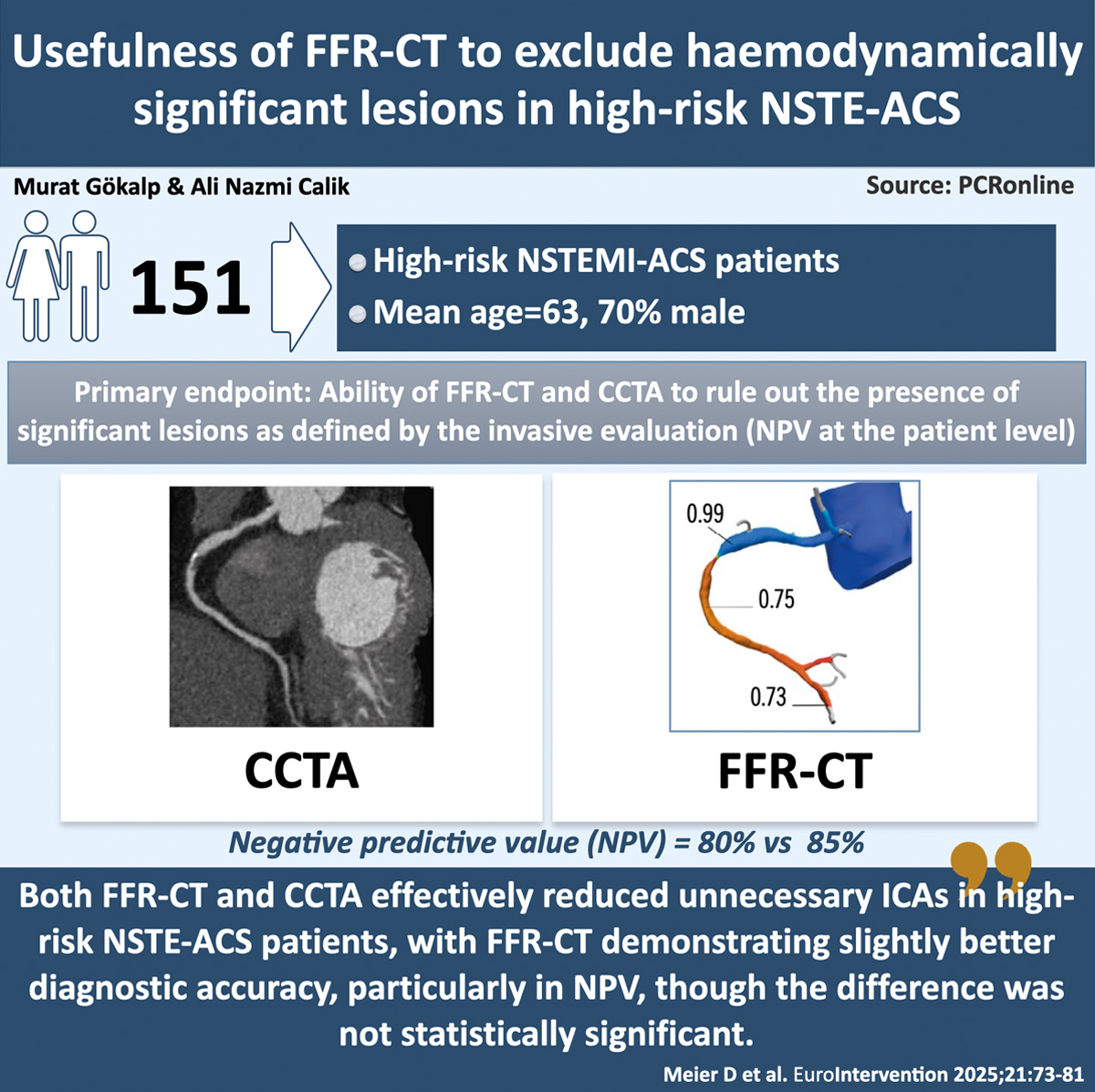
Usefulness of FFR-CT to exclude haemodynamically significant lesions in high-risk NSTE-ACS
Selected in EuroIntervention Journal by A. N. Calik , M. Gökalp
This single-arm, double-blinded, core-laboratory adjudicated, prospective trial, conducted across four European centers between August 2019 and April 2022, investigates whether CCTA and FFR-CT are able to exclude hemodynamically significant coronary stenoses in patients with high-risk NSTE-ACS.
References
Authors
David Meier, Daniele Andreini, Bernard Cosyns, Ioannis Skalidis, Tatyana Storozhenko, Thabo Mahendiran, Emilio Assanelli, Jeroen Sonck, Bram Roosens, David C. Rotzinger, Salah Dine Qanadli, Georgios Tzimas, Olivier Muller, Bernard De Bruyne, Carlos Collet, Stephane Fournier
Reference
DOI: 10.4244/EIJ-D-24-00779
Published
Jan 6, 2025
Link
Read the abstractReviewers
Our Comment
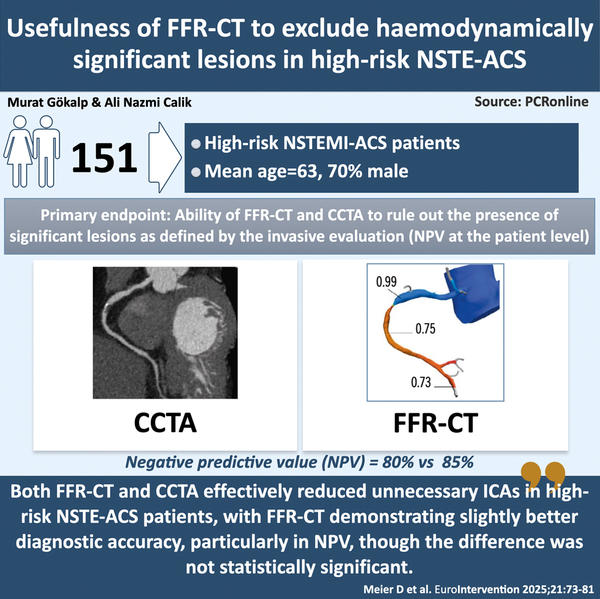
Designed by Murat Gökalp & Ali Nazmi Calik - Source: PCRonline
Why this study – the rationale/objective?
Diagnosing non-ST-elevation acute coronary syndrome (NSTE-ACS) is challenging, as clinical assessment and ECG findings alone are often insufficient. Mildly elevated high-sensitivity troponin (hs-Tn) levels can reduce diagnostic accuracy, leading to unnecessary invasive coronary angiography (ICA). Studies show that up to 50 % of patients with troponin elevations ≤ 3 x the upper reference limit (URL) have no significant epicardial stenosis1.
Coronary CT angiography (CCTA) effectively rules out significant coronary artery disease in low- to intermediate-risk chest pain, while FFR-CT helps assess intermediate lesions in stable cases2. However, their role in high-risk, troponin-positive NSTE-ACS remains unexplored.
This study evaluated the ability of CCTA and FFR-CT to rule out hemodynamically significant coronary stenoses in high-risk NSTE-ACS patients.
How was it executed – the methodology?
From August 2019 to April 2022, four European centers enrolled patients with ischemic symptoms and high-sensitivity troponin T (hs-TnT) levels above the 99th percentile. High-risk NSTE-ACS was defined by troponin elevation with dynamic changes and ischemic symptoms per American and European guidelines3,4.
High-risk NSTE-ACS patients who consented underwent CCTA followed by ICA within 24 hours per guidelines. A lesion was considered significant if QCA showed > 50 % stenosis. Blinded investigators analysed FFR-CT in a central lab, defining hemodynamically significant lesions as FFR-CT ≤ 0.80. FFR was measured for lesions with ≥ 30 % stenosis using the PressureWire X (Abbott), with hyperemia induced by intracoronary adenosine (100 μg for RCA, 200 μg for LCA). In ICA, lesions with FFR ≤ 0.80 were deemed hemodynamically significant.
The primary endpoint was the ability of FFR-CT and CCTA to rule out the presence of significant lesions as defined by the invasive evaluation (i.e., the negative predictive value [NPV] at the patient level). Secondary endpoints were the sensitivity, specificity, positive predictive value (PPV), and accuracy of FFR-CT and CCTA compared to the invasive evaluation at the patient level.
What is the main result?
The study included 168 high-risk NSTE-ACS patients, with 17 excluded due to insufficient CCTA and FFR-CT data, leaving 151 for analysis. The mean age was 63 ± 12 years, 70 % were male, and the median hs-TnT level at 1 hour was 5.3 times the URL (IQR: 1.8-18.6).
Among 151 patients, 99 (66 %) had at least one significant lesion (stenosis > 90 % or 30–90 % with FFR ≤ 0.80). The remaining 52 (34.4 %) had no significant stenosis or lesions with FFR > 0.80. FFR was measured in 106 lesions across 68 patients (45 %). Most had 1-vessel (34.4 %) or 2-vessel disease (44.4 %). Post-ICA, 64 % underwent PCI, 33 % received conservative management, and 3 % were referred for CABG.
FFR-CT showed a higher negative predictive value (NPV) than CCTA (85 % vs. 80 %) for ruling out significant lesions. Similar trends were seen in sensitivity (94 % vs. 93 %), specificity (63 % vs. 54 %), PPV (85 % vs. 80 %), and accuracy (83 % vs. 79 %), though the differences were not statistically significant (p = 0.58).
Misclassification rates varied by strategy. Guideline-based approaches led to 34 % unnecessary ICAs, while CCTA- and FFR-CT-based strategies reduced this to 21 % and 17 % (p < 0.01). Potentially avoidable ICAs were 19 % with CCTA and 22 % with FFR-CT.
Overall, FFR-CT outperformed CCTA due to higher specificity. In ROC analysis, AUC for FFR-CT was significantly greater (0.85 vs. 0.64; p < 0.01). Though FFR-CT had slightly lower sensitivity (83 % vs. 87 %), it showed better specificity (81 % vs. 70 %), PPV (67 % vs. 56 %), and accuracy (82 % vs. 75 %).
Critical reading and the relevance for clinical practice
This study comparing FFR-CT and CCTA in high-risk NSTE-ACS patients found both methods effectively reduced unnecessary ICA. FFR-CT showed slightly better diagnostic accuracy, especially in NPV, though the difference was not statistically significant. At the vessel level, FFR-CT significantly outperformed CCTA.
A significant number of patients had no obstructive coronary artery disease, raising concerns about the effectiveness of current diagnostic methods. Despite meeting guidelines for early invasive strategies (within 24 hours), over one-third of these patients showed no actionable coronary cause for their symptoms. In the present study, the use of CCTA or FFR-CT would have avoided between 54 % and 64 % of unnecessary invasive assessments.
CCTA has been studied as a diagnostic tool in various populations. A meta-analysis of 9 studies (n = 1,349 patients) showed that CCTA had a high negative predictive value for excluding ACS in chest pain patients5. However, no studies have directly compared CCTA and FFR-CT with invasive FFR in this high-risk population. Furthermore, none have systematically assessed the performance of CCTA and FFR-CT relative to FFR, the invasive gold standard, in such a high-risk group.
In the present patient population, as in previous studies, FFR-CT demonstrated enhanced specificity and effectiveness in identifying significant lesions further reducing the number of patients undergoing unnecessary invasive evaluations. For patients requiring ICA, using an FFR-CT-based strategy beforehand can streamline the evaluation. By assessing the haemodynamic significance of coronary lesions, FFR-CT may reduce or eliminate the need for additional invasive FFR measurements.
The study's limitations include a small sample size, as patients with low GFR, prior PCI/CABG, and severe heart failure were excluded, resulting in a selected population. While the focus was on physiological assessment, the potential benefit of intravascular imaging, which could detect plaque erosion or rupture in non-FFR-significant lesions, was not explored.
In conclusion, FFR-CT provides superior diagnostic accuracy compared to CCTA in high-risk NSTE-ACS, offering enhanced specificity and positive predictive value at the lesion level. This indicates that FFR-CT could help reduce unnecessary invasive procedures by more accurately identifying patients who require further intervention.
References
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40:237-69.
- DISCHARGE Trial Group; Maurovich-Horvat P, Bosserdt M, Kofoed KF, Rieckmann N, Benedek T, Donnelly P, Rodriguez-Palomares J, Erglis A, Štěchovský C, Šakalyte G, Čemerlić Adić N, Gutberlet M, Dodd JD, Diez I, Davis G, Zimmermann E, Kępka C, Vidakovic R, Francone M, Ilnicka- Suckiel M, Plank F, Knuuti J, Faria R, Schröder S, Berry C, Saba L, Ruzsics B, Kubiak C, Gutierrez-Ibarluzea I, Schultz Hansen K, Müller- Nordhorn J, Merkely B, Knudsen AD, Benedek I, Orr C, Xavier Valente F, Zvaigzne L, Suchánek V, Zajančkauskiene L, Adić F, Woinke M, Hensey M, Lecumberri I, Thwaite E, Laule M, Kruk M, Neskovic AN, Mancone M, Kuśmierz D, Feuchtner G, Pietilä M, Gama Ribeiro V, Drosch T, Delles C, Matta G, Fisher M, Szilveszter B, Larsen L, Ratiu M, Kelly S, Garcia Del Blanco B, Rubio A, Drobni ZD, Jurlander B, Rodean I, Regan S, Cuéllar Calabria H, Boussoussou M, Engstrøm T, Hodas R, Napp AE, Haase R, Feger S, Serna-Higuita LM, Neumann K, Dreger H, Rief M, Wieske V, Estrella M, Martus P, Dewey M. CT or Invasive Coronary Angiography in Stable Chest Pain. N Engl J Med. 2022;386:1591-602.
- Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, Claeys MJ, Dan GA, Dweck MR, Galbraith M, Gilard M, Hinterbuchner L, Jankowska EA, Jüni P, Kimura T, Kunadian V, Leosdottir M, Lorusso R, Pedretti RFE, Rigopoulos AG, Rubini Gimenez M, Thiele H, Vranckx P, Wassmann S, Wenger NK, Ibanez B; ESC Scientific Document Group. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44:3720-3826.
- Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ; ACC/AHA Task Force Members; Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:2354-94.
- Samad Z, Hakeem A, Mahmood SS, Pieper K, Patel MR, Simel DL, Douglas PS. A meta-analysis and systematic review of computed tomo- graphy angiography as a diagnostic triage tool for patients with chest pain presenting to the emergency department. J Nucl Cardiol. 2012;19:364-76.





No comments yet!