07 Mar 2025
Navigating LAA closure in retrobend chicken-wing anatomy
In collaboration with the European Left Atrial Appendage Closure Club
A 76-year-old female patient with a history of atrial fibrillation and contraindication to long-term anticoagulation presents for left atrial appendage closure. However, preprocedural imaging reveals a challenging retrobend chicken-wing morphology. What is the best technique to optimize positioning and ensure safe, effective closure in this scenario?
Authors
Clinical presentation
- 76-year-old female
- Permanent AF
- Spontaneous intracerebral cortical bleeding under rivaroxaban 20 mg
- Multiple microbleeds on MRI
- HTA/Diabetes
- Ischemic heart disease with previous DES on the mid-LAD
- Normal renal function
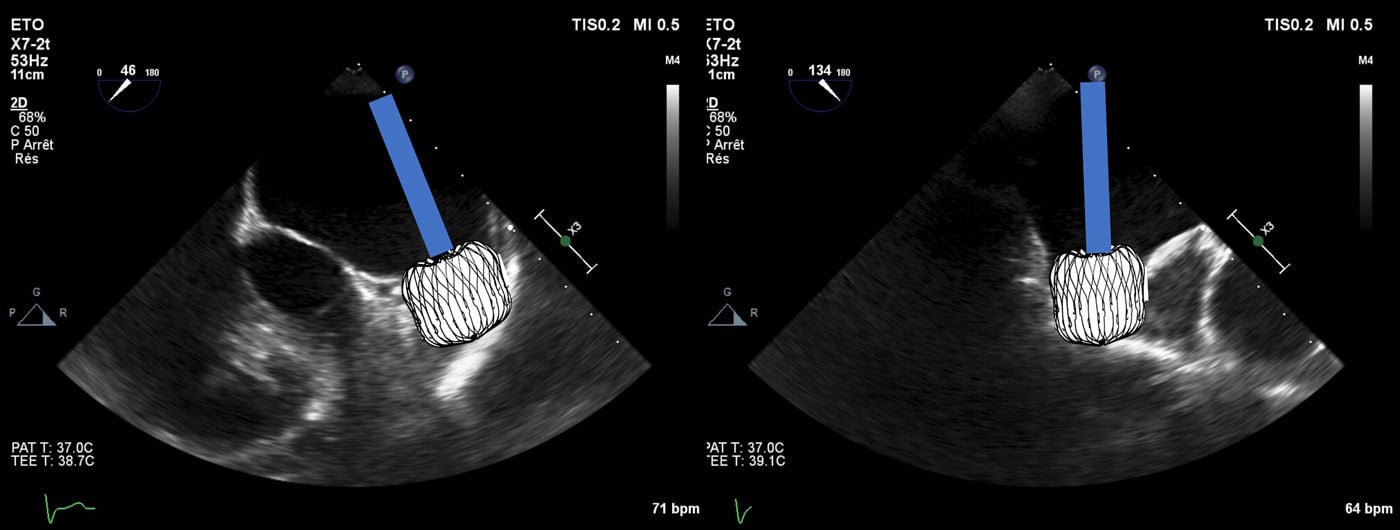
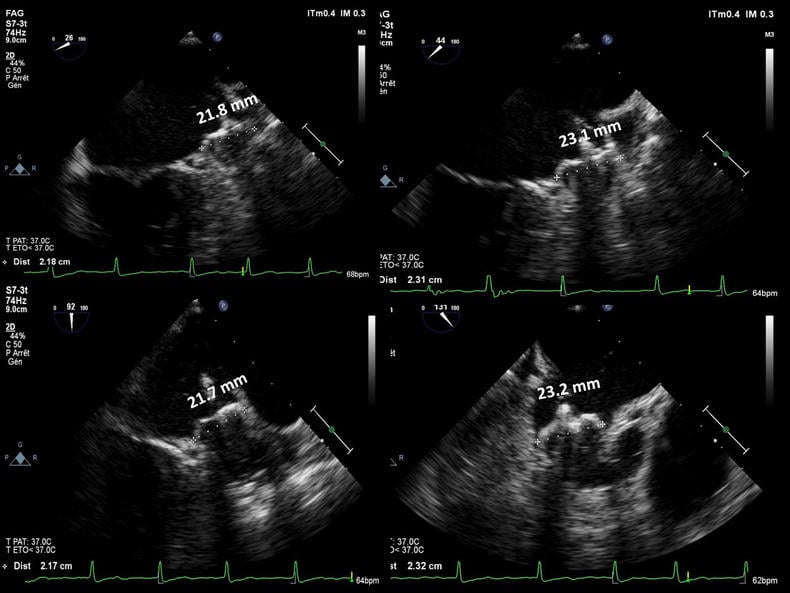
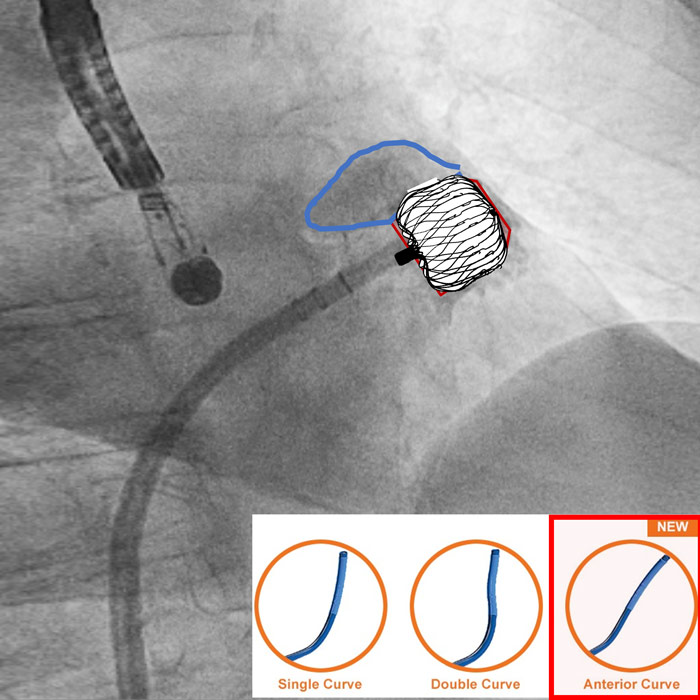
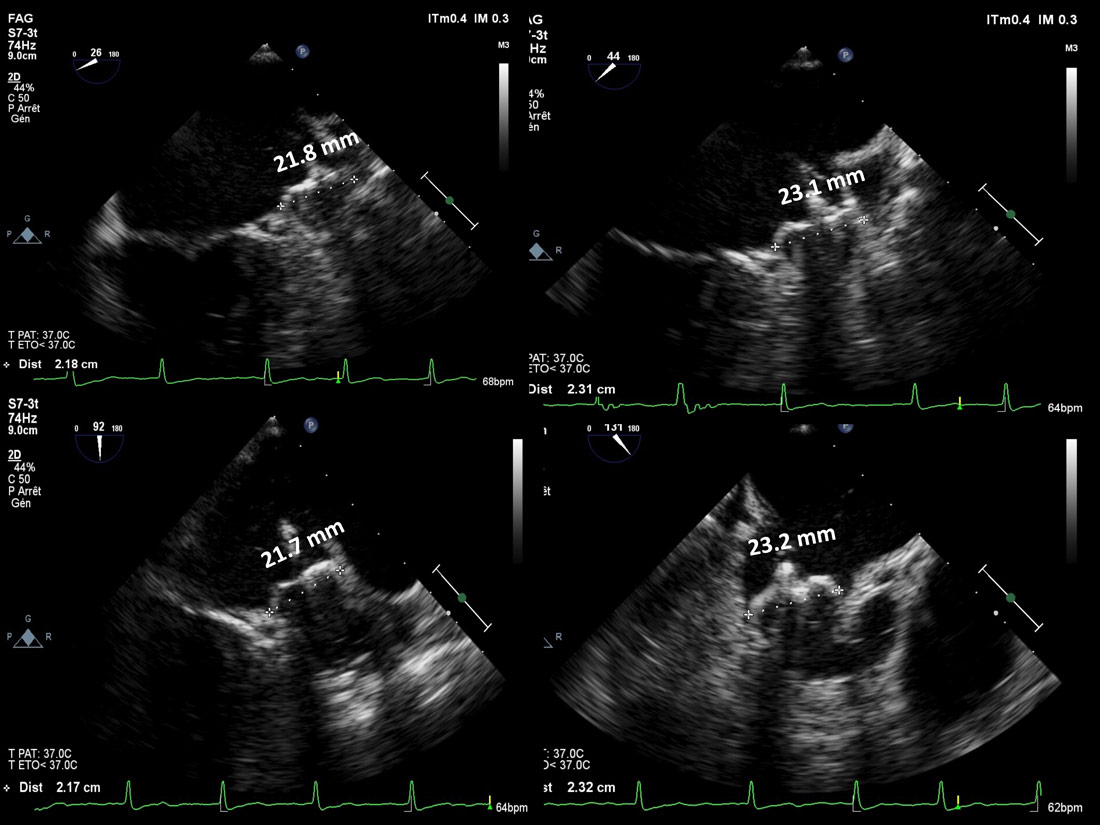
Preprocedural TEE: Retrobend Chicken-Wing!
Watchman Flx and retrobend CW: Basic implantation principles
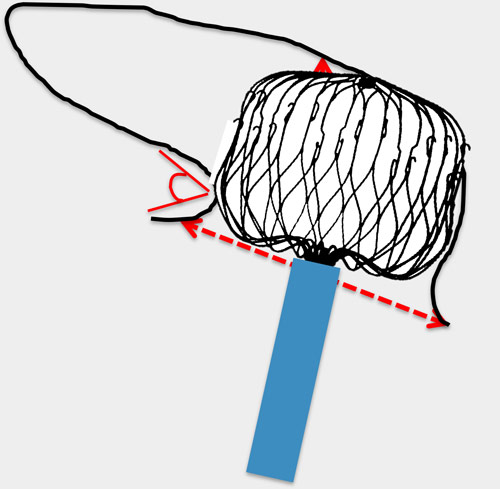
WM Flx should be placed in a shallow area and not beyond the bend!
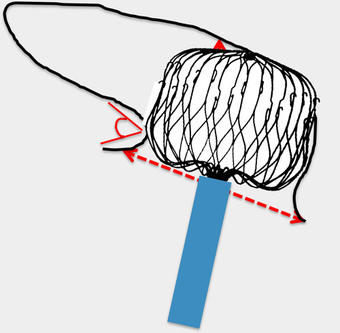
« Working » depth ≥ ostium
Technically feasible
Sizing is of utmost importance!
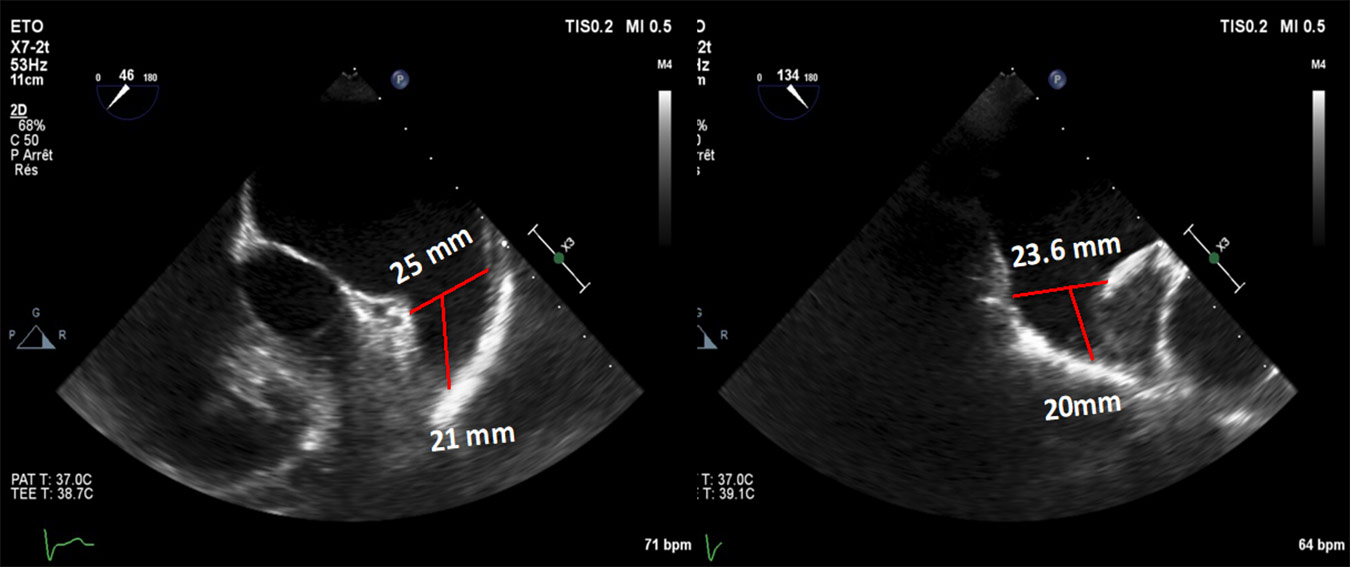
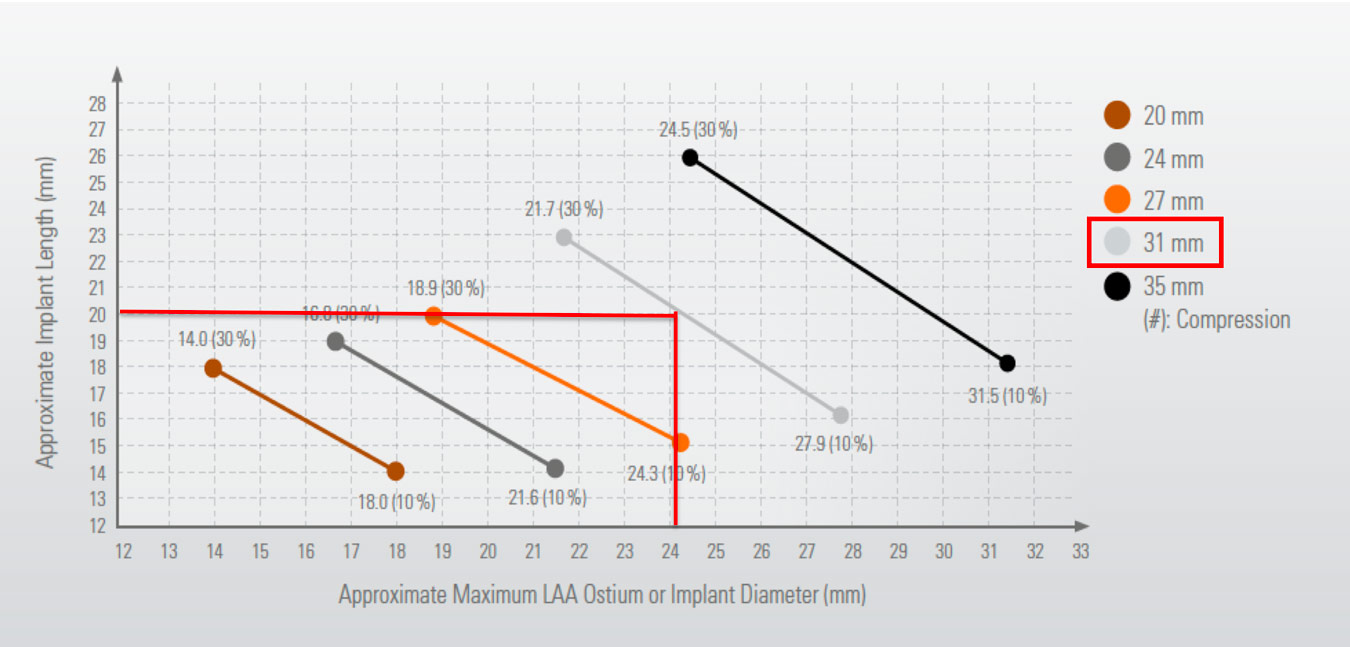
WM Flx LZ 23.6/25 mm
Working depth 20-21 mm
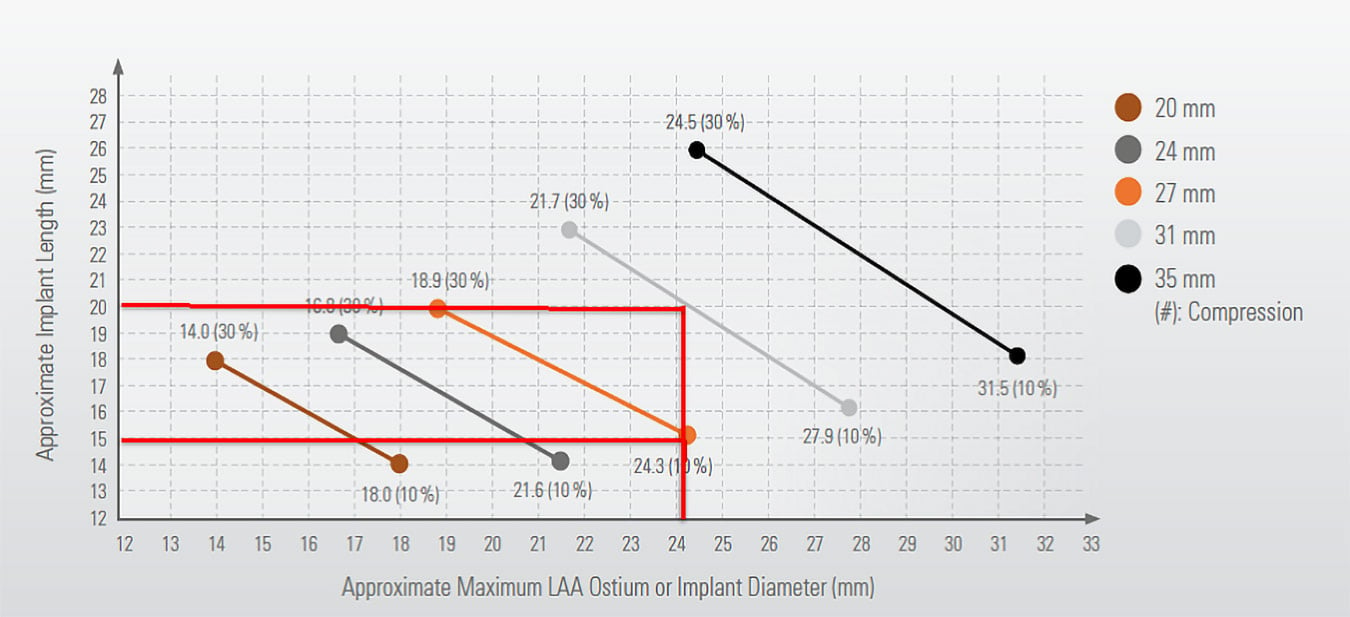
Determine proper device selection!
- Wm Flx 27 mm?
- Expected compression 10%
- Working depth needed 15 mm
- Wm Flx 31 mm?
- Expected compression ~20%
- Working depth needed = 20 mm
Device selection: Watchman Flx 31 mm
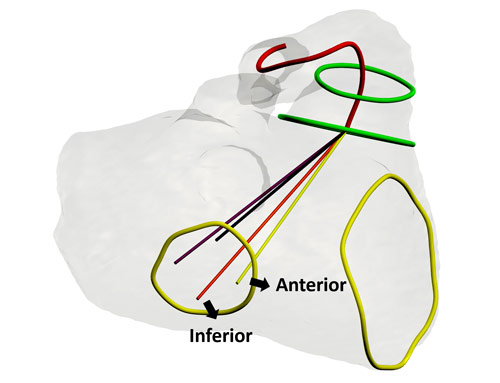
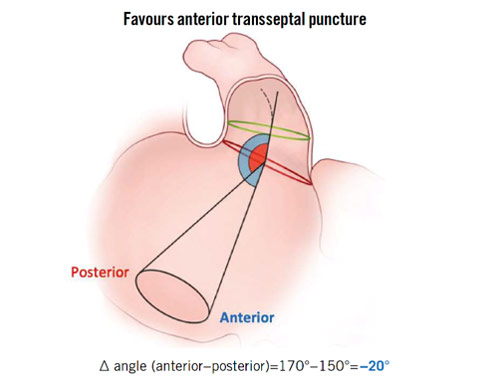
Retrobend CW: Tailored TSP inferior and mid-anterior > improved co-axial alignment
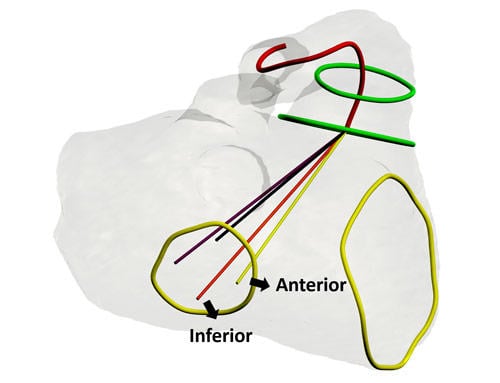
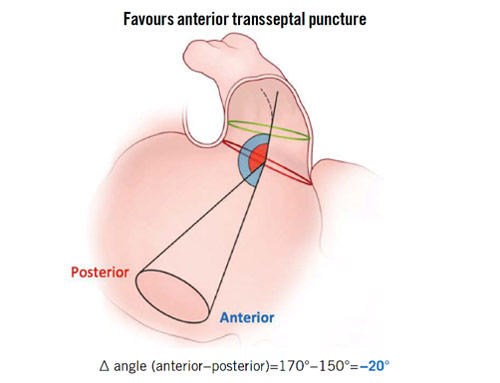
Source: Fukotomi M et al. Eurointervention 2022
Target implantation area
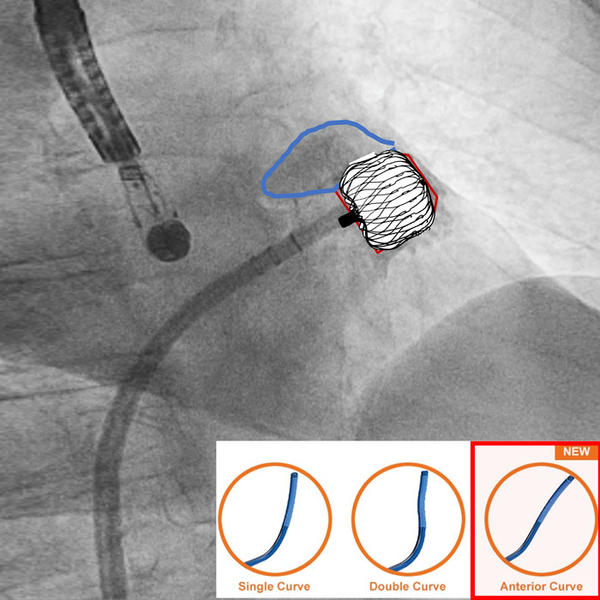
Flx ball- Mix between push and retrieval technique (goal= keep adequate implantation depth!)
28 minutes procedure, 30 CC of contrast
30% maximal compression, 25% minimal compression
30% maximal compression
25% minimal compression







4 comments
I think a 27 mm Watchman FLX could be the correct device size, but proper stability testing with a robust tug test is mandatory. In my experience, for retrobend chicken-wing anatomies, a mid-anterior TSP may be a better choice than a posterior one
Flx 31 mm. Positioning the delivery system deep and working in unsheat.
31 mm
The most challenging anatomy we have to face... still hesitating about the most appropriate device in this setting, we've had issues with both designs, but a sandwich technique with a lobe-and-disc device might be preferred... In any case, transeptal puncture (TSP) must be inferior and anterior. In the event of using a Watchman FLX as suggested, achieving a perfectly coaxial position can be very tricky, but an off-axis implant would lead to a proximally protruding inferior shoulder and an "over-the-fabric" leak. Therefore, a correct TSP is key. I'd choose a 31 mm device in this case.