advanced left ventricular diseases, evidenced by a lower mean LV-EF, increased LV dilatation, and notably higher PCWP. This suggests significant competing risk in a portion of these patients and a potential diagnostic anchoring bias, where diagnosing the valvular pathology is clinically more straightforward than phenotyping the underlying pathology (e.g., HFpEF).
- Real-world patients were treated over a 6-year period, spanning the very beginnings of therapy in compassionate use programs in clinical practice. This period likely saw an evolution in techniques, devices, and patient selection in clinical practice.
- Real-world patients exhibited a more advanced heart failure stage despite meeting TRILUMINATE criteria, evidenced by a significantly higher hospitalization rate in the prior year, increased dyspnea, and worse RV-PA coupling, despite similar RV dimensions and function. This observation is crucial, as prior matched observations have indicated a prognostic benefit of T-TEER compared to medical therapies in intermediate but not early or late disease stages (2,3).
- Patients in the real-world cohort, despite formally fulfilling TRILUMINATE criteria, did not undergo a committee for anatomical suitability, akin to the approach in the randomized trial. This divergence might account for the more complex TR features observed in the TRILUMINATE-eligible real-world cohort, such as more RV leads, larger coaptation gaps, and less pure functional TR. Consequently, this likely led to a lower rate of sustained TR reduction at one year. Within the TRILUMINATE trial, patients meeting inclusion criteria but not anatomical suitability criteria were treated in a non-randomized single-arm study. Patients in the single-arm study also displayed higher rates of RV leads, larger coaptation gaps, and less pure functional TR compared to their randomized counterparts. Intriguingly, the extent of TR reduction and mortality closely resembled the findings of the TRILUMINATE-eligible real-world cohort (4).
Importantly, T-TEER resulted in robust and significant functional and symptomatic improvements across all discussed groups, including real-world patients regardless of their TRILUMINATE eligibility.
In conclusion, this study underscores the currently still unclear precise criteria for futility in selecting patients for T-TEER, while highlighting that the procedure likely offers symptomatic benefits across various patient cohorts. Additionally, it supports the argument for a potential sweet spot for prognostic benefit of T-TEER, as it confirms that randomized TRILUMINATE patients were at low risk, whereas in real-world practice, event rates and consequently the reduction potential are much higher. Lastly, it indirectly emphasizes the importance of optimally diagnosing and treating concomitant left-sided heart failure to optimize hard outcomes.
References
- Sorajja P, Whisenant B, Hamid N, Naik H, Makkar R, Tadros P et al. Transcatheter Repair for Patients with Tricuspid Regurgitation. N Engl J Med 2023;Online ahead of print.
- Dreyfus J, Galloo X, Taramasso M, Heitzinger G, Benfari G, Kresoja KP et al. TRI-SCORE and benefit of intervention in patients with severe tricuspid regurgitation. Eur Heart J 2024;45:586-597.
- Schlotter F, Miura M, Kresoja KP, Alushi B, Alessandrini H, Attinger-Toller A et al. Outcomes of transcatheter tricuspid valve intervention by right ventricular function: a multicentre propensity-matched analysis. EuroIntervention 2021;17:e343-e352.
- Adams DH et al., TRILUMINATE Pivotal: Outcomes of All Randomized and the Single-arm Subjects with Transcatheter Tricuspid Valve Edge-to-Edge Repair for Tricuspid Regurgitation. Presented at TCT 2023, San Francisco, California, USA.







No comments yet!