25 Jul 2019
Step-by-step decision planning on how to deal with a «simple surgical case», but a potentially troublesome PCI lesion
This is the case of an 84 year old man, widower, with initial cognitive decay, living with his sons and daugthers - non autonomous but physically robust. He was admitted for chest pain at rest after weeks of worsening angina, and underwent coronary angiography within 48h of hospital admission
- Minimum troponin rise
- Normal LV ejection fraction
- CKD class II (creatinine 1.56)
Author
When you have to treat a coronary lesion that worries you….
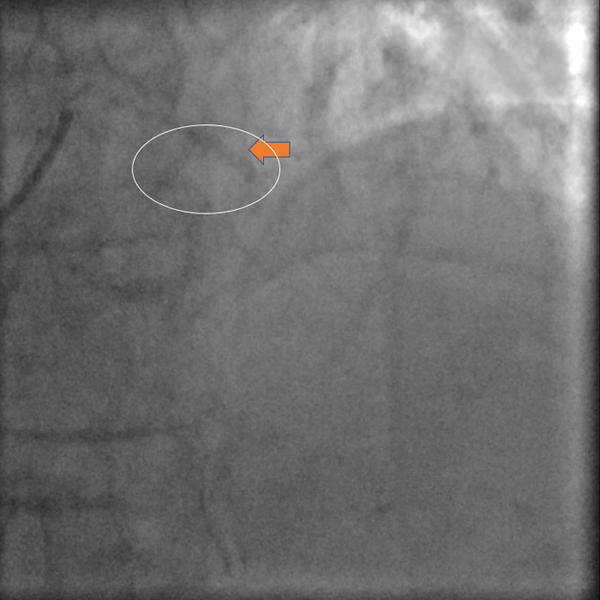
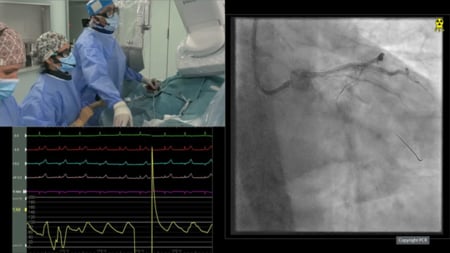
This still frame shows: Tight stenosis of a large LAD at the mid segment, a massive calcification of the LAD territory also distant to the vessel lumen, moderate/severe tortuosity : the lesion has a 90°bend
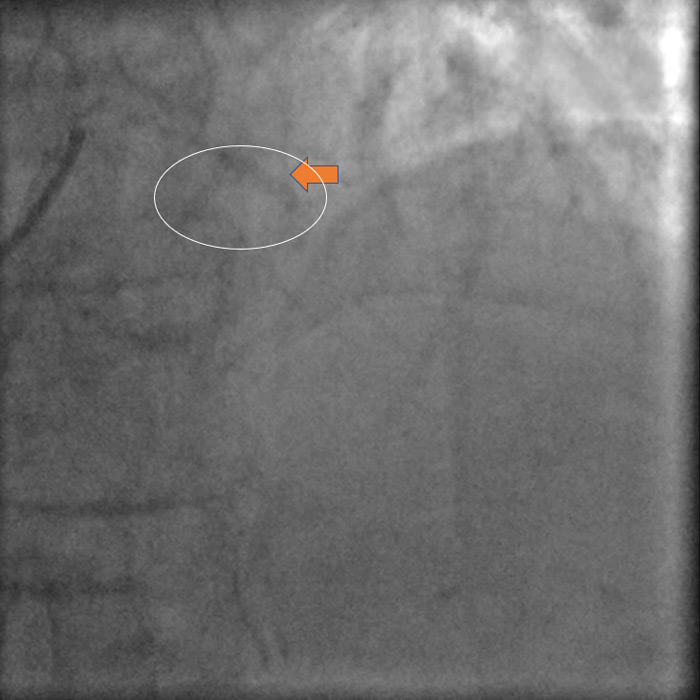
This still frame shows: The vessel calcification extends from the proximal to the distal part of the LAD. The tortuosity beyond the stenosis is <90°
Would I treat this patient with surgery or PCI?
- Single vessel disease
- Good LV function
- No diabetes
- Cognitive decay
- SYNTAX score: 12
- SYNTAX II
- PCI
SYNTAX Score II: 33.2
PCI 4 Year Mortality: 8.8 % - CABG
SYNTAX Score II: 41.5
CABG 4 Year Mortality: 16.9 % - Treatment recommendation: CABG or PCI
- PCI
Balloon angioplasty or Rotational Atherectomy
Why Rotational Atherectomy (RA) in this case?
- Probably the ONLY option to cross the lesion
- Effective for stenosis dilatation
- Essential for stent expansion
- Protective against diagonal branch occlusion
Furthermore…
- Balloon may not expand
- Balloon may occlude the diagonal branch
- Lithotrispy balloon may not cross the stenosis
But…
Warnings about RA in this case!
- High risk of bur entrapment
- High risk of severe dissection
- Moderate risk of vessel rupture
- Difficult stenting even after RA
We decided to proceed with PCI basically because of three reasons:
- patient's age
- the risk of further intellectual impairment after cardiac surgery
- the agreement of the heart team and the patient’s family to proceed with the minimally invasive option.
Procedural planning
- Preventive hydration
- Effective surgical stand-by
- Radial access
- No Mechanical Circulatory Support
- DAPT with clopidogrel and ASA
A first attempt was performed with balloon, to avoid the use of RA, but the balloon did not expand
- No severe dissection was apparent
- Plan B was rotational atherectomy
- A possible alternative was a lithotripsy balloon
A microcatheter was used to exchange the regular 0.014» wire for a 0.009» ES rotawire
RA was preferred over a lithotripsy balloon because of the lower cost, and the perception that this kind of balloon may not cross the lesion.
The protection wire in the diagonal branch is removed before RA.
A 1.25mm bur was selected and used with patience. Indeed, the bur crossed the lesion after 12 minutes and 8 run attempts, the last at 180.000rpm
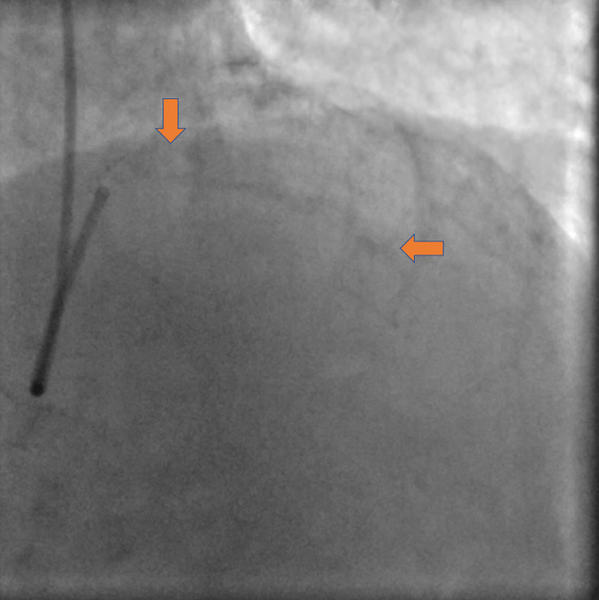
Angiography after RA.
- The LAD vessel is patent, the flow is normal
- The diagonal branch is unchanged
- No images of spasm or dissections
- The stenosis appear relieved
- The patient is stable and pain free
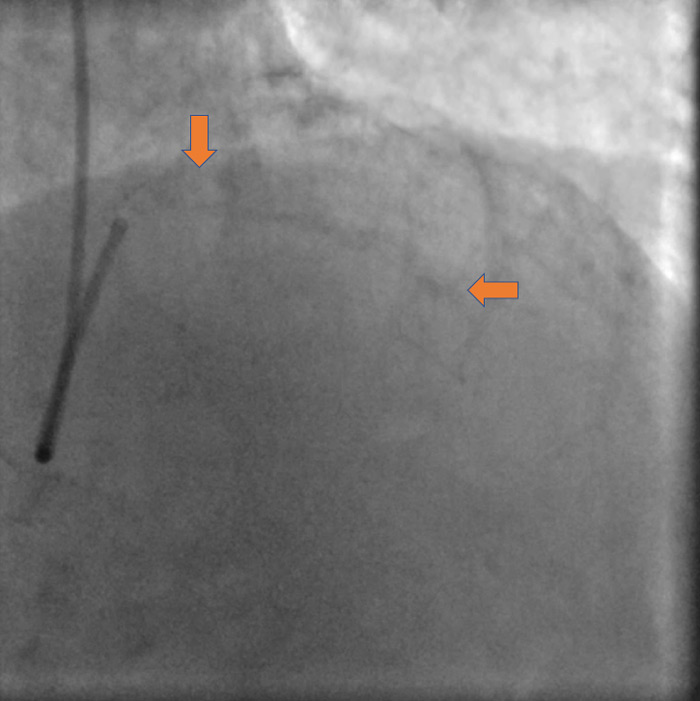
After RA a protection wire is reinserted in the diagonal branch and both NC balloons dilated properly
Final result with good angiographic expansion of the stent, good flow in the diagonal branch without new stenosis and the appearence of a dynamic stenosis of the distal LAD after removal of the critical stenosis and administration of NTG.
Outcome and follow-up
- There were no post-procedural complications
- The total amount of contrast was 120ml
- The patient was discharged 48h later
- DAPT was advised for a minimum of 6 months
- No clinical recurrences at follow-up (available at 6 months)
Key messages
- Maximize safety and efficacy
- Prepare the lesion for optimal stenting conditions
- Minimize contrast medium volume
There are different ways to do the same thing… But planning before starting a complex procedure is ESSENTIAL. Planning means also having a plan B and C in case A does not work!
"Thank you very much for your comments and suggestions, we are glad to see the enthusiasm that a case like one we face in our everyday practice rises among our community; furthermore, the exchange of opinions is the easiest way to open our minds to new ideas.
Basically the case we wanted to share would have been an ideal one for an off-pump single LIMA on LAD in centers with experienced cardiac surgeons. The choice of PCI is certainly “less conventional” given the risky features of the lesion that require experience with the use of RA to prevent complications and obtain a good result.
Of note, the agreement regarding the preference for the good old Clopidogrel in a rather stable CAD, the consideration of no need for hemodynamic support given the normal LV function and single vessel disease, but the preference for having on-site surgical back up in an elective case, with a challenging coronary anatomy, despite the low SYNTAX score, that often underestimates the peri-operative risk in calcified patients. Interesting to see also the growth of the radial access for complex cases treated with RA!.
It is obvious that there are many ways to do the job. The one we presented is the way we are confident with. Good planning based on a simplified strategy and experience with the use of RA are key and this is what we wanted to share.
We are all interested in knowing more about new technologies to treat calcified lesions, such as lithotripsy and orbital atherectomy, but clinical experience is limited so far. However, follow our Euro4C cases because much more is to come, including cases with these fascinating devices.
Our next case is what sometimes could turn into a nightmare when an apparently “straightforward primary PCI” cannot be reperfused because of a nasty calcified lesion, and again… a trained team and good technique may easily solve the problem in this emergency setting."
Flavio Ribichini for Euro4C





20 comments
Good support is essential in this case. Rotablator is a problem due to wire bias . Dissection and even perforation is probable. I would dilate with non compliance ballons if it cross and after this shock wave.Looks safer to.me. Ticagrelor is the muy choice
IMHO, the most probable complication is a wire bias and a building of a 2nd channel parallel to the artery with "exit" in the 1st curve and "re-entry" in the true lumen at the 2nd curve with consecutive risk of perforation. Implantation of a stent with relatively low pressure without agressive postdilation can be enough to achieve an acceptable angiographic result. But we should be ready to deal with rupture of the artery close to a very big 1st diagonal and may be to sacrifice the D1 and cover the perforation with a graft. By the way, this scenario is possible with rotablation and lithoplasty as well. I would start with 1.25 burr over floppy wire and check the path and position of the rotawire. In case of intraluminal (and not paravasal) path of the wire i would proceed with 1.5 and than predilate and stent. I would perform the procedure without circularory support (why?), but after breafing with my nurses about pericardial drainage set and grafts. And I would start through ldTRA
its interesting how the calcium does not follow the course of the vessel. Imaging is essential in these cases anyway
Great case to discuss. I would treat this lesion with upfront RA. I agree with other comments that correct wiring is crucial and would definitely use a workhorse wire over a micro-catheter and exchange for a Rotawire. Also agree that wire bias is a concern and would discuss about using an Extra-Support Rotawire (never used in my practice so far). Vascular access is not a concern but I would use a 7F guide or a 7.5 sheathless guide from the radial. Would keep the procedure as simple as possibile with a provisional strategy (although calcific, the diagonal does not appear to be stenotic).
Great case. Not to be attempted without rotablation. Yes wire bias is an issue but there are some tips in order to overcome the extreme tortuosity: 1) floppy rotawire (either directly or exchange with a microcatheter is up to the operator's discretion) trying to leave the wire as loose as possible and not to push it very hard in order to avoid wire bias 2) rotablation with 1.25 mm burr. This is a focal lesion and sometimes even touching the lesion with the burr may alter the compliance. Try not to advance the rotaburr far beyond the lesion 3) Very bendy vessel means low rpm. Not exceed 140000rpm in order to avoid complications I am pretty sure that once the burr passes through there will be no need for further rota. Just follow the routine PCI procedure afterwardas, Thank you, Petros Dardas
Very interesting case. The vessel is bending, the lesion is highly calcific and very tight. Actually my PCI strategy would be to maximize my support: 7Fr. femoral approach, very supportive guiding catheter and guidewire. I think I would start my PCI with conventional SC/NC balloons pre-dilation and if it works then I would upgrade to cutting/lithotripsy balloons, as vessel bends increase vessel perforation risk with RA. In my opinion, lithotripsy as first PCI option isn't a good idea as it wouldn't cross the lesion.
Great case, Flavio. Thank you for sharing it with us. For this massively calcified, very tight, and angulated LAD lesion, I would certainly prepare the lesion before trying to dilate. I would choose the RA in first intention, and my strategy would be the following: 1/ Prepare the patient with a loading dose of TICAGRELOR upfront the procedure 2/ Place, through radial approach (if feasible) a 7 Fr extra back up guiding catheter to get an excellent support. 3/ I would not use any mechanical support for such a case, considering the good LV function, but I would try to ensure a good arterial pressure all along the procedure with drugs if necessary 4/ Then I would advance a performant 0.014 guidewire, down in the LAD and exchange with a microcatheter for a FLOPPY ROTAWIRE 5/ Start RA with a small 1.25 mm BURR, pecking the lesion several times before crossing with the BURR, to avoid to trap it 6/ I would exchange the ROTAWIRE for a 0.014 guidewire, again using a microcatheter (as the presence of a dissection after RA is highly probable) and predilate with a NC 3.0 balloon, after protecting the DIAGONAL with a standard 0.014 guidewire. Then I would finish the PCI of this LAD-DIAGONAL bifurcation using the T provisional technique. If the NC balloon does not expend properly, I would use a lithotripsy balloon in bail-out.
This abifurcational lesion so need 2wires LAD floppy Wire because of torousity Use RA for LAD lesion and put stent in LAD lesion with balloon in in the big D1 to the LAD this for good position of LAD stent and if D1 become jeopardized we can crush the LAD stent by D1 balloon.
Nice challenging case. Although the risk of perforation is a possibility, I believe that a stepwise approach with 1.25 and 1.5 mm RA is feasible. I would start with a Whisper or Sion wire and a Caravell, changing later with a floppy rotawire. After finishing the atherectomy I would protect the diagonal, despite the risk of losing the branch may be considered very low. Afterwards I would use a 2.5 mm cutting or scoring balloon and deploy a 2.5 x 15 mm Xicence Sierra stent, performing postdilatation of the segment of the stent proximal to the bifurcation depending on the diameter by IVUS, presumably with a 3.5 x 10 NC balloon. The decision about the stent is based on the disparity among the diameter of the LAD proximal and distal to the bifurcation and the excellent capability of that stent to reach larger diameters. I don´t think that a mechanical support would add anything to this case and I would choose radial approach. Clopidogrel would be my first choice and I would try not to increase the volume of contrast with OCT given the age and the creatinine clearance.
what about CX stenoses?
The calcification is far from the lesion, so I start with pre-dilatation by a small and then a NC sized balloons, if the balloon fully opened and the result is good, I will put a long stent begin before the diagonal branch until the last LAD curve and finished by post dilatation.
I full agree with the strategy as suggested by Didier Carrie although I would choose a 7 Fr femoral approach upfront. Great case!
I full agree with the strategy as suggested by Didier Carrie although I would choose a 7 Fr femoral approach upfront. Great case!
Well done, Flavio, and especially well described and discussed. Congrats!
Great Case I would have upgraded the but size upto 1.5mm after 1.225 as it's 3.5 mm vessel , for better Stent expansion
Great Case I would have upgraded the but size upto 1.5mm after 1.225 as it's 3.5 mm vessel , for better Stent expansion
Great learning case. I would have upgraded but size to 1.5mm followed by 2.75mm cutting balloon predilatation and then deploying the stent
Great learning Case I would have upgraded the bur size upto 1.5mm after 1.25mm as it's 3.5 mm vessel , for better Stent expansion. I would have predilated the lesion with 2.75 mm cutting balloon afterRA
It was a good case from decision making till the end
great case I would surely do imaging as it also gives idea about the wire bias if wire bias favourable than RA or else IVL