14 Nov 2019
About a complex clinical decision...
Euro4C Case
Author
Let’s exchange opinions on this case. This could happen to you tomorrow…
Case presentation
- 79-year-old B.V. male, active farmer
- Begining 2018: important weight loss; increment of hepatic GGT
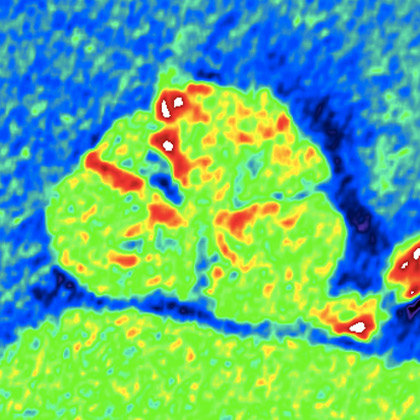
- June 2018: Echo-abdominal shows big hepatic mass (20 cm) confirmed at MRI
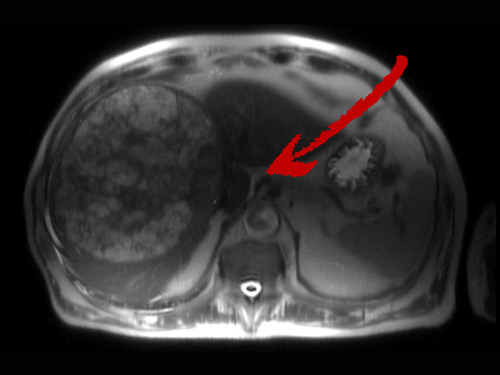
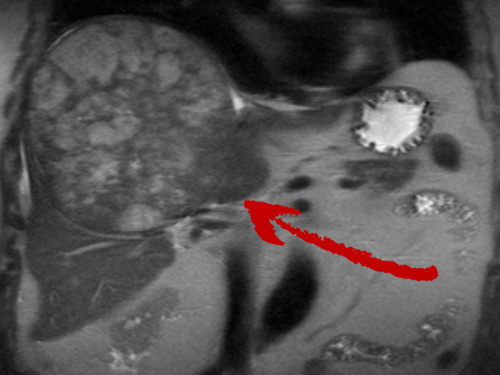
Bioptic diagnosis: Hepatocarcinoma
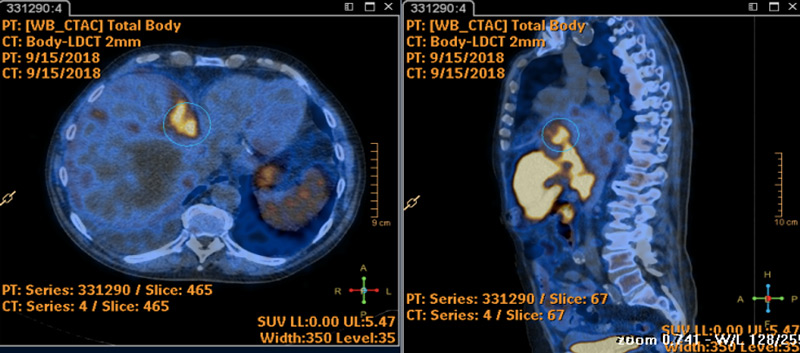
PET-TC with coline: no methastasis → Candidate to surgery of the hepatocarcinoma
Pre-operative cardiovascular work-up: severe AVS, mild mitral regurgitation and AF under oral anticoagulation

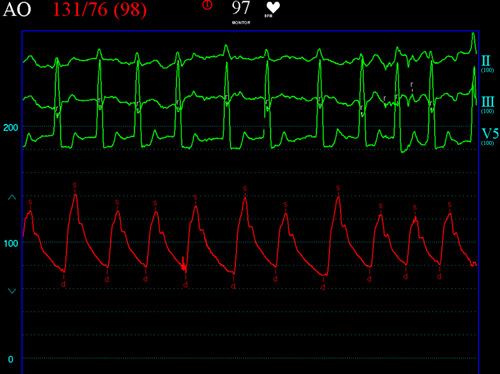
Echocardiogram: preserved EF and severe AVS: mean gradient 53mmHg
The abdominal intervention is formally contra-indicated
- November 2018: Oncologic team evaluation: indication to radical surgery → Need for TAVI
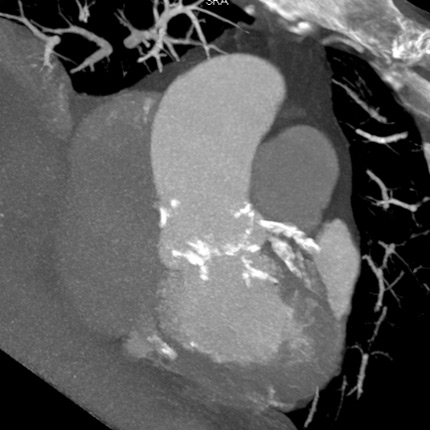
- 20 November 2018: angio TC pre-TAVI
- December 2018: admitted in Cardiology for TAVI
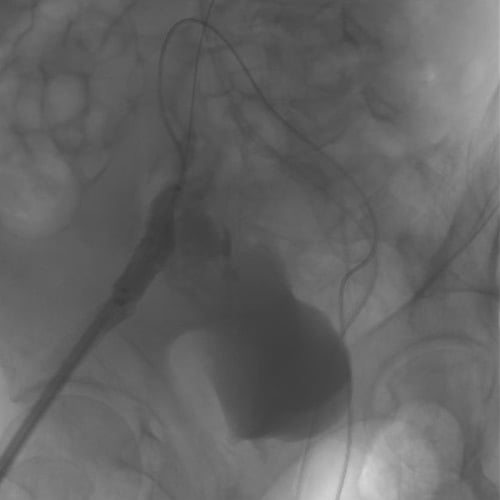
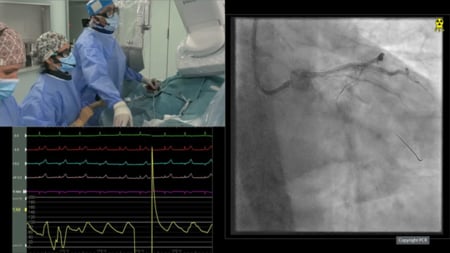
Coronary angiogram pre-TAVI performed in the same procedure shows very calcified CAD with sub-occlusive LAD stenosis at the proximal segment.
Need for PCI…?
What would you do?
- Perform PCI and defer TAVI (one week or one month later)
- Perform PCI before TAVI in the same procedure
- Perform TAVI and then PCI in the same procedure
- Perform TAVI and defer PCI (one week or one month later)
- Perform aortic balloon valvuloplasty and PCI and consider TAVI at a later stage.
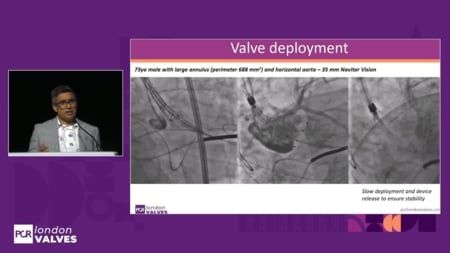
TAVI (Corevalve Evolut R 34 mm)
Replacement of OAC with UFH INR 1,7 the day of the procedure


Vascular access: right femoral prepared with pre-implantation of 2 proglides
Excellent hemodynamic result of the valve implantation
Immediately after TAVI: catheterisation of the left main with guiding catheter EBU 3.5 6 french, but rapid hypotension…
STOP PCI → Intra-procedural bleeding?
Severe iliac bleeding: covered stent and stop the PCI procedure!


Two units of RBC
Covered stent 10 x 40 mm
Subsequent hospital stay uneventful
- No further bleeding,
- No signs or symptoms of ischemia
- PCI postponed due to the high bleeding risk
- Discharged under UFH therapy and the PCI was scheduled after 4 weeks.
Before PCI, started aspirin and clopidogrel 3 days before without pre-loading.
- January 2019: Re-admitted for PCI of the proximal LAD
Catheterization of the left main ostium with the EBU 3,5 6 French guiding catheter from the left femoral artery
How would you treat this LAD?
- Rotational atherectomy as a first strategy
- Balloon dilatation and atherectomy only if balloon fails
- Lithotripsy as a first strategy
- Lithotripsy after balloon dilatation
Advancement of a Pilot 50 0.014" wire

Wire exchange (Rotawire floppy) on micro-catheter → Rotablator (Rota-Pro®) with 1,5 mm burr
- Balloon dilatations with NC balloons 2.0 and 3.0 mm up to 18 atm
- Advancement of a ZES (Onyx) 3,5 x 18 mm,
- Post-dilatation with 4,0 x 15 mm NC balloon a 16 atm
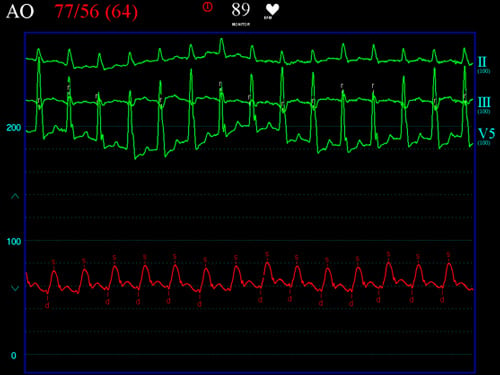
The complex PCI on the proximal LAD caused sustained hypotension during RA that was well tolerated due to the previous removal of the LV outflow tract obstruction → Enhanced safety by treating the AVS before…
Final angiographic result
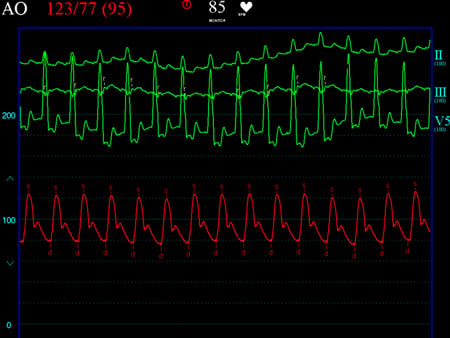
Good recovery of blood pressure
Discharge
Triple therapy: ASA + Clopidogrel + clexane 6000 UI x 2 for one month → Abdominal surgery after 1 month without peri-operative complications
Final comments
Triple therapy: ASA + Clopidogrel + clexane 6000 UI in hospital after surgery.
Before discharge, heparin was substituted by Warfarin and clopidogrel was stopped when a therapeutic INR was reached.
This case is an example of a complex clinical, surgical and interventional management accomplished with success under the coordination of the heart team.
The issue of PCI AFTER TAVI remains a very debatable one. As previously discussed, in our center this is the option of choice to enhance safety, but some difficulties to catheterize the coronaries might be encountered until adequate training is achieved.
"Thank you very much for all your comments and suggestions.
Needless to say that there is no scientific evidence to support our strategy, but neither to support any other alternative one!
Indeed, there is absolutely no conclusive data related to the use of rotational atherectomy (RA) before TAVI, or after the valve implantation.
In our experience, RA has always been performed AFTER the valve implantation (as in the case presented here) because we believe that it is safer to address a complex PCI in a severely calcified CAD once the severe AS has been removed, so that the hemodynamic reserve in case of complications or prolonged ischemia is better preserved. Indeed, the presence of a severe AS (in particular if the LVEF is compromised) may precipitate catastrophic hemodynamic crush in case of complications, an eventuality that can have fatal consequences in these complex pathophysiologic context.
Our experience with RA in TAVI patients has been recently published, and we are pleased to share our open access PDF with the Euro4C followers.
Until scientific data becomes available, common sense and experience will guide this decision and we look forward to seeing cases like this in our Euro4C website, (including those without a happy end…) because we can all learn from each other’s experience, and this is in the DNA of EuroPCR and the Euro4C."
Flavio Ribichini for Euro4C








10 comments
In this particular case I would perform TAVI and then PCI in the same procedure. Lesion on LAD si highly calcific and very tight, so I think I would prepare the lesion by RA with 1.25 burr (6 Fr. guiding catheter), then upgrading to 1.50 mm burr if necessary. I think PCI should be IVUS-guided
I am not sure at all if it is better to start with the TAVI or the PCI. Regarding the PCI, I think is a nice case for RA with 6F starting with 1.25 mm and continue with a 1.5 mm burr. Although it would also might be done directly with 1.5 mm, this patient may have a limited tolerance to any complication and probably I would select a progressive approach, NC or cutting balloon after the RA and finishing with a 3.5 x 18 mm DES, guided by IVUS in case of doubt with the sizing. I would have ready a bolus of noradreanaline to maintain the blood pressure in case of need.
Maybe better PCI first, because of potential challenges of left main engagement after valve implantation. TAVI could be performed at the same procedure in order to reduce delays for the further oncologic surgery
I would have staged the TAVI and begun with cautious Rota on the prox LAD. »Cautious« means that starting with 1,25 burr, as the filiform lesions seems to be at the very edge of the vessel. After 1,25 Rota, I would have inspected the vessel for further strategy: more Rota with a bigger burr or ballooning and stenting.
perform PCI and defer TAVI
Excellent case where we can debate the optimal PCI timing in TAVI patients. We know that about 60% of TAVI patients have significant angiographic stenosis and the vast majority of them affect proximal segments, being a very frequent decision in our daily practice. In my opinion, we would perform first TAVI and then PCI, probably in a deferred procedure. I would attempt the lesion with an AR guiding catheter and a 1.25 burr, always guided with IVUS-imaging.
Excellent case where we can debate the optimal PCI timing in TAVI patients. We know that about 60% of TAVI patients have significant angiographic stenosis and the vast majority of them affect proximal segments, being a very frequent decision in our daily practice. In my opinion, we would perform first TAVI and then PCI, probably in a deferred procedure. I would attempt the lesion with RA and a 1.25 burr, always guided with IVUS-imaging.
1. PCI and TAVI in the same hospital stay 2. As I am not experienced in TAVI procudres I would probably opted to preform PCI and than defer TAVI for few days - to my knowledge PCI after TAVI may be more challenging 3. Reason to perform PCI and TAVI during the same hospital stay - to decrease the delay to oncological treatment 3. LAD is big - stent at least 3.5mm - therefore at least burr 1.5mm 4. to prevent complications (mainly slow-flow) - short runs 5. when only remember to perform short runs - usually no flow complications expected 6. As transfemoral procedure contraindicated - rota with 1.5mm burr transradially 5. If bigger burr necessary - still feasible in this case - when only 6F EBU guding catheter used (such guding catheter curve allows to upsize the burr to even 1.75mm) 6. other option - patient is male - try to use 7F guding catheter transradially - often feasible (sometimes with the support of 5F diagnostic catheter as a rail) 7. cutting balloon/score balloons on the shelf 8. low threshold to use IVUS - but usually - careful lesion preparation with stent posdilatation allows to expect good result 9. new generation DES - with allowed 1 month DAPT
Congratulations. Really nice result despite the vascular complication. Probably in this case the treatment of the AE before the PCI helped to tolerate the hypotension during the PCI, but also the low cardiac output state during the severe bleeding might have cause serious ischemia in the presence of the lesion in the LAD, besides the difficulties to find the left coronary ostium after the TAVI. It is clear that we need more data regarding the timing of both procedures.
Very difficult case, congratulations for the great result! In such cases, the desision which procedure to perform first should be based on patient's clinical presentation, imaging and TAVI valve choice. I don't believe that extrapolating your desision to all TAVI- PCI cases is the right aproach. We had patients who developed CAD years after TAVI, and the catheter engagement proved to be extremely difficult, in one case we had to perform Rota with the RCA guiding catheter far away from the ostium and outside the valve cage, which was a nightmare. Sometimes, other parameters may influence your desision. In Greece, the coronary angiogram is usually performed weeks before the TAVI implantation approval from the Central Health Council (I know it sounds silly). Now, imagine a patient with unstable angina in the cath lab with severe AS and severe CAD, having to tell him or her (including yourself) that you will defer treatment. For all these reasons, I believe that the answer to what to do first is complicated. With that in mind, once again, congratulations!