20 Jun 2019
Defining together a treatment strategy for calcified CAD in a patient with multivessel disease
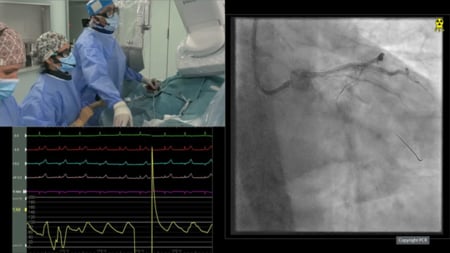
This is the case of a 68 year old female patient, autonomous and physically robust. She has been diabetic for 10 years, but without cardio-vascular antecedents. She was admitted for chest pain at rest, lasting around 70 minutes with signs of STEMI in the inferior leads and extensive anterior ST depression. She underwent coronary angiography with 40 minutes in-hospital delay.
Author
Let’s exchange opinions on this case. This could happen to you tomorrow…
Would I treat this patient with surgery or PCI?
- Single vessel disease
- Good LV function
- Diabetic
- Normal renal function
- SYNTAX score: 25
- SYNTAX II
- PCI
SYNTAX Score II: 34.7
PCI 4 Year Mortality: 9.9% - CABG
SYNTAX Score II: 21.1
CABG 4 Year Mortality: 3.3%
Treatment recommendation: CABG
- PCI
Balloon angioplasty or Rotational Atherectomy
Why Rotational Atherectomy (RA)?
- Effective for stenosis dilatation
- Essential for stent expansion
- Protective against side branch occlusion
Furthermore…
- Balloon may not expand
- Balloon may occlude the septal and diagonal branches
- Lithotripsy balloon may not cross
Warnings about RA
- Long lesion
- Diffuse disease
- Relatively small vessel
↓
Risk of dissection and low flow
- Impaired contractility of the inferior wall
↓
prepare to prevent hypotension
What would be your first choice to treat the lesion?
- I would use rotational atherectomy as a first option
- I would use balloon first and rotational atherectomy if balloon does not expand
- I would use a lithotripsy balloon
Procedural planning
- Complete revasc before discharge
- Preventive hydration
- Effective surgical stand-by
- Radial access
- No mechanical circulatory support
- DAPT with Ticagrelor and ASA
Question: What to do with an undilatable lesion?
- Stent and try to expand with NC balloons → NO!!!!!
- Use cutting balloon → ???
The options are two-fold:
- Use a lithotripsy balloon → But there is little clinical evidence to support this option at this stage
- Use rotational atherectomy → large experience with this device
Final angiographic result
Follow-up
- No peri-procedural complications (stable creatinine level)
- Total amount if contrast media: 90ml
- DAPT was advised for 12 months
- Discharged 48 hours post PCI
- One year follow-up available, without recurrences
“Thank you for your comments on this case!
This was the first of a series of cases that we would like to share to exchange ideas and opinions.
Interestingly, in this specific case, clinical scores were in favor of surgery as the “best” therapeutic option, but both the clinical and angiographic presentation appeared to be reasonable also for PCI, a decision that very likely most cardiologists would support.
The key message of this case was to show how a lesion that may appear to be straightforward for balloon PCI may prevent a good preparation for stenting. The case is quite a simple one showing the usefulness of RA before stenting to achieve a good result.
In the upcoming months we will share other cases with growing complexity, with the intention of sharing our experience and hearing alternative ideas. This will give the experts the opportunity to share their tips, and those interested in gaining experience, a great occasion to learn from real-life cases and from the experience of their older companions.
Enjoy the case, and let us know you thoughts.”
Flavio Ribichini for Euro4C






20 comments
We have only one view of the left system ! Seeing this I would choose a radial approach, 6 Fr Guiding, 1.5 Rota. After this PTCA and Stenting of the LAD
I think intravascular imaging with IVUS may give a clue whether to start with rotational atherectomy directly (270 degree calcification or more) or going step by step with 1:1 NC balloon +/- scoring or cutting balloons followed by lithotripsy balloon if still non dilatable. We can also notice that the RCA appears heavily calcified , so I wonder if we can extrapolate the data we have from the behaviour of RCA lesion into the LAD one ( balloon dilatable) . Thanks alot
I think intravascular imaging may give insight about the degree of calcification which will impact our strategy whether to go directly for rotational atherectomy (270 degree or more) or going step by step with 1:1 N.C +/- scoring or cutting balloons with a room for lithotripsy balloon. We can also appreciate that the RCA lesion has to some extent similar degree of calcification angiographically, so I wonder if we can extrapolate the behaviour of the RCA lesion (Balloon dilatable) into the LAD one if we don't have imaging on table. Thanks alot.
Although the procedure might be approached both with balloon angioplasty or rotational atherectomy, my first choice would be the second one, mainly due to the large septal branch with severe stenosis in its origin. A 1.5 mm burr with a 6F catheter through radial access may prepare the two lesions properly and probably I would continue with 2 inflations of a 2.5 x 15 mm balloon, followed by a 2.5 x 28 mm DES. I would take the decission about final postdilatation depending on the residual stenosis. Let see with the second part if the operator chose the same approach...
Left system appear to be be calcified.probably severity of calcification of left system is better appreciated in RCA views. Spotty calcification is seen at least in views provided. I would try to predilate LAD lesion with a 2mm NC balloon and see for presence of nondilatable waist . In case of latter I would proceed with rotablation with a 1.5 mm burr. Imaging would provide an idea but I feel with lesion severity in pLAD, imaging catheter may not cross the lesion and my threshold of upfront imaging in this case would be rather high in this case. I would use it at end of procedure to verify stent expansion & apposition.
After treatment of the culprit lesion the Syntax Score is about 17 for two LAD lesions, so, definitely PCI. Both lesions looks not severely calcified, but Rotablation with at least 1.5 burr (or may be 1.75) can be helpful to preserve side branches - the 1st diagonal and the 1st septal. Summarizing: 6F, ldTRA, primary rota with 1.5 burr, predilatation 1:1 with nc balloons, DES
Nice case, thanks for sharing. I believe at least one more projection of the left system is essential before decision. First choice elective PCI, radial access, 6Fr, balloon +/- rota 1.25. If PCI not feasible then minimal invasive CAB.
Radial, imaging with OCT. If unable to pass OCT then 1.25burr and the OCT to determine thickness of calcium., length and arc which will help to determine id IVL necessary. Good case, thanks for sharing.
Lesion on LAD is tight and highly calcified, so I wouldn't start PCI with conventional balloon. I think Rotational Atherectomy could be a better option in this case for two reasons: 1) lesion on proximal LAD is severe and lithotripsy balloon couldn't be able to cross 2) lesion on LAD is long and lithotripsy balloon is only 12 mm; actually only one balloon couldn't be enough, and using several lithotripsy balloons the procedure could be very expensive
RAC is treated - collaterals are less important now (but are good for opposite direction) Would go for balloon first: if it does nor cross, does not expand, would go for rota: lesion is to tight for direct IVL
Great case, thanks Flavio. Culprit lesion is treated. LAD seems to have a challenging anatomy, though I cannot see a lot of calcium from the angio provided (I can have a sense of it looking at the RCA angio where I can a shadow of calcium on the LAD, there is lot of calcium in the aorta). First, I would stage this procedure after having cooling off a bit the acute clinical condition. I would then bring the patient back a start with balloon PCI first. If there is any concern with balloon crossing or with expanding, I would not hesitate to rotablate. Alternatively, imaging might be also an option, even if I am not sure that IVUS or even OCT would easily cross these 2 tight lesions. This would then bring us back to a balloon predil and to my initial reasoning. Looking forward the way you treated!
Angiographically doesn't seem so calcified. NC-Balloon first, bailout Rota 1.25 mm. After this, IVUS for better long-term result & stent-expansion.
A real-life case Flavio. I will also treat the culprit lesion and stage the second procedure (but treating it before discharge) As there are two bends in LAD with calcium and some tortuosity and IVUS/OCT catheters will not progress I will approach directly with rotablation instead of ballooning. I guess it is a more controlled scenario. Maybe a step-up approach with a 1.25 mm burr and next 1.5 o 1.75 depending on the angio (plus nitro) images. Next, OCT or IVUS imaging if available and surely a 2.5x28/32 mm DES with a final POT in the proximal part.
Great case! LAD not so heavily calcified and in RCA good result without RA - I would try LAD with a balloon (but not nc balloon) keeping in mind a very low treshold for RA . What does it mean? Low pressure (6-8 atm) sc balloon - if not fully expanded - switch to RA. Why sc? The bigger the pressure, the bigger the risk of dissection. Small dissection is not a problem for consecutive RA, but if a big dissection occurs - in case of a nondilatable lesion we put our patient at a big risk of troubles. It is better to be on a safe side. Radial approach, 6F Guide, OCT after ballon expantion/1.5 burr successful passage.
Great Case. Angiographically RCA stent Looks underexpanded. If RCA stent is really Underexpanded, It May require IVL for further stent expansion and better apposition. LAD lesion looks highly calcifoed. For LAD lesion I will use Upfront Rotational athetrctomy with 1.5mm Burr followed by 1:1 NC balloon dilatation for Plaque Modification and better Stent expansion. I will do it by using Radial approach 6F,EBU guide.
Nice result of the case. Congratulations. You are right that the worse scenario might be to deploy the stent without having prepared the lesión adequately. Last time we did it in our lab we need 3 additional procedures in the following 3 years to get the desired result. The only thing I would have done differently in this case would have been to cover the entire lesión with a long stent of 28 mm.
Excellent description of the case. Makes you think you about the options every step and then showed us how they treated the patient. Instructive case, thoroughly enjoyed it.
Many thanks. Pure rotablation technique: start with 1.25 mm burr as a default at low speed up to 140000rpm, use bigger burr only if needed, avoid complications, excellent result
Personally, I would start from the very beginning with rota, 1.5 burr (1.25 has the potential to be stacked while trying to retrieve), and then predil. with NC balloons, and finally the aim is to implant only one stent, in order to avoid gaps or overlaping. Anyway, great job, congtrats.
Very good case from real life. Thank you for sharing. Distal TR approach; 6F EBU 3.5 First step: I would try to dilatation LAD lesion with a 2.25-2.5 mm compliant ballon (beware of ballon rupture). If unsuccessful as in this case then the Second step: I would introduce a second wire into the LAD and repeat angioplasty with NC ballon 2.0 - 2.25mm. like the cutting ballon. If failure again then the Third stage: i would use a burr.