Prediction of mortality and heart failure hospitalization after transcatheter tricuspid valve interventions: Validation of TRISCORE
Selected in JACC: Cardiovascular Interventions by F. Bargagna
This study highlights the TRISCORE's role in assessing risk for patients undergoing TTVI. Despite limitations, TRISCORE effectively identifies high-risk patients, aiding decision-making in a complex landscape of valvular heart disease management.

References
Authors
Joerg Hausleiter, Dominique Himbert, Daniel Kalbacher, Edwin Ho, Azeem Latib, Edith Lubos, Sebastian Ludwig, Laura Lupi, Philipp Lurz, Vanessa Monivas, Georg Nickenig, Daniela Pedicino, Giovanni Pedrazzini, Alberto Pozzoli, Denise Pires Marafon, Roberta Pastorino, Fabien Praz, Joseph Rodes-Cabau, Christian Besler, Anne Rebecca Schöber, Joachim Schofer, Andrea Scotti, Kerstin Piayda, Horst Sievert, Gilbert H.L. Tang, Alessandro Sticchi, David Messika-Zeitoun, Holger Thiele, Florian Schlotter, Ralph Stephan von Bardeleben, John Webb, Julien Dreyfus, Stephan Windecker, Martin Leon, Francesco Maisano, Marco Metra, and Maurizio Taramasso
Reference
J Am Coll Cardiol Intv. 2024 Apr, 17 (7) 859–870
Published
April 2024
Link
Read the abstractReviewer
My Comment
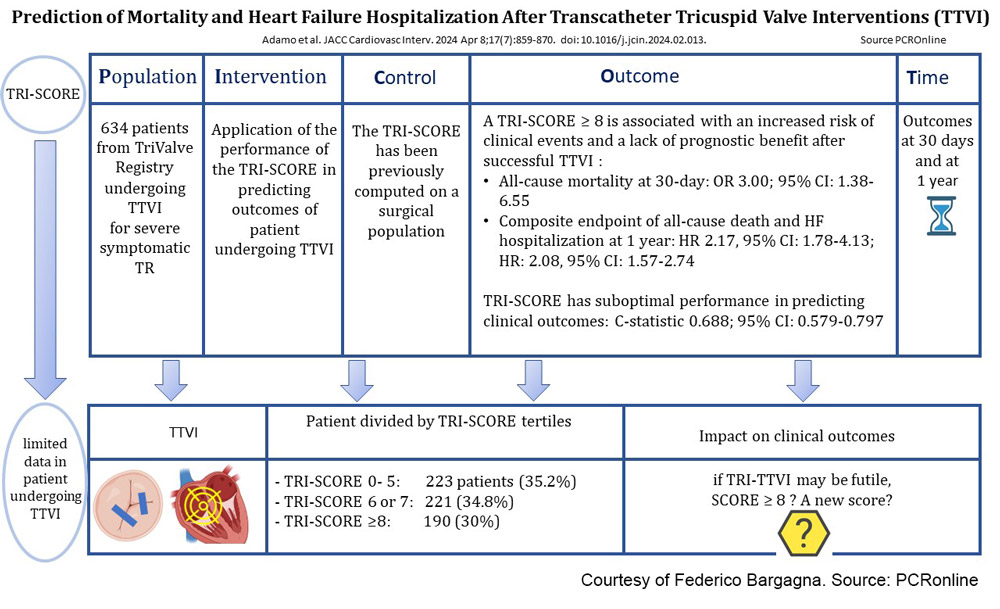
Figure 1: Picot scheme highlighting key aspects of the study.
Courtesy of Federico Bargagna. Source: PCRonline
Why this study? – the rationale/objective
The TRI-SCORE is a risk model initially devised to predict in-hospital mortality after isolated tricuspid valve surgery. This study aimed to evaluate the TRI-SCORE's efficacy in predicting outcomes for patients undergoing transcatheter tricuspid valve intervention (TTVI), as data on this application is limited. The goal was to validate the TRI-SCORE within the context of TTVI and to refine patient selection and risk stratification processes.
How was it executed? - the methodology
This study analyzed data from the TriValve Registry, which included patients who underwent TTVI from 2010 to 2022 across 24 European and U.S. centres. The TRI-SCORE was calculated for each patient, and the population was stratified into tertiles, (0-5, 6-7, ≥8).The outcomes of interest included:
- All-cause death at 30 days
- All-cause death and heart failure hospitalization at one year.
The performance of TRI-SCORE was assessed for its predictive value of these outcomes.
What is the main result?
Among 634 patients included in the study, 223 patients (35.2%) had a TRI-SCORE between 0 and 5, 221 (34.8%) 6 or 7, and 190 (30%) > 8 points. TRI-SCORE tertiles were directly associated with clinical outcomes.
- Patients with a TRI-SCORE of 8 or higher had a 30-day all-cause mortality rate of 8.2% (OR: 3.00; 95% CI: 1.38-6.55; P = 0.006), compared to 2.4% and 3.4% of those with lower scores (0-5 and 6-7, respectively).
- At a median follow-up of 186 days, the high TRI-SCORE tertile demonstrated a higher incidence of composite endpoints, which include all-cause death or heart failure hospitalization, with a rate of 57.8% vs 36.2% and 33.3% (P < 0.001).
- A TRI-SCORE >8 was associated with a 2-fold increased risk of a composite of all-cause death or HF hospitalization (HR: 2.08, 95% CI: 1.57-2.74) after adjustment for procedural success and EuroSCORE II or STS-PROM.
- The TRI-SCORE demonstrated modest discrimination in predicting 30-day mortality with a C-statistic of 0.688 and optimal threshold of 8, resulting in 44% sensitivity and 88% specificity. Over a 1-year period, it overpredicted mortality and hospitalization, showing a Harrell C index of 0.658 for all-cause death and 0.608 for death combined with heart failure hospitalization.
- The TRI-SCORE's calibration and discrimination were inadequate, underscoring the need for new, specific risk models for patients undergoing transcatheter procedures.
Critical reading and relevance for clinical practice
This study adds important additional data regarding the use of the TRI-SCORE in patients undergoing TTVI. These findings suggest that while the TRI-SCORE has limitations in predicting events at 30 days and one year, it effectively identifies patients at greater risk of adverse events post-TTVI.
While transcatheter valve interventions (TVI) have revolutionized the management of valvular heart diseases, the identification of patients who would derive the most benefit from TVI remains complex. Unlike the relatively straightforward decisions in aortic valve replacement, where surgical risk scores like the STS-PROM and EuroSCORE are established predictors, TTVI for severe tricuspid regurgitation (TR) demands consideration of several factors beyond the mere technical feasibility of the procedure.
The TRI-SCORE, tailored for TR, provides a more nuanced assessment by integrating clinical, biological, and echocardiographic parameters. However, the TRI-SCORE may overestimate the risk of postprocedural clinical events, albeit being superior at predicting outcomes compared to traditional surgical scores. Interestingly, the TRISCORE validation in TTVI underscores an elevated risk associated with a TRI-SCORE ≥8, despite procedural success. Furthermore, the benefit of TTVI appears to be limited to patients with a TRI-SCORE <8, raising questions about the intervention's futility in those with higher scores.
In clinical practice, the TRI-SCORE can be a double-edged sword. On one hand, it aids in stratifying patients and avoiding interventions likely to be futile. On the other, it could potentially deny beneficial interventions to a subset of high-risk patients who might still experience symptom relief post-TTVI. The optimal patient candidacy in TTVI remains a challenge and we need for randomized clinical trials to discern the true efficacy of TTVI across the spectrum of TRISCORE. Until then, heart team evaluation probably represents the best assessment due to the synergistic opinion of interventionists, heart failure specialists, electrophysiologists, imaging experts, and cardiac surgeons, encouraging to deliberate beyond numbers and consider the holistic clinical narrative of patients with severe TR.
The take-home message for clinicians is to not view the TRI-SCORE as a determinant of futility but rather as a component of a multifaceted decision-making tool. It serves as a reminder that while risk scores inform clinical decisions, they must be contextualized within the broader clinical picture of each individual patient.




No comments yet!